-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(7): 518-523
doi:10.5923/j.ajmms.20211107.04
Received: Jun. 20, 2021; Accepted: Jun. 30, 2021; Published: Jul. 15, 2021

Place of Vasopressin in Demarcation of Interstitial Ectopic Pregnancies During Laparoscopic Resection
Samarawickrama N. G. C. L.
Senior Registrar, Professorial Obstetrics and Gynecology Unit, Colombo South Teaching Hospital, Colombo, Sri Lanka
Correspondence to: Samarawickrama N. G. C. L., Senior Registrar, Professorial Obstetrics and Gynecology Unit, Colombo South Teaching Hospital, Colombo, Sri Lanka.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Diagnosis and management of interstitial ectopic pregnancy is challenging. Resistance of decidual vessels to vasopressin when compared to rest of the uterine vasculature taken into consideration in laparoscopic excision of interstitial ectopic pregnancies to demarcate the margins and to minimize blood loss. Method: Case series of nine patients diagnosed with interstitial ectopic, who underwent laparoscopic surgery, were injected with diluted vasopressin to the myometrium prior to make the surgical resection. Results: The myometrial tissue turned pale in contrast to pink and vascular interstitial ectopic revealing a clear margin between the two tissues. Vasopressin injection significantly reduced the blood loss as oppose to procedure done without vasopressin. Conclusion: Injection of vasopressin in to the myometrium prior to resection of an interstitial ectopic pregnancy provides well-demarcated zones to aid complete laparoscopic resection while minimizing the blood loss.
Keywords: Interstitial ectopic, Vasopressin, Laparoscopic
Cite this paper: Samarawickrama N. G. C. L., Place of Vasopressin in Demarcation of Interstitial Ectopic Pregnancies During Laparoscopic Resection, American Journal of Medicine and Medical Sciences, Vol. 11 No. 7, 2021, pp. 518-523. doi: 10.5923/j.ajmms.20211107.04.
1. Introduction
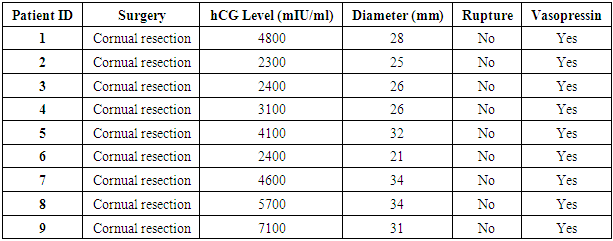
- When the conception implanted outside the uterine cavity it is referred to as an ectopic pregnancy regardless of the site of implantation [1]. The incidence of an ectopic pregnancy is 11 per 1000 pregnancies at present and it is being in increasing trend over the recent years [1,2]. Even though majority of these women does not carry any risk factors, tubal damages due to infections, pelvic surgeries, smoking and artificial reproductive techniques are direct contributory factors for these abnormal implantations. Fallopian tubes are the commonest site for abnormal implantations, which accountable for 95% of extra uterine pregnancies and among these, 80% are in the ampulla region of the tube [3]. Trans vaginal scan is the diagnostic tool of choice in diagnosing an ectopic pregnancy, with the sensitivity of 87 to 99% and specificity of 94 to 99% [1] in the light of clinical and biochemical findings. When an ectopic pregnancy implanted in the interstitial part of the tube, this abnormal implantation is referred to as an interstitial ectopic, with the incidence of 1% to 6% [1]. This part of the fallopian tube is about 1 to 2 cm in length and is encircled by a thin layer of myometrium. Three- dimensional ultrasonography will increase the sensitivity of detecting an interstitial ectopic pregnancy when compared to the conventional two- dimensional ultrasonography [1]. Comparatively interstitial ectopic pregnancies are associated with higher morbidity and mortality due to its inherent difficulty in the diagnosis, which leads to delayed diagnosis with higher chance of uterine rupture and subsequent significant life-threatening hemorrhage. The established criterion in diagnosing an interstitial ectopic pregnancy includes (1) Empty uterine cavity (2) Laterally placed gestational sac surrounded by less than 5 mm myometrial tissues (3) Presence of “interstitial line sign” [1] (Figure 1). It has been noted that rather delayed risk for rupture due to the presence of myometrial covering, interstitial ectopic pregnancies rupture in early gestations than expected [4].
 | Figure 1. Trans abdominal ultrasound image showing an interstitial pregnancy at 12 weeks and 5 days. Arrows indicate normal endometrium on the left and absent myometrium above the pregnancy |
2. Objectives
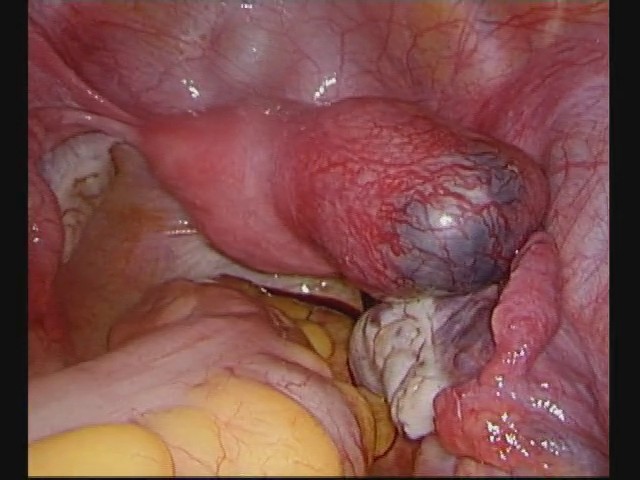
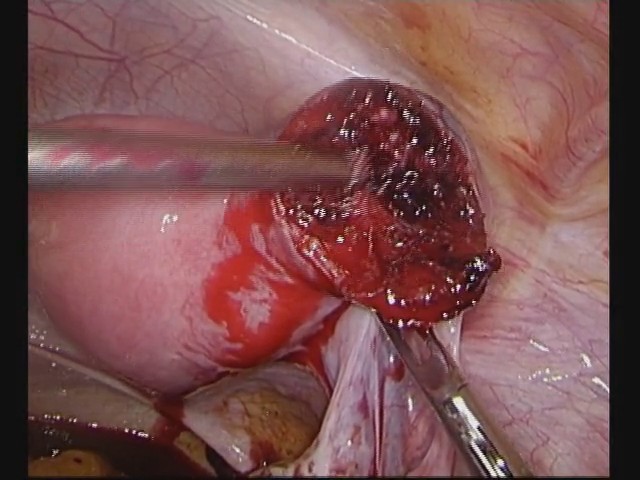
- Due to the anatomical site, interstitial ectopic pregnancies are associated with an increased risk of life-threatening hemorrhages following rupture as well as during surgical resections. Compared to open methods, laparoscopic approach associated with higher incidences of intra-operative hemorrhages, thus there are many techniques developed to minimize such bleeding. These include infiltration of diluted vasopressin to the normal uterine myometrium, electrocoagulation of resected area, multi-layered repair of surgical defect and ligation of ipsilateral uterine artery [8].In the literature of laparoscopic management of interstitial pregnancies, the use of diluted Vasopressin in view of minimizing the hemorrhage has being well established [8]. But it is important to highlight the fact that in certain interstitial ectopic pregnancies, it is not straightforward in demarcating these resection margins. As one of the premier centers for advanced laparoscopic surgeries in Sri Lanka, the Professorial Obstetrics and Gynecology unit attached to Colombo South Teaching Hospital, we looked into this fact more closely as it can improve both patient care as well as the training of postgraduate trainees. We have observed that in addition to minimizing the risk of intra-operative hemorrhages, injection of Vasopressin can be used as a method of demarcating the interstitial ectopic thus to perform more organized resection. Our objective in this article is to delineate the importance of proper demarcation by explaining the anatomical, molecular and receptor level interactions of vasopressin with uterine and trophoblastic tissues.Vasopressin - Mechanism of action Vasopressin is a typical neural hormone (Nona peptide) which secreted by the neural cells in the hypothalamus [9]. Its primary action is to enhance water re-absorption at the nephron levels in the kidney via the action at V2 receptor level. When the hormone acts on V1 receptor it activates the cascade of intracellular signal transduction via IP3 (Inositol Triphosphate) in the vascular smooth muscles thus cause vasoconstriction [10]. This effect is the basis for injecting vasopressin to the uterine myometrium to minimize bleeding during procedures such as myomectomy and cornual resection of interstitial ectopic pregnancy. As mentioned previously, for the action of vasopressin, presence of vascular smooth muscle is an essential factor. Therefore, this knowledge can be utilized in view of demarcating the gestational trophoblastic tissues from the uterine myometrium.Myometrium, Placenta and Fetomaternal interface – The difference in the vasculatureBy the beginning of the 3rd week, the trophoblasts are characterized by the presence of primary villi, that consist of cytotrophoblast core covered by a syncytial layer [3]. During further development, mesodermal cells penetrate the core of the primary villi and grow towards the decidua thus form the secondary villi. By the end of third week, mesodermal cells in the core of the villus begin to differentiate in to blood vessels and small blood cells and therefore differentiate into a tertiary villus. During further trophoblastic differentiation along with trophoblastic invasion of terminal branches of maternal spiral arteries, hybrid vessels containing both fetal and maternal cells are replaced by an endothelium. To accomplish this process, cytotrophoblast cells undergo an epithelial to endothelial transition, along with transformation of decidual spiral arteries from small-caliber resistance vessels to large, capacitate, low resistance vessels, which lack smooth muscle coat [3,11]. Absence of smooth muscle cells allows these vascular lakes to be resistant to vasoconstrictor substances such as vasopressin thus maintain constant supply of adequate amount of blood to the growing fetus. This is the chemistry behind well demarcation of interstitial ectopic pregnancy following vasopressin injection into the myometrium. This knowledge can be applied for the comprehensive resection of interstitial ectopic pregnancy along with proper repair of uterine defect. Additionally, this type of approach can reduce the incidence of uterine ruptures during subsequent pregnancies [12], a well- recognized complication of cornual resection and repair.
3. Our Experience
- In our unit as one of the premier centers for advanced laparoscopic surgeries in Sri Lanka, unless otherwise indicated, almost all ectopic pregnancies were managed via laparoscopic approach. Wide variety of surgical approaches have been utilized depend on the type and clinical presentation of the ectopic pregnancy. For the interstitial ectopic pregnancies, either cornual resection or cornuostomy and anatomical reconstruction are the preferred methods. Up to date our unit has the highest number of case reports with regard to laparoscopic management of interstitial ectopic pregnancies in Sri Lanka and all these cases are pre mapped by using vasopressin injection (Table 1). In the literature of cornual ectopic pregnancy, a technique of using highly diluted vasopressin (20 Units of vasopressin diluted in 1000 ml of normal saline and injected 150–250 ml below the interstitial pregnancy to achieve hemostasis during laparoscopic surgery has been described [13]. In our practice we inject 20 Units of vasopressin, which diluted in 200 ml of normal saline into the uterine myometrium. The aim of this technique is to achieve maximum trophoblastic to myometrial demarcation in addition to achieving bloodless field for the laparoscopic resection. Careful patient selection is an essential component as patients with certain medical conditions such as seizure disorders, migraine headache, asthma, cardiovascular or renal disease, heart failure, goiter with cardiac complications, arteriosclerosis, or fluid overload are not suitable for vasopressin injection [14].
|
4. Case Reports
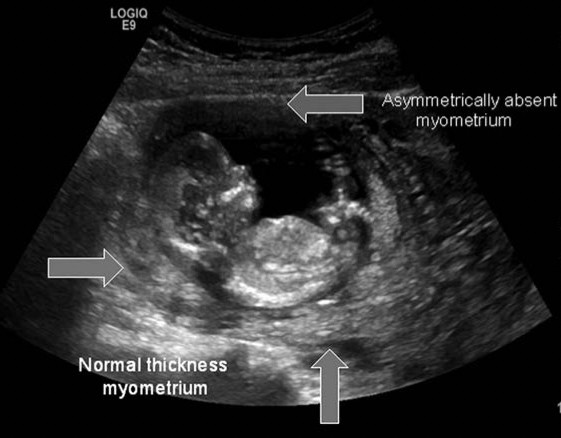
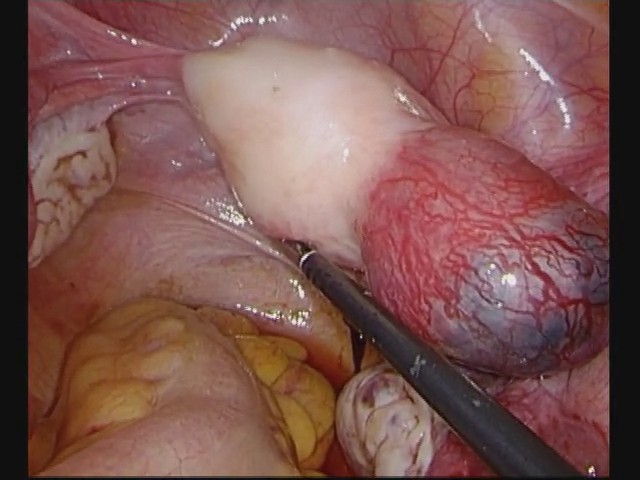
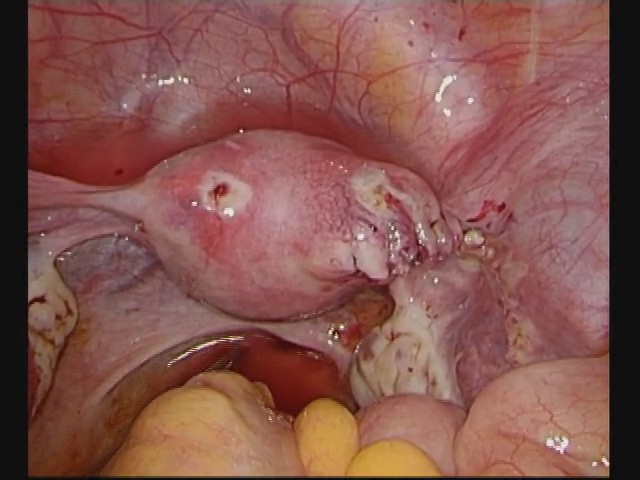
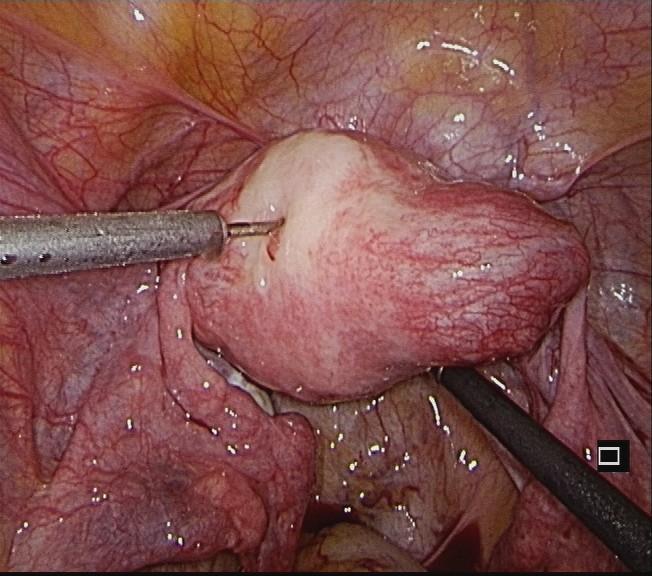
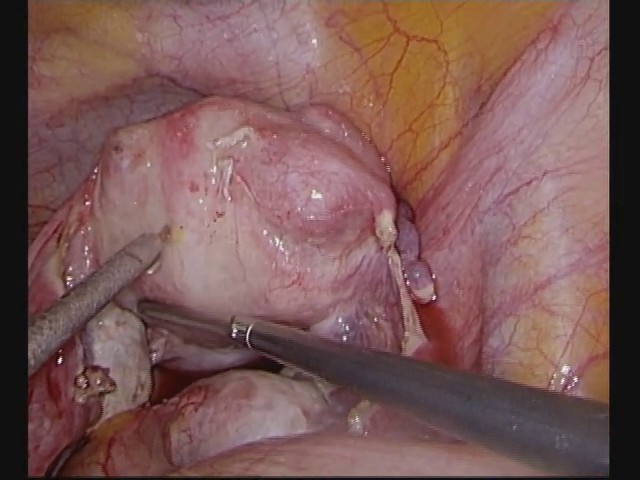
- The images shown below are of some patients who managed laparoscopically following vasopressin injection in Colombo South Teaching Hospital University Gynecology unit attached to University of Sri Jayewardenepura. The mean gestation age is nine weeks for this case series with mean gestational sac diameter of 38 mm.Case description 1A 31-year-old woman, G3P1C1 presented to the Gynecological ward of Colombo South Teaching Hospital with a history of period of amenorrhea. According to her last menstrual period, the estimated gestational age was ten weeks and four days. She complained of non-radiating, dull lower abdominal pain, which accompanied with bleeding per vagina. Her first pregnancy was in 2012, ended with vaginal delivery at term following Prostaglandin E2 induction and delivered a live male baby. The second pregnancy ended as a spontaneous miscarriage at six weeks of gestation in 2013 for which she underwent medical management.On general examination, patient was not pale. The pulse rate was 78 beats per minute and her blood pressure was 110/70 mmHg. The abdomen was not distended, and mild tenderness was elicited in the right iliac fossa with no guarding. Pelvic examination revealed normal external genitalia, closed cervix and positive cervical motion tenderness. The uterus was bulky, tender and examining finger was stained with blood.Patient had a positive urine pregnancy test. Trans vaginal 2 - dimensional ultrasound scan revealed an empty uterus with thickened endometrium of 12 millimeters. There was a circumscribed well- encapsulated mass measuring 39 x 41 mm, eccentrically positioned at the upper portion of the uterus away from the lateral edge of the uterine cavity with no fetal pole. No free fluid collection was demonstrated in the pouch of Douglas.The diagnosis of an ectopic pregnancy was made, and laparoscopic resection was planned. The intra operatively there was a clean abdomino-pelvic cavity with slightly bulky uterus. The right cornua was distended by a mass of 55 mm in length (Figure 2). Both ovaries and left tube were normal. Following vasopressin injection, normal uterine tissue became totally pale compared to the ectopic pregnancy with a distinct demarcation between the two regions (Figure 3). Patient underwent right Cornual resection and salpingectomy (Figure 4). The tissue defect was repaired laparoscopically by using 0 variable loop braided sutures (Figure 5). Histopathological evaluation of the specimen confirmed the diagnosis of an ectopic pregnancy. The postoperative period was uneventful, and the patient was discharged on day 2 post-operatively.
 | Figure 2. Laparoscopic view of large right interstitial ectopic pregnancy in case 1 |
 | Figure 3. Laparoscopic view of right interstitial ectopic pregnancy after injection of diluted vasopressin in case 1 |
 | Figure 4. Laparoscopic cornual resection after injection vasopressin in case 1 |
 | Figure 5. Laparoscopic cornual resection and repair of right interstitial ectopic pregnancy in case 1 |
 | Figure 6. Right interstitial ectopic pregnancy after injection of diluted vasopressin in case 2 |
 | Figure 7. Right interstitial ectopic pregnancy after injection of diluted vasopressin in case 3 |
5. Discussion
- Laparoscopic management of interstitial ectopic pregnancies has been described extensively in the literature [15,16]. Compared to other locations of ectopic pregnancies, presence of an interstitial ectopic pregnancy, carries a significantly increased risk of severe morbidity and mortality. This consist of intra-operative adverse outcomes including heavy and often life-threatening bleeding due to the challenging nature of these surgical procedures [8].Thus, findings successful methods to identify these pregnancies early and establishing ways to minimize the risk associated with the procedure would improve overall surgical outcomes. The use of vasopressin injection to minimize the bleeding risk during resection of interstitial ectopic pregnancies has being described by many case series [8,13]. But in the same literature, we have observed that the use of Vasopressin for the demarcation of interstitial ectopic pregnancies has being seldom addressed. Due to the anatomical location of the interstitial ectopic, surgical management either open or laparoscopic is always challenging. Thus, proper demarcation of the gestational trophoblastic tissues from normal uterine tissues will provide excellent field of resection to the operator. As it has being described earlier, the difference between the vasculature provides the key to this explanation. Depend on the presence or absence of Vasopressin V1 receptors, the vasculature responds to the vasoactive Vasopressin. Since normal uterine vasculature consists of vessels that are capable of contracting in response to Vasopressin, it will become a distinctly pale zone. Therefore, this area stands as a well-demarcated area from gestational tissues, which remain in the normal tissue texture throughout.This demarcation of zones will provide better tissue resection plane during surgical management of the ectopic pregnancy not only for an experienced operator, for whom who are in the process of acquiring the experience and skills. Proper dissection provides optimal repair of the uterine defect thus minimize the risk of uterine rupture following subsequent pregnancies [12].These cases illustrate the degree of clarity in demarcation of interstitial ectopic pregnancies by injection of Vasopressin therefore will continue to be benefited to both individual patients as well as the health care system.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML