-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(6): 501-505
doi:10.5923/j.ajmms.20211106.08
Received: Jun. 9, 2021; Accepted: Jun. 27, 2021; Published: Jun. 30, 2021

Multiple Primary Malignant Tumors of the Female Reproductive System as the Risk Indicators for Oncopathologies Development
K. Sh. Izrailbekova, S. V. Kamishov
Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology, Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

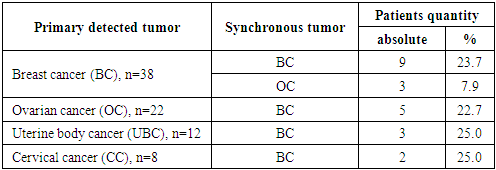
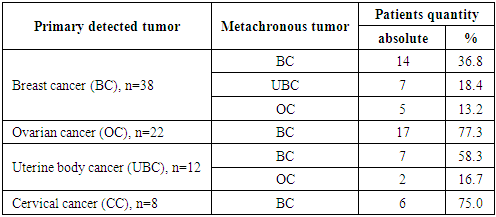
The aim of the research was to study the frequency of development of synchronous and metachronous tumors, as well as the combination of various types of cancer among patients with primary multiple malignant tumors of the female reproductive system, which is important for improving the diagnosis of this category of patients. Material and methods. 80 patients with multiple primary malignant tumors with lesions of the female reproductive system (II-III clinical stages of the disease) were included in the study. Results. In our studies, synchronous tumors were found in 22 (27.5%), and metachronous tumors – in 58 (72.5%) patients. 9 (23.7%) from 38 patients with breast cancer were diagnosed with synchronous cancer of the second breast, and 3 (7.9%) were diagnosed with ovarian cancer. At the same time, synchronous breast cancer was detected in 5 (22.7%) of 22 patients with primary ovarian cancer, in 3 (25.0%) of 12 patients with uterine body cancer and in 2 (25.0%) of 8 patients with cervical cancer. Metachronous tumors were diagnosed in 26 (68.4%) patients with breast cancer, in 17 (77.3%) with ovarian cancer, in 9 (75.0%) with uterine body cancer and in 6 (75.0%) patients with cervical cancer. The most often metachronous tumors were detected in the period from 6 months to 1 year and from 1 year to 2 years in 26 (44.8%) patients. Conclusion. Thus, each of the female reproductive system tumors should be considered as an indicator of other oncopathologies risk. And effective dispensary monitoring will allow to monitor the development of multiple primary malignant tumors in this type of patients in advance.
Keywords: Metachronous tumors, Primary multiple malignant tumors, Tumors of the female reproductive system, Synchronous tumors
Cite this paper: K. Sh. Izrailbekova, S. V. Kamishov, Multiple Primary Malignant Tumors of the Female Reproductive System as the Risk Indicators for Oncopathologies Development, American Journal of Medicine and Medical Sciences, Vol. 11 No. 6, 2021, pp. 501-505. doi: 10.5923/j.ajmms.20211106.08.
Article Outline
1. Introduction
- There is an increasing interest in studying issues related to the problem of multiple primary malignant tumors (MPMT) among oncologists due to the wide spread increase in the number of patients with this type of oncopathology [2,19]. Many researchers agree that polyineoplasias are most often found in women. It is associated with an increase in the incidence of the reproductive system hormone-dependent tumors, which is functionally represented by the mammary glands, uterus and ovaries [14,18]. Malignant tumors of the reproductive system are the most frequent in the structure of cancer morbidity in women and their total share exceeds 35%. According to various authors, the frequency of MPMT of the female reproductive system ranges from 0.8% to 12.6% of all cancer cases of these localities [1,6,11]. The issue of the time boundary between the synchronicity and metachronism of the malignant tumors development has been open for a long time [13]. Currently, most authors consider the most reliable, although rather conditional interval of occurrence of the second metachronous tumor, a period of more than 6 months from the diagnosis of the first one. In the vast majority of cases (75-80%) metachronous tumors occur in the period from 3 to 15 years, although isolated cases of the second tumors occurrence at a later time are described [7,20]. According to various authors data in patients with breast cancer (BC) MPMT occurs in 1.9-7.1% of cases. Most often, breast cancer is associated with malignant tumors of the female reproductive system (33-42%): ovarian cancer (OC) (15-17%), uterine body cancer (UBC) (12-14%), cervical cancer (CC) (10-12%). Next in the frequency of occurrence is cancer of the colon and rectum (12-13%), then the stomach (14-15%) and thyroid cancer (7.7%). The remaining localizations of malignant tumors are described in single observations [2,3]. Among UBC patients, the most frequent combination is noted with breast tumors, which confirms the hormonal dependence of malignant cervical tumors. In UBC patients, the relative risk of breast cancer (BC) is 13.6% in the first year, 5.3% in the fifth, 3.9% in the tenth and 3.0% in the fifteenth year. In patients with breast cancer, the relative risk of UBC is 9.0% in the first year, 2.4% in the fifth, 2.2% in the tenth, and 3.6% in the fifteenth year. Consequently, in patients with both BC and UBC, the risk of a second tumor developing is realized mainly in the first year due to synchronous polyineoplasias. The synchronicity of UBC and OC development and the relatively short interval between the development of UBC and BC, indirectly indicate the common pathogenetic mechanisms of these malignant tumors development [16,17].The aim of the research was to study the frequency of development of synchronous and metachronous tumors, as well as the combination of various types of cancer among patients with primary multiple malignant tumors of the female reproductive system, which is important for improving the diagnosis of this category of patients.
2. Material and Methods
- 80 patients with multiple primary malignant tumors with lesions of the female reproductive system (II-III clinical stages of the disease) were included in the study, which were examined and treated in the departments of oncomammology, oncogynecology and chemotherapy-2 of Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology from 2015 to 2021. In accordance with the objectives of the study, the patients were divided into the following groups: group 1- 38 (34.5%) patients with breast cancer (BC); group 2-22 (20.0%) patients with ovarian cancer (OC); group 3-12 (10.9%) patients with uterine body cancer (UBC); group 4-8 (7.3%) patients with cervical cancer (CC).The age of the examined BC patients varied from 23 to 79 years, the mean age was 46.8±7.3 years; in OC patients the age ranged from 24 to 68 years, the mean age was 45.7±6.4 years; in UBC patients the age varied from 32 to 76 years, the meanage was 48.6±6.8 years; in CC patients the age ranged from 25 to 69 years and the mean age was 43.5±7.0 years.Disease-specific staging was performed according to the International Clinical Classification TNM (7th ed. and 8th ed.) and FIGO (2009 and 2016) [4,8,9,10]. As it follows from the data presented in the main groups, in BC patients IIB and IIA stages of the disease were more common; in patients with OC - IIB, IIA and IIIC stages; in UBC patients -I IB and IIC stages and in CC patients -IIB and IIIB stages of the tumor process.
3. Results and Discussion
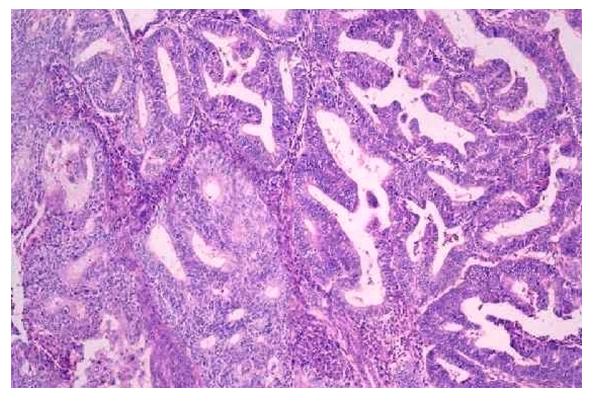
- The results of the study showed that infiltrating ductal cancer prevailed in patients with breast cancer – 22 (57.9%) cases. A mixed form of ductal and lobular types of cancer was revealed in 9 (23.7%) cases, infiltrating cancer occurred in 3 (7.9%) patients. The study of the OC morphological structure showed that 10 (45.5%) patients had serous cystadenocarcinoma, 6 (27.3%) – undifferentiated cancer, 4 (18.2%) – endometrioid cancer and 2 (9.1%) patients - mucinous cystadenocarcinoma, respectively.Histological analysis of UBC biopsy samples showed that in 8 (66.7%) patients endometrioid carcinoma was detected, in 2 (16.7%) cases – serous-papillary adenocarcinoma, in 1 (8.3%) patient – mixed carcinoma and 1 (8.3%) patient – light cell carcinoma.The morphological structure of the CC was also studied. Histologically, 4 (50.0%) patients had squamous cell carcinoma with keratinization, 3 (37.5%) – without keratinization. Adenocarcinoma was detected in1 (12.5%) patient.When analyzing the family oncological history of the examined patients, breast cancer (BC) was noted in 22 (57.9%) blood relatives on the maternal line, 2 (5.3%) of them had ovarian cancer (OC) and 4 (10.6%) had a combination of OC and BC.The study of the anamnesis data showed that in most of the patients – 35 (43.8%) - the symptoms of the disease appeared in the period from 3 to 6 months. In our studies, synchronous tumors were found in 22 (27.5%), and metachronous tumors – in 58 (72.5%) of the examined patients. Synchronous tumors, occurred in the period from 3 to 6 months, were found in 12 (31.6%) patients with breast cancer, synchronous second breast cancer was found in 9 (23.7%) of them, and ovarian cancer – in 3 (7.9%) cases. In patients with primary detected OC, UBC, and CC, synchronous breast cancer was simultaneously detected in 5 (22.7%), 3 (25,0%) and in 2 (25.0%) patients, respectively (Tab. 1).
|
|
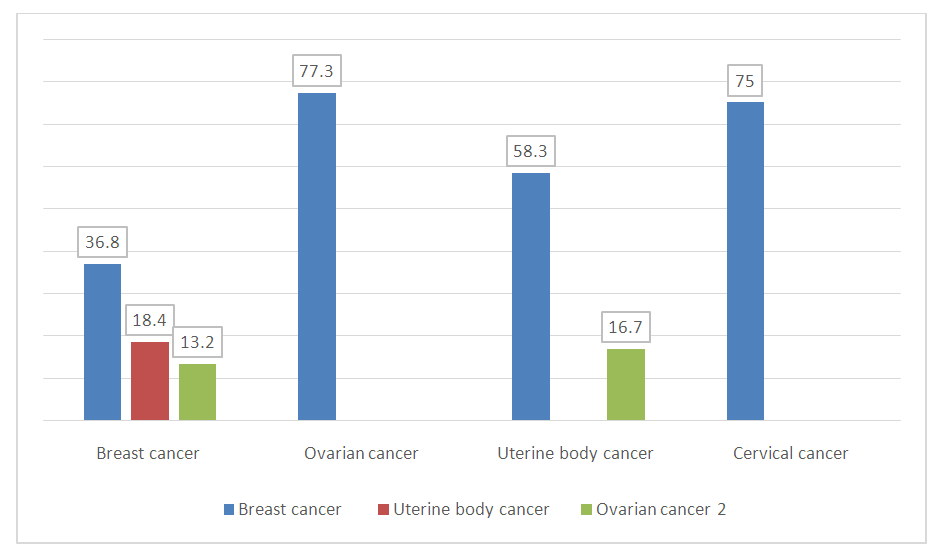 | Figure 1. Percentage of metachronous combined tumors in patients with multiple primary malignant tumors, n=80 |
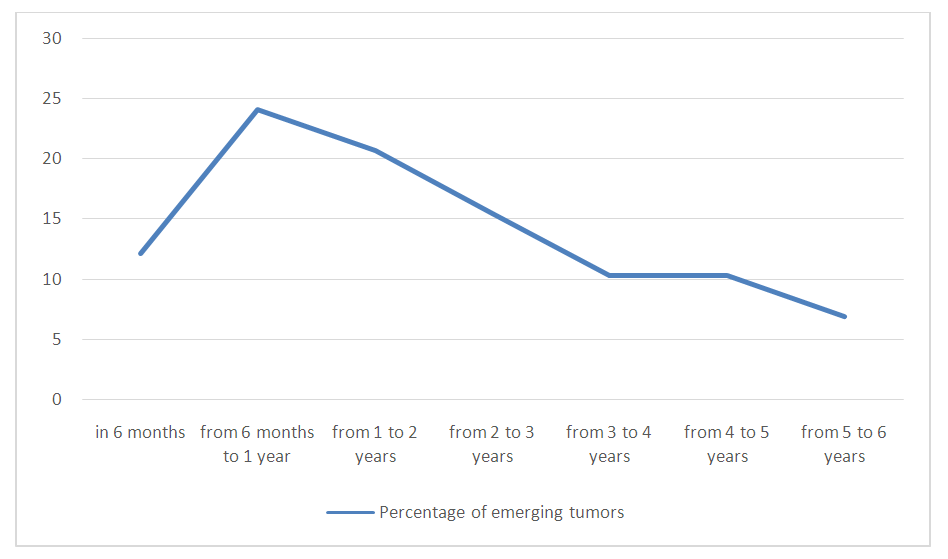 | Figure 2. Distribution of metachronous tumors in the examined patients at different follow-up periods, in percentage |
4. Conclusions
- In our studies, synchronous tumors were found in 22 (27.5%) of 80 patients with multiple primary tumors. In our studies synchronous tumors were found in 12 (31.6%) patients with breast cancer, synchronous second breast cancer was found in 9 (23.7%) of them and ovarian cancer – in 3 (7.9%) cases. In patients with primary detection of OC, UBC, and CC, synchronous breast cancer was simultaneously detected in 5 (22,7%), in 3 (25,0%) and in 2 (25.0%) patients, respectively.Metachronous tumors at the period of 6 months and above were subsequently detected in 26 (68.4%) patients with breast cancer: metachronous second breast cancer – in 14 (36.8%), UBC – in 7 (18.4%) and OC – in 5 (13.2%) patients. Metachronous breast cancer was detected in patients with OC and CC (17 (77.3%) and 6 (75.0%), respectively). In patients with UBC we found metachronous breast cancer and ovarian cancer (7 (58.3%) and 2 (16.7%), respectively).Metachronous tumors were most often detected in the period from 6 months to 1 year and from 1 year to 2 years in 26 (44.8%) patients.The conducted studies allow us to conclude that multiple primary malignant tumors in female oncopathology are primarily associated with breast cancer, while uterine body cancer is also associated with ovarian cancer, which is observed both in synchronous and metachronous forms of their development. In the case of primary ovarian cancer and cervical cancer, metachronous tumors of the breast alone were observed.
Дополнения
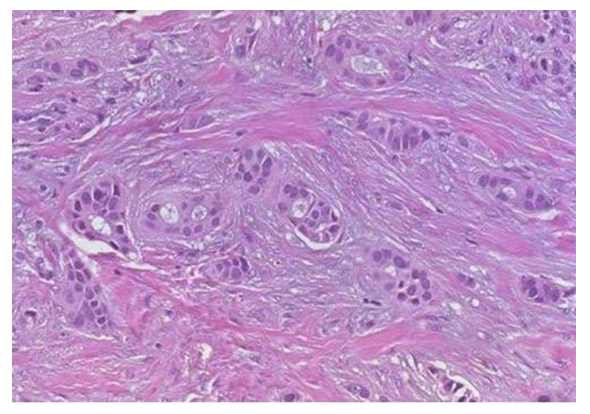 | Больная Х. И/б №54628. 15.07.2018 г. Инфильтративный протоковый рак молочной железы. У больной через1,5 года развился метахронный рак яичников. |
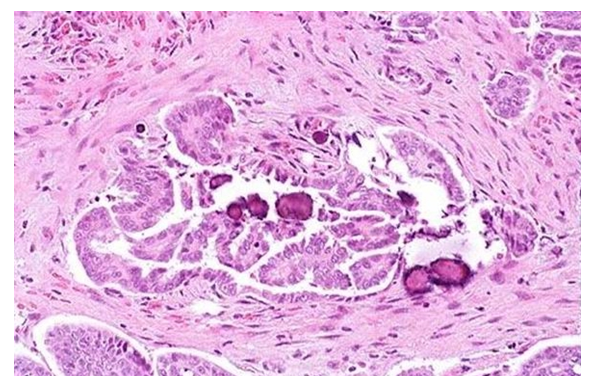 | Больная Ф. И/б №22431. 21.03.2016 г.Серозная цистаденокарцинома яичника. У больной в течение 4-х месяцев развился рак левой молочной железы. |
 | Больная У. И/б №32561. 12.01.2017 г. Серозная цистаденокарцинома яичника. У больной в течение 3-х месяцев развился рак правой молочной железы. |
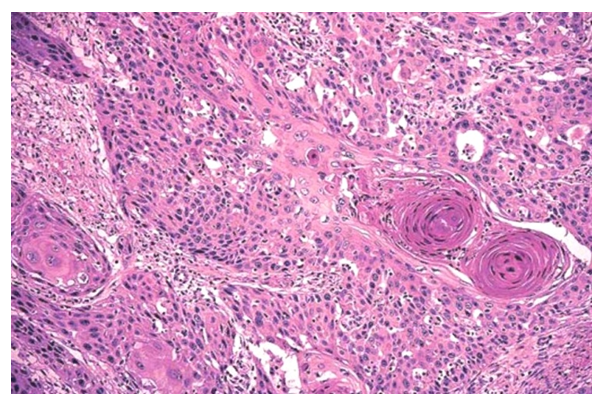 | Больная Ч. И/б №36298. 26.04.2017 г. Плоскоклеточный рак шейки матки с ороговением. У больной в течение 2-х лет развился рак правой молочной железы. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML