-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(7): 524-528
doi:10.5923/j.ajmms.20211107.05
Received: Jun. 16, 2021; Accepted: Jul. 5, 2021; Published: Jul. 15, 2021

Evaluation of Sacubitril Efficiency in the Treatment of Acute Decompensation of Cardiac Insufficiency
K. K. Gulyamova
Republican Research Center of Emergency Medicine, Tashkent, Uzbekistan
Correspondence to: K. K. Gulyamova, Republican Research Center of Emergency Medicine, Tashkent, Uzbekistan.
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

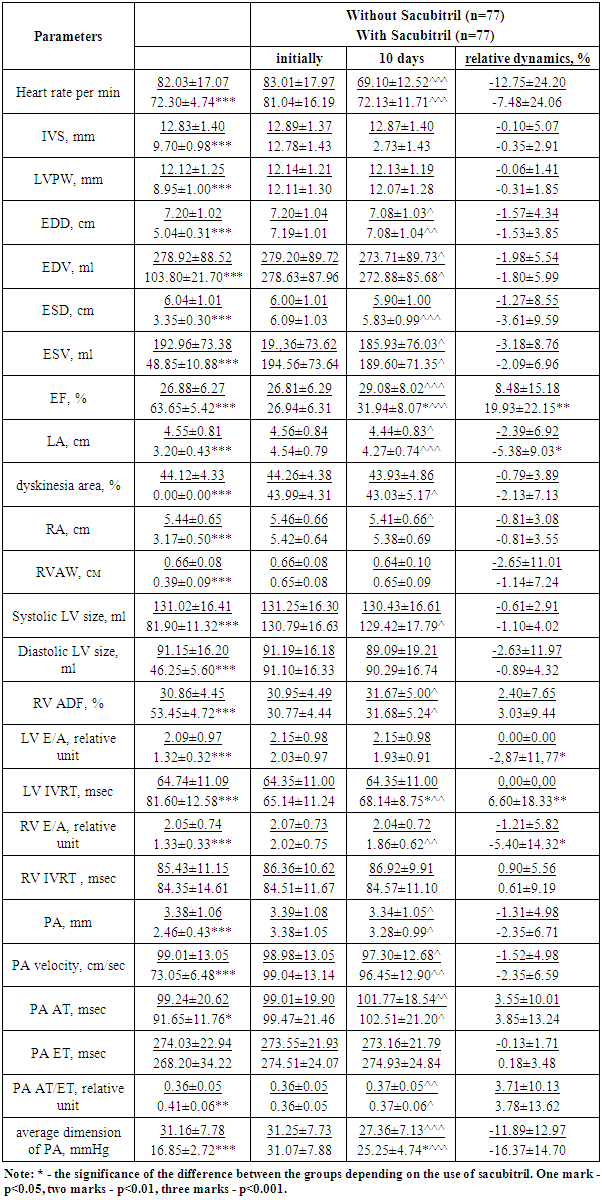
Aim of theresearch was to study the effect of Sacubitril introduction in the therapy of patients with acute decompensation of heart failure. Material and methods. The study included 138 patients with chronic heart failure who were hospitalized to the Republican Research Center of Emergency Medicine due to the development of acute decompensation of heart failure. All patients were performed an echocardiographic examination and were prescribed therapy aimed at compensating of heart failure. During the study all patients were divided into 2 therapeutic groups: in group C+ (69 patients), Sacubitril – a neprilysin inhibitor in combination with valsartan (Uperio) was added to the therapy regimen, in group C- only standard therapy was used. The control examination was performed on the 10th-14th day of therapy, including echocardiography. Results. In the group of patients taking Sacubitril, there was a significantly greater decrease in the right ventricular E/A ratio (-5.40% vs. -1.21%, p<0.05), a decrease in the size of the left atrium (-5.38% vs. -2.39%, p<0.05) and an increase in the left ventricular ejection fraction (19.93% vs. 8.48%, p<0.01). As a result, by the end of the hospitalization period, significantly higher left ventricular ejection fraction (31.94±8.07% vs. 29.08±8.02%, p<0.05), duration of isovolumic relaxation time of the left ventricle (68.14±8.75 msec vs. 64.35±11.00, p<0.05), lower values of the average pressure in the pulmonary artery system (25.25±4.74 mmHg vs. 27.36±7.13 mmHg, p<0.05) were achieved in the group C+ in compare with the patients who did not take a neprilysin inhibitor. Conclusion. The present study found that in the intensive care of acute decompensation of heart failure in the period of hospitalization (10 days), the introduction of Sacubitril into the therapy regimen can increase the positive effect of treatment, contributing to the improvement of central and pulmonary hemodynamics.
Keywords: Acute decompensation of heart failure, Sacubitril, Echocardiography, Pulmonary hemodynamics
Cite this paper: K. K. Gulyamova, Evaluation of Sacubitril Efficiency in the Treatment of Acute Decompensation of Cardiac Insufficiency, American Journal of Medicine and Medical Sciences, Vol. 11 No. 7, 2021, pp. 524-528. doi: 10.5923/j.ajmms.20211107.05.
1. Introduction
- Chronic heart failure (CHF) is one of the most important socio-economic problems in the world due to high mortality and disability of the population. The number of patients with CHF in the world, despite the intensive search for new treatments, steadily grows [1-3]. About 5 million Americans suffer from CHF, 550 thousand new cases are detected annually [4]. The prevalence of CHF in the European population ranges from 0.4% to 2.0% [5]. In Russia, according to the results of the EPOCHA-O-CHF study, decompensation of CHF caused hospitalization in hospitals with cardiology departments in almost every second patient (49%), and CHF appeared in the diagnosis in 92% of those hospitalized in such clinics; the one-year mortality of patients with clinically evident CHF reaches 26-29% [6-8]. The treatment strategy of CHF is based on the effect on the pathogenetic links of the pathology progression and includes inhibition activity of the sympathoadrenal and renin-angiotensin-aldosterone system activity. In the case of acute decompensation of heart failure (ADHF), drugs that reduce preload – diuretics and peripheral vasodilators - are introduced to the treatment. Recent studies have revealed an important role in inhibiting the CHF progression of the natriuretic peptide system, and the activation of this system by Sacubitril, which inhibits neprilysin, is already reasonably recommended for use at CHF with reduced left ventricular (LV) systolic function. However, the effects of Sacubitril at the ADHF and the feasibility of its use in an acute situation remain unclear. Aim of the research was to study the effect of Sacubitril introduction in the therapy of patients with acute decompensation of heart failure.
2. Material and Methods
- The study included 138 patients with chronic heart failure who were hospitalized to the Republican Research Center of Emergency Medicine due to the development of acute decompensation of heart failure (ADHF). The mean age of the patients made up 66.02±10.41 years. There were 94 (68.12%) men in the cohort of the studied patients. Etiologically, in all patients included in the study, CHF was associated with CHD. The clinical form of CHD was angina pectoris. In the anamnesis, 84 (60.87%) patients had a myocardial infarction, including 33 (23.91%) patients with more than once, 26 patients (18.84%) underwent surgical revascularization, 44 (31.88%) patients were performed endovascular revascularization. The duration of CHD was on average 13.27±2.87 years, CHF – 5.87±2.16 years. Verification of the diagnosis was based on documentary data (extracts from the medical records of previous hospitalizations).As a control group, the study included 20 healthy volunteers of the appropriate age, who did not have signs of the cardiovascular system lesion, including those of a vegetative nature. The criteria for non-inclusion in the study were valvular and congenital heart defects, cardiac arrhythmias in the form of sinus node weakness syndrome, atrial flutter and fibrillation, high and III degree of atrioventricular block, and other variants of atrioventricular dissociation. In addition, the study did not include patients with acute infectious and febrile diseases, endocrinological pathology, malignant neoplasms, chronic organ failure requiring constant therapy, anemia with a hemoglobin level below 100 g/l.Hypertension was the background pathology in 128 (92.75%) patients.At the time of hospitalization, all patients were taking drugs aimed at correcting CHF and arterial hypertension: beta-blockers – 113 (81.88%) patients, angiotensin-converting enzyme inhibitors – 62 (44.93%) patients, angiotensin II receptor blockers – 48 (34.78%) people, spironolactone – 63 (45.65%) people, eplerenone – 12 (8.70%) people, torasemide – 33 (23.91%) patients, furosemide – 68 (49.28%) patients, cardiac glycosides – 96 (69.57%) patients.All patients included in the study were examined during hospitalization, aimed at determining the structural and functional state of the left and right parts of the heart, as well as the features of pulmonary blood flow. The study examined the dependence of cardiovascular status on LV systolic function. All patients were prescribed therapy aimed at compensating of heart failure: carvedilol, valsartan, torasemide 20 mg / day, spironolactone 200 mg / day, antiplatelet therapy, antiarrhythmic therapy (amiodarone) in the presence of ventricular arrhythmias. During the study all patients were divided into 2 therapeutic groups: in group C+ (69 patients), Sacubitril – a neprilysin inhibitor in combination with valsartan (Uperio) was added to the therapy regimen, in group C- only standard therapy was used The control examination was performed on the 10th-14th day of therapy, including echocardiography.Echocardiographic examination of the heart was performed on a scanner "Siemens Sonoline Omnia" (Germany) using a multi-frequency sensor 2-4 Mhz in one-dimensional (M), two-dimensional (B) modes and in the Doppler echocardiography mode (using pulse and constant wave spectral Doppler, as well as color Doppler mapping of blood flow). Echocardiography was performed at rest, lying on the back. All measurements were carried out for at least three cardiac cycles and then averaged.Measuring the length of the asinergic region and the length of the endocardial surface of the myocardium in the “long axis” and “four chambers " projections, the area of the myocardial lesion was determined as a percentage of the total LV surface (%Sac).MEchoCG (from the left parasternal access along the long axis of the left ventricle): the End-systolic volume (ESV) and the End diastolic volume (EDV) of the left ventricle, the Left ventricular posterior wall thickness (LVPWT) and the interventricular septum (IVS), the thickness of the free wall of the right ventricle in systole and diastole.2MEchoCG (from the apical access in the projection of the 4-chamber section): end systolic volume and end diastolic volume of the left ventricle. The volume of the left ventricle was calculated by the "area-length" method using the formula V=8A2/3πL, where V – left ventricle volume (EDV or ESV). The impact volume (IV), ejection fraction (EF), right ventricular volume, and right atrium size were calculated by the planimetric method using the “area-length” method. The systolic function of the RV was evaluated by the degree of reduction of its area in the systole (area decrease fraction (ADF) of the RV).DEchoCG:1. The study of pulmonary flow was carried out from the left parasternal access in cross-section at the level of the aortic valve at the position of the control volume between the leaflets of the pulmonary artery valve. The maximum velocity of systolic pulmonary flow (Vmax) and the diameter of the pulmonary artery were determined; the acceleration time (AT) of systolic flow in the outflow tract of the RV, corresponding to the interval from the beginning of the flow to the peak of the velocity; the time of blood expulsion from the RV (ET), corresponding to the interval from the beginning of the systolic flow in the RVoutflow tract to its end. The average pressure in the pulmonary artery was determined by the value of the AT / ET ratio of the ejection flow on the pulmonary artery valve.2. The study of the transmitral flow was carried out from the apical access in a 4-chamber section at the position of the control volume between the leaflets of the mitral valve. We determined the followings: maximum rate of early peak diastolic filling (Vmax Peak E); maximum rate of transmitral blood flow during left atrial systole (Vmax Peak А); the ratio of the maximum rates of early and late filling of E/A; isovolumic relaxation time of the left ventricle – IVRT. 3. The study of the transtricuspid flow was carried out from the apical access in a 4-chamber section at the position of the control volume between the leaflets of the tricuspid valve. The following parameters were calculated: the maximum rate of early (E) and late (A) diastolic RV filling, as well as their ratio (E/A), isovolumic relaxation time (IVRT).All the data obtained were entered in summary tables with the distribution of patients into groups. Arithmetic averages and standard deviation were calculated for each group. Intergroup differences were evaluated using the Student's test for 2 comparisons. The frequency differences were determined using the chi square tabular criterion and evaluating its reliability from the tables taking into account the number of freedom degrees.
3. Results and Discussion
- The examination of patients hospitalized due to ADHF revealed a significant increase in heart rate (p<0.001), despite the use of beta-blockers as part of continuous therapy (113 (81.88%) patients) which indicates a pronounced activation of the sympatho-adrenal system (SAS) (Tab. 1).
|
4. Conclusions
- Our study found that in the conditions of intensive therapy of ADHF in the period of hospitalization (10 days), the introduction of Sacubitril into the therapy regimen can increase the positive effect of treatment, contributing to the improvement of central and pulmonary hemodynamics.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML