-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(7): 507-511
doi:10.5923/j.ajmms.20211107.01
Received: May 12, 2021; Accepted: Jun. 21, 2021; Published: Jul. 15, 2021

Improving Conservative Treatment of Chronic Moderate Purulent Otitis in Patients in the Postoperative Period
Nargiza Orzeuvna Xamrakulova, Nilufar Jurakulovna Khushvakova, Yulduz Nuriddinovna Isakova, Shaxboz Mexrodjevich Mexrodjev
Samarkand State Medical Institute, Uzbekistan
Correspondence to: Nargiza Orzeuvna Xamrakulova, Samarkand State Medical Institute, Uzbekistan.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article describes the methods of conservative treatment of chronic moderate purulent otitis in patients in the postoperative period. There are also scientific studies on the types and causes of chronic otitis media in patients. In addition, any ear infection is very dangerous and provides information on the symptoms of the disease and ways to treat them. In addition, conclusions and recommendations for the improvement of conservative treatment of chronic moderate purulent otitis in patients in the postoperative period were presented.
Keywords: Otitis, Inflammation of the ear, Acute form of otitis, Chronic moderate purulent otitis in patients, Severe pain in the ear, Eardrum, Spread to the skull
Cite this paper: Nargiza Orzeuvna Xamrakulova, Nilufar Jurakulovna Khushvakova, Yulduz Nuriddinovna Isakova, Shaxboz Mexrodjevich Mexrodjev, Improving Conservative Treatment of Chronic Moderate Purulent Otitis in Patients in the Postoperative Period, American Journal of Medicine and Medical Sciences, Vol. 11 No. 7, 2021, pp. 507-511. doi: 10.5923/j.ajmms.20211107.01.
1. Introduction
- According to statistics, 30% of all otorhinolaryngological diseases are acute forms of otitis. preschoolers are more likely than adults to develop the disease. eighty percent of children under the age of three have had otitis media at least once.Infection that cause inflammation of the hearing and otitis media [1]:Ø pneumococci;Ø streptococci;Ø staphylococci;Ø includes hemophilic rods and other microorganisms.Any ear infection is very dangerous and you should see a doctor if you have any symptoms (described below). Symptoms of moderate otitis media include [2]:Ø severe pain in the ear;Ø fever;Ø purulent discharge from the ear canal after 1-3 days.After the pus comes out, the patient's condition improves, the body temperature drops, and the pain is significantly reduced or eliminated. The pus comes out of a hole in the eardrum. this outcome of the disease is considered positive, and with proper treatment, the eardrum is gradually restored without affecting hearing. The negative development of the disease is dangerous because it is impossible for the pus to come out and the pus can spread into the skull. This otitis can cause meningitis as well as brain abscess. to prevent such dire consequences, consult an otolaryngologist for advice and treatment at the first signs of otitis. Classification of inflammation by location [3]:Ø external otitis;Ø otitis media;Ø internal otitis.Often, otitis externa develops in swimmers. inflammation is caused by damage to the outer ear canal or ear canal. Violation of the protective layer leads to the entry and proliferation of pathogenic microorganisms in the area, which then forms a boil. If left untreated, otitis externa can become severe and the inflammation can spread to the earlobes and bone. In such cases, the patient may experience symptoms such as severe throbbing pain, swelling of the ear, and a moderate rise in body temperature. In otitis media, the inflammatory process spreads to the airway cavity of the middle ear, which is located behind the tympanic membrane of the ear: the tympanic cavity, the ear canal, and the mastoid tumor. Otitis media often progresses from catarrhal to purulent. Acute catarrhal otitis of the middle ear can also form as a complication of arvi (inflammation), which occurs after the pathogen enters the eardrum cavity of the infection. In the early stages, hearing loss may be accompanied by noise in the ears, but the temperature may be normal or slightly elevated. If these symptoms are ignored, catarrhal otitis may develop further, with sudden onset of high fever and ear pain. The pain can then spread to the eyes, neck, throat or teeth. to treat such otitis, you only need to eliminate the infection, and for this you need to see a doctor immediately [4].Acute purulent otitis media is an advanced catarrhal form of the disease. the disease is accompanied by rupture of the tympanic membrane and the outflow of pus, followed by a decrease in body temperature. Treatment should include regular removal of pus from the ear, which can only be done by a doctor, while fighting the infection.Also, pus does not always come out on its own. If the eardrum is very strong, surgery may be needed to pierce it. this procedure is called “paracentesis” and is performed using local anesthesia: at the most convenient point, a hole is made with a special tool and the pus is completely removed. When the pus comes out, the eardrum is restored and the quality of hearing is not impaired [5]. If left untreated, otitis media can spread to the skull. as a result, otitis media develops, which affects the vestibular apparatus, leading to brain abscess and at least partial or complete hearing loss. So when the first signs of otitis are observed, you should see a doctor immediately without putting anything in the ear or putting a tampon with alcohol or other antiseptics.
2. Materials and Methods
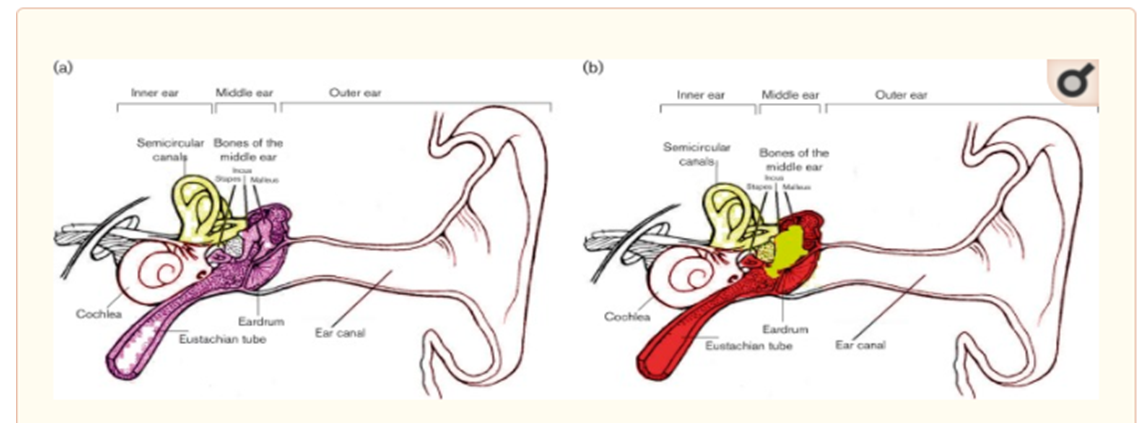
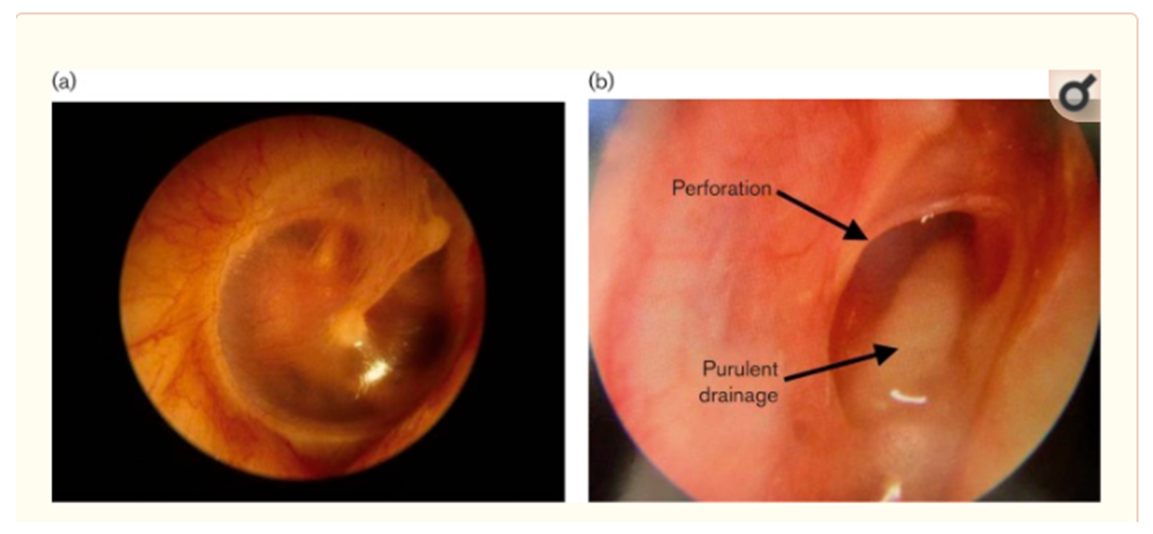
- When examined by otoscope, the middle ear looks red and inflamed with purulent discharge in CSOM patients (Figs 1 and 2). It is one of the most common chronic infectious diseases worldwide especially affecting children.
3. Results
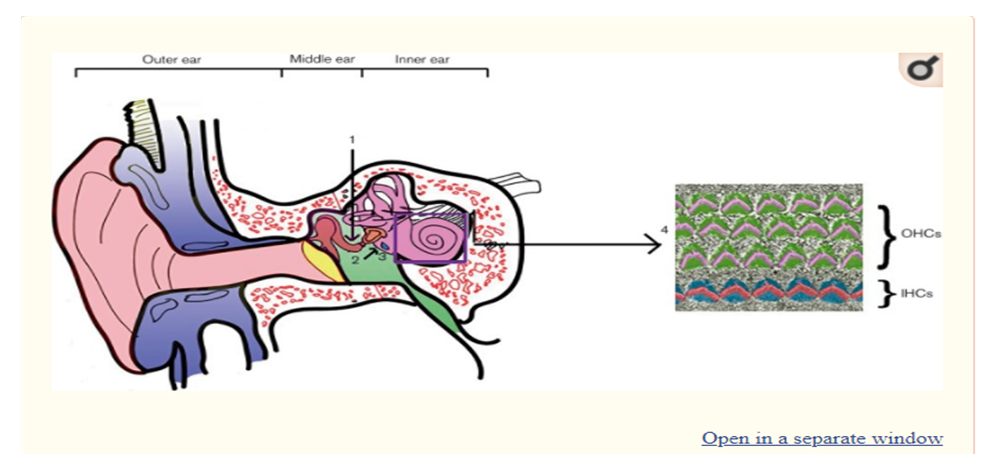
- These inflammatory mediators can also penetrate the round window membrane and pass into the inner ear causing cochlear damage (Fig. 3).
4. Discussion
- If otitis externa is detected in adults, the main treatment is the use of ear drops. In a healthy person with normal immunity, external otitis can be cured by the use of drops alone, without the need for antibiotics in the form of injections or tablets. The drops may contain only an antibacterial drug or a combination of antibiotic and anti-inflammatory agent. Otitis externa is treated for an average of one week. In general, the following are prescribed for the treatment of otitis externa [12]:Ø Antibiotics - norrofloxacin (normax), ciprofloxacin hydrochloride (Ciprox), rifamycin (Otofa);Ø Corticosteroid antibiotics - Candibiotics (beclomethasone, lidocaine, clotrimazole, chloramphenicol), Sofradex (dexamethasone, framicetin, gramicidin);Ø Antiseptics (Miramistin);Ø Antimicrobial ointments - clotrimazole (Candide), natamycin (Pimafutsin, Pimafucort) - if the cause of otitis externa is a fungus.The recently approved ointment, which contains the active ingredient "mupirocin", which has no pathological effect on normal skin microflora, but is effective against fungi, is also showing its effectiveness. Antibacterial drugs are commonly used to treat otitis media. However, the treatment of otitis in adults is slightly different from the treatment of otitis in children - in adults, the disease has a 90% chance of healing on its own, eliminating the need for antibiotics. However, the remaining 10% of cases can lead to very serious consequences, so if no improvement is observed after the first two days of illness, antibiotics are prescribed.Taking antibiotics should be prescribed by a qualified physician as the side effects of such substances can be dangerous. However, complications from otitis cause up to 28,000 deaths a year, so treatment is usually justified. Antibiotics are usually given in tablet form, but if the patient is unable to take the medicine, an injection is given. The following are used to treat otitis media in older patients [13]:Ø Amoxicillin (Flemoxin Solyutab, Ekobol, Ospamox or Amosin);Ø Combination of amoxicillin with clavunal acid (Flemoclav, Augmentin, Ecoclav);Ø Cefuroxime (Sefurus, Aksetin, Zinnat, Zinatsef).Other medications may be prescribed, but it is important to follow the basic requirements of antibiotic treatment: the duration of treatment should be at least a week. If the microorganisms are not completely destroyed due to the discontinuation of the antibiotics, the bacteria will resist this group of drugs and the antibiotics will no longer affect them.
5. Conclusions
- Complex treatment of otitis media usually involves the use of drops. Because not all ear drops are the same, if an earache starts, not every ear drop is right for the treatment. The difference is that the active ingredients for the treatment of otitis are completely different before and after the perforation of the tympanic membrane. If the tympanic membrane is intact, lidocaine, benzocaine, or choline salicylate may be used as painkillers - Otipax, Otinum, or Otizol. In the catarrhal form of otitis media in adults, antibiotic drops do not help at all, because the inflammation does not reach the center of inflammation behind the eardrum. Conversely, if the pus has come out and a crack has formed in the tympanic membrane, the pain-relieving drops are of no use, as they can lead to undesirable consequences. They are not needed because the pain goes away as soon as the pus comes out. Antibiotics are prescribed - "Normax", "Tsiprofarm", "Miramistin" and others, to prevent the recurrence of pus and the penetration of pus into the inner ear, they are prescribed by a doctor. The use of ototoxic antibiotics, alcohol solutions, phenazone or choline salicylate is strictly prohibited [14].When drug treatment is ineffective, a large amount of pus accumulates behind the eardrum. This causes severe pain and the absorption of the products of the vital activity of bacteria into the blood. General intoxication of the body is observed. When such symptoms appear, doctors consider paracentesis to be an emergency, a practice that prevents the development of serious complications of otitis. The operation is performed under local anesthesia. With minimal damage to the paracentesis, a hole is made in the thinnest part of the eardrum using a special thin needle, through which pus is expelled. In addition, a finely wound wound heals much faster than a crack created by natural perforation, and minimal scarring occurs after paracentesis. The next day, the health condition improves dramatically and the patient’s recovery accelerates. This is especially true of paracentesis, which is used to treat otitis in children. Immediate paracentesis is recommended in the following cases [15]:Ø Inflammation of the inner ear;Ø Cerebral palsy (manifested as headache and nausea);Ø Damage to facial nerves;Ø Three days after the start of antibacterial treatment, the pain does not subside and the pus does not come out.Unlike external or secondary otitis, the treatment of inflammation of the auditory labyrinth involves complex procedures and is carried out in medical institutions under the constant supervision of a neurologist and otolaryngologist. not only antibiotics are needed to treat otitis media, but also neuroprotectants and other medications to improve microcirculation in the inner ear.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML