-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(6): 495-500
doi:10.5923/j.ajmms.20211106.07
Received: Jun. 6, 2021; Accepted: Jun. 22, 2021; Published: Jun. 30, 2021

The Role of Radiation Research Methods in the Diagnosis of the Biliary Tract Cystic Transformations in Children
Khabibulla Akilov, Khamid Matyakubov
Republican Research Center of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the study is to improve diagnostic and treatment results of various forms of choledochal cyst transformations in children through the use of highly informative diagnostic methods and the introduction of new treatment technologies. Introduction. Choledochal cysts transformation is a relatively rare abnormality of the biliary tract. In 80% of cases choledochal cysts transformation is detected in childhood and adolescence. In most cases, this pathology is diagnosed in infants and children (in 25% of cases - in children of the first year of life and in 60% - at the age of 10 years). Material and methods. The research is based on the analysis, diagnostics and treatment of 78 patients aged from 2 months to 18 years with choledochal cysts transformation, who were observed in the Department of Pediatric Surgery of the Republican Research Centre of Emergency Medicine for the period from 2005 to 2021. Results and discussion. 78 children were examined and treated: 56 (71.8%) girls and 22 (28.1%) boys. Ultrasound investigation of the liver and abdominal organs was performed in all patients of the control and main groups. Great importance was attached to retrograde endoscopic examinations in the diagnostics of various clinical forms and types of choledochal cysts. All patients were performed the following surgical procedures: in 39 (50.0%) cases - resection of the choledochal cyst with the imposition of a hepaticenteroanastomosis with a skeleton ring on the Roux loop of the small bowel, in 32 (41.0%) patients - resection of the choledochal cyst with the imposition of hepaticoenteroanastomosis on the Roux loop of the small bowel, in 6 (7.6%) cases, supraduodenal choledohoduodenoanastomosis was applied, in 1 (1.4%) patient - Kerr's drainage (due to perforation of the choledochal cyst). Conclusion. Timely recognition of congenital dilation of the common bile duct presents significant difficulties. Choledochal cysts in children belong to the group of rare diseases which stipulates its difficulty in diagnosing them. A thorough assessment of clinical data and anamnesis study allow to suspect the disease, and endoscopic retrograde cholangiopancreatography, percutaneous and transhepatic cholangiography, magnetic resonance cholangiopancreatography helps to clarify the diagnosis, to determine the nature and type of lesion.
Keywords: Choledochal cysts, Anastomosis, Children
Cite this paper: Khabibulla Akilov, Khamid Matyakubov, The Role of Radiation Research Methods in the Diagnosis of the Biliary Tract Cystic Transformations in Children, American Journal of Medicine and Medical Sciences, Vol. 11 No. 6, 2021, pp. 495-500. doi: 10.5923/j.ajmms.20211106.07.
1. Introduction
- Choledochal cysts transformation (CCT) is a relatively rare abnormality of the biliary tract. In 80% of cases choledochal cysts transformation is detected in childhood and adolescence [1-6]. In most observations this pathology is diagnosed in infants and children (in 25% of cases - in children of the first year of life and in 60% - at the age of 10 years). In the adult population, the disease is more common in young women, the ratio of women/men is approximately 4/1 [1-2,5-7]. The morbidity rate is 1 per 100,000 population in Western countries [1-2,4-6,8] and 1 per 13,000 population in Japan [2,5-6]. The pathogenetic basis of the disease is considered to be congenital hypoplasia of the muscular layer of the duct, neuromuscular dysfunction of the sphincter of Oddi [2]. The clinical picture of CCT has a characteristic triad of symptoms: abdominal pain (90-92%), intermittent jaundice (43-70%), palpable tumor-like formation in the right hypochondrium (25-60%). In 20% of patients, the clinical picture may be absent for a long time [9,2-3]. The difficulty of diagnosing CCC is due to the fact that it can be asymptomatic in the early stages. The lack of clear clinical manifestations significantly complicates the early diagnostics of congenital diseases of the bile ducts [10].Full-fledged diagnostics of bile duct cysts is possible only with the help of special research methods. It is important to have the most complete understanding of the cyst size in various parts of the hepatobiliary tract, its contents, the relationship of the cyst with the surrounding organs and structures. This is important not only for assessing the degree of existing pathological changes, but also for choosing the optimal method of surgical correction of pathology [11]. The introduction of ultrasound investigation (USI), multi-spiral computed tomography (MSCT), magnetic resonance imaging (MRI), including magnetic resonance cholangiopancreatography (MRCP), endoscopic retrograde cholangiopancreatography (ERCP), as well as percutaneous and transhepatic cholangiography and cholangiostomy (PTHC and PTHCS) into clinical practice has allowed not only to early diagnose of cystic transformation of the common bile duct, dynamic monitoring of patients in order to control the size of dilatation, but also to choose the optimal period of surgical intervention [12-13]. They allow us to get data not only about the existence of the cyst, its size and position, but also gives an idea of the cyst walls, its contents, relationships with the surrounding organs, the nature of their changes. Their efficiency is 75.8—79.2%. The most reliable data is provided by ERCP, but recently it is rarely used due to its high invasiveness [3]. The aim of the study is to improve diagnostic and treatment results of various forms of choledochal cyst transformations in children through the use of highly informative diagnostic methods and the introduction of new treatment technologies.
2. Material and Methods
- The research is based on the analysis, diagnostics and treatment of 78 patients aged from 2 months to 18 years with choledochal cysts transformation, who were observed in the Department of Pediatric Surgery of the Republican Research Centre of Emergency Medicine for the period from 2005 to 2021.In the research material, along with uncomplicated forms of CCT, we included complicated forms of this pathology with clinical manifestations of mechanical jaundice and purulent cholangitis. Complicated forms of cystic changes in choledochus had the peculiarity of progressing according to their own laws, acquired the features of an independent disease and, accordingly, required a separate treatment program.Depending on the tactics and method of therapeutic and diagnostic procedures, all patients with various forms of CCT were divided into 2 groups: control and main. The control group included 39 (50%) patients who were treated with traditional therapeutic and diagnostic tactics. In 39 (50%) patients of the main group, the treatment and diagnostic process was supplemented by modern methods of radiation and endobiliary diagnostics, as well as a new method of surgical treatment of choledochal cysts transformations in children using an external metal frame. All patients with various forms of CCT were examined urgently. The diagnostic process at the availability of contact began with finding out the complaints of patients. In parallel, a thorough but rapid physical examination was carried out using the methods of questioning, examination, palpation, auscultation, percussion.Further, the examined patients were performed laboratory examination and instrumental diagnostics, the purpose of which was: to clarify or confirm the presence of CCT with determination of its clinical form and type, to assess the general condition of patients and to choose treatment tactics with the determination of an adequate method of surgical intervention.
3. Results
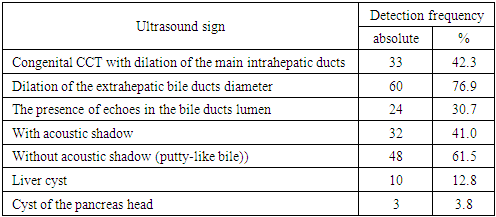
- 78 children were examined and treated: 56 (71.8%) girls and 22 (28.1%) boys. In total, X-ray examination of the chest and abdominal organs was performed in 52 (66.6%) patients. Ultrasound investigation (USI) of the liver and abdominal organs was performed in all patients of the control and main groups. USI was performed in 100% of all sick children, which allowed to diagnose a choledochal cyst in 79.6% of cases (n=60). The most characteristic signs were: the diameter of the extrahepatic and intrahepatic bile ducts, the nature of their contents, the presence of acoustic shadows, as well as the state of the liver, pancreas and neighboring organs (Tab. 1).
|
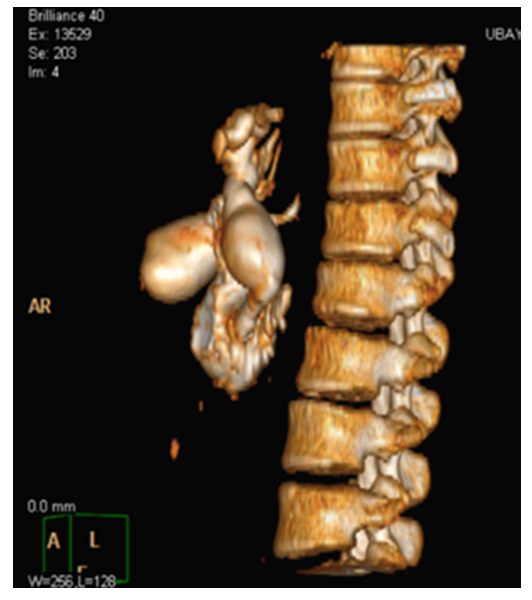 | Figure 1. 3D-reconstruction of cystic dilation of the common bile duct of type I |
4. Discussion
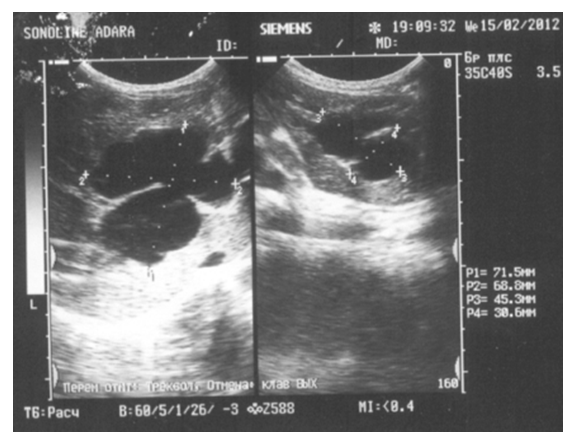
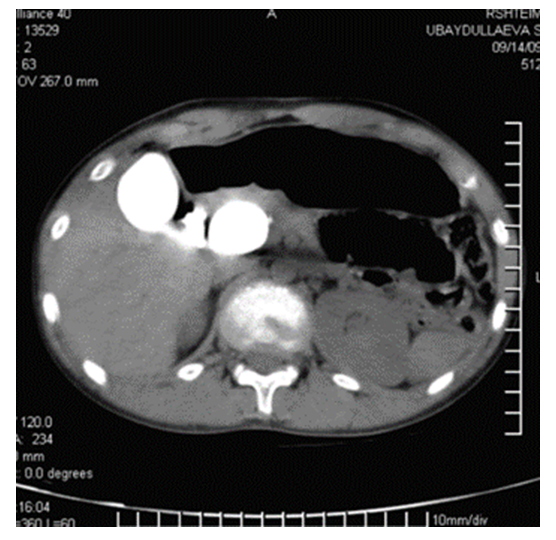
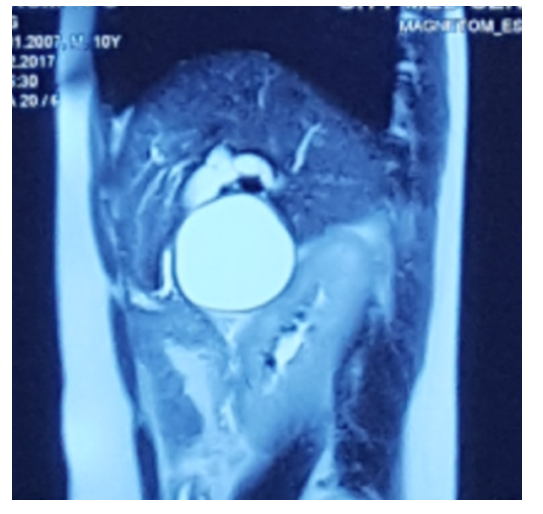
- A mandatory set of laboratory diagnostic methods for accurate and timely diagnosis of all patients with various clinical forms of CCT was carried out, including the determination of clinical and biochemical blood parameters, characteristics of the acid-base state (ABS). It was mandatory to assess the level of hemoglobin, red blood cells, hematocrit, to determine the leukocytosis with the leukocyte formula and the rate of erythrocyte sedimentation (ESR).The most important advantage of ultrasound investigation was its non-invasiveness, speed of execution (3-5 minutes), high sensitivity in detecting direct and indirect signs of various clinical forms and types of CCT, safety and ease of execution, allowing for a repeat study with an assessment of the process dynamics. At the same time, the resolution capabilities of echography in patients with CCT are significantly reduced in some complex clinical situations. In this regard, USI in the diagnostics of CCT was considered as a primary, screening investigation.In the study of patients with CCT, the presence of a cavity formation in the the liver gate area was determined in all cases (Fig. 2), but it was not always possible to clearly differentiate where it came from (Fig. 3). At the large size of the cyst it was difficult to determine whether it comes from the liver itself (solitary or parasitic cyst) (Fig. 4), the head of the pancreas, or it is directly a hepaticocholedochal cyst.
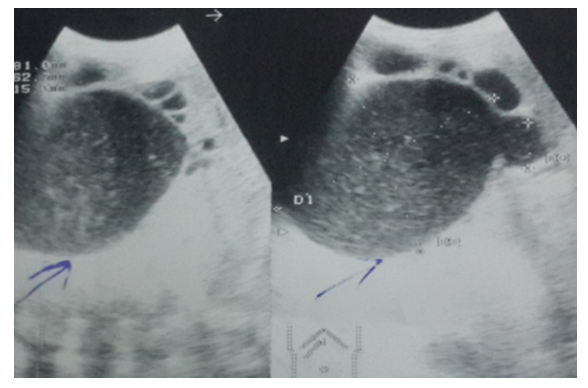 | Figure 2. Cystic formation of hepaticocholedochus |
 | Figure 3. Cystic formation of the intra-and extrahepatic bile ducts |
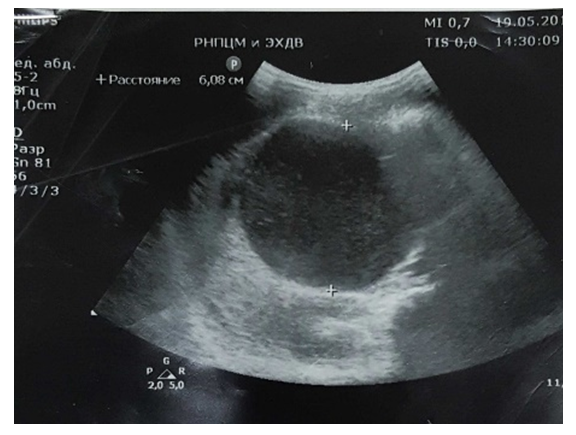 | Figure 4. Volume formation in the IV-V-VI segments of the liver |
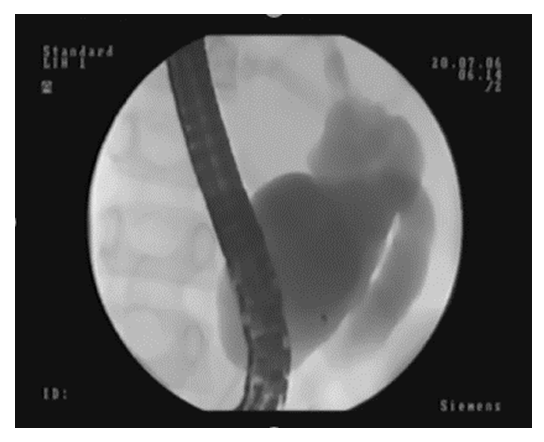 | Figure 5. ERCP. Cystic dilation of the intra-extrahepatic bile duct |
 | Figure 6. EPST by L. Demlihg and K. Kawai method (1980) |
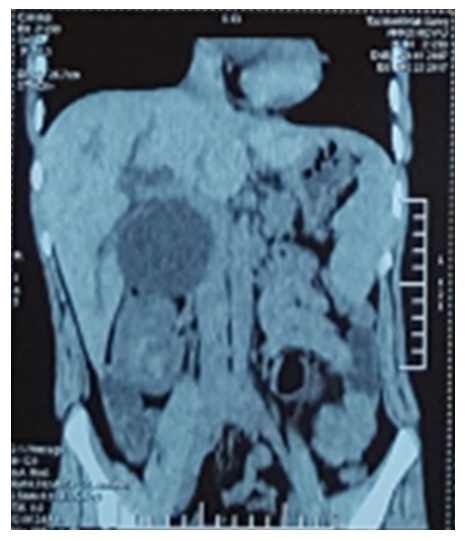 | Figure 7. MSCT. The common bile duct cystic dilation of type I |
 | Figure 8. After ERCP |
 | Figure 9. MR-signs of a huge cyst (echinococcal?) in the mesenteric zone with compression of the choledochus and the common bile duct |
 | Figure 10. MR-signs of hepaticocholedochus cystic transformation |
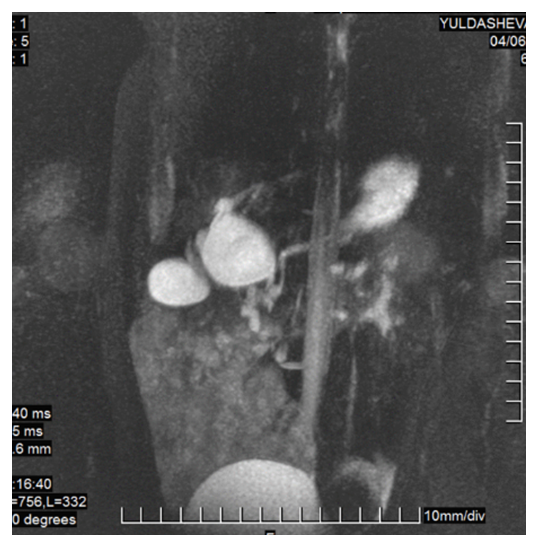 | Figure 11. MRI-cholangiography. CCT and choledocholithiasis |
 | Figure 12. PTHC. CCT at the level of porta hepatis |
 | Figure 13. PTHC |
5. Conclusions
- Timely recognition of congenital dilation of the common bile duct presents significant difficulties. Choledochal cysts in children belong to the group of rare diseases which stipulates its difficulty in diagnosing them. A thorough assessment of clinical data and anamnesis study allow to suspect the disease, and endoscopic retrograde cholangiopancreatography, percutaneous and transhepatic cholangiography, magnetic resonance cholangiopancreatography helps to clarify the diagnosis, to determine the nature and type of lesion.A radical operation for cysts of the extrahepatic bile ducts is considered to be the maximum excision of the cystically altered walls of the hepaticocholedochus and the imposition of a hepaticenteroanastomosis with a skeleton ring on the Roux loop of the small bowel.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML