-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(5): 419-425
doi:10.5923/j.ajmms.20211105.13
Received: May 1, 2021; Accepted: May 21, 2021; Published: May 26, 2021

Clinical-Laboratory Markers of Progression of Non-Alcoholic Fatty Liver Disease
Abror Asrorovich Khamraev1, Dilnavoz Khasanovna Yuldasheva2, Zarifa Ramazonovna Mukhamedova3, Vokhid Zokhidovich Zokirov3
1Head of the Department of Internal Medicine, Tashkent Medical Academy, Tashkent, Uzbekistan
2Department of Propaedeutics of Internal Medicine, Bukhara Medical Institute, Uzbekistan
3Department of General Hygiene and Ecology, Bukhara Medical Institute, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

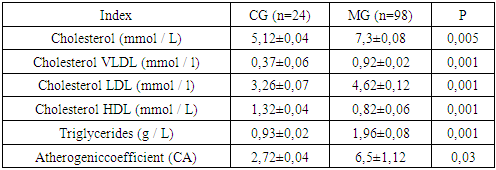
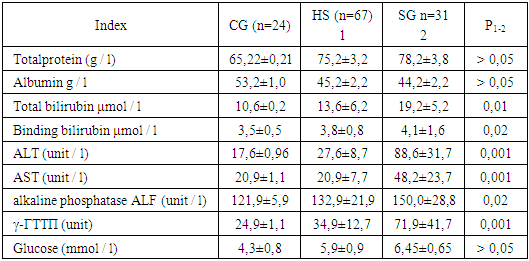
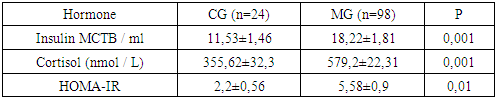
Non-alcoholic fatty liver disease (NAFLD) high prevalence, a tendency to an increase in morbidity, disease progression, coverage of the most efficient part of the population, the severity of clinical manifestations only in the late stages makes it possible to classify NAFLD as socially significant, of course, makes NAFLD one of the urgent problems of clinical medicine. The main feature of NAFLD is the absence of symptoms; the disease is often detected by chance, based on laboratory or instrumental tests. This article studied clinical and laboratory analyzes of 98 patients with non-alcoholic fatty liver disease. With steatohepatitis, higher ALT and AST values are noted than in patients with hepatic steatosis. The main differential difference between non-alcoholic steatosis and steatohepatitis, available in clinical practice, may be the severity of the biochemical syndrome of cytolysis. The article contains clinical features and prognosis in patients with fatty hepatosis and non-alcoholic steatohepatitis (NASH). Dyslipidemia (hypertriglyceridemia, decreased HDL, increased LDL) occurs in about 65-85% of patients. The basal insulin level, according to the results of our studies, in persons with NAFLD at the stage of steatosis and steatohepatitis was significantly increased.
Keywords: Non-alcoholic fatty liver disease, Liver steatosis, Non-alcoholic steatohepatitis, Insulin resistance, Obesity, Lipoprotein, Cholesterol, Alanine aminotransferase
Cite this paper: Abror Asrorovich Khamraev, Dilnavoz Khasanovna Yuldasheva, Zarifa Ramazonovna Mukhamedova, Vokhid Zokhidovich Zokirov, Clinical-Laboratory Markers of Progression of Non-Alcoholic Fatty Liver Disease, American Journal of Medicine and Medical Sciences, Vol. 11 No. 5, 2021, pp. 419-425. doi: 10.5923/j.ajmms.20211105.13.
Article Outline
1. The Urgency of the Problem
- Currently, non-alcoholic fatty liver disease (NAFLD) is one of the most common diseases in hepatology, leading to a deterioration in the quality of life, disability and death. The overall prevalence of NAFLD in the population ranges from 10 to 40% [2,4,11,20,26,33,42]. NAFLD is in the focus of attention not only of general practitioners and gastroenterologists, but also of cardiologists, endocrinologists, and nephrologists, which is associated with the existence of a close relationship between the presence of NAFLD and a high risk of cardiovascular events, type 2 diabetes mellitus, chronic kidney disease [1,5,8,11,15,34,35,39]. The main feature of NAFLD is the absence of symptoms; the disease is often detected by chance, on the basis of laboratory or instrumental tests. NASH symptoms are nonspecific and do not correlate with its severity [38,42].In the normal course of NAFLD, 12-40% of patients with hepatosis develop non-alcoholic steatohepatitis after 8-13 years. Of these, 15% of patients develop liver cirrhosis and liver failure. Of 7% of patients with liver cirrhosis, hepatocellular carcinoma develops within 10 years. The heterogeneity of NAFLD leads to the absence of a single generally accepted standard of treatment for such patients. Of course, all overweight patients should be advised to reduce their weight by eating a low-calorie diet and exercising regularly, and the effect of the latter seems to be more significant. Unhealthy lifestyles are the leading cause of NAFLD [2,3,11,12,18,24,27,28,30,33,36,41,43].NAFLD occurs in all age groups, with a greater frequency in the 40-60 age group. Most often, NAFLD was detected in the following age groups: 50–59 years old (31.1%), 40–49 years old (23.6%), 60–69 years old (18.1%). The problem of an increase in the incidence of NAFLD is associated with a significant increase in the number of obese people. Moreover, the severity of the disease increases with an increase in the degree of obesity [4,11,16,17,23,33]. In obese individuals, NAFLD occurs in 30-100% of cases [16,22]. The prevalence of NAFLD among patients with type 2 diabetes mellitus (DM) reaches 70% [13,31]. NAFLD is a very diverse group of diseases, essentially differing in the combination of etiopathogenetic factors, the rate of progression and prognosis. In some cases, there is a steadily progressive course with the development of liver cirrhosis, in some cases - hepatocellular carcinoma.The most common risk factors in the NAFLD population were dyslipidemia (type 2 according to Friedrichsen) - 75.9% of patients, arterial hypertension - 69.9% and hypercholesterolemia - 68.8% [4,33,39,41,42]. NAFLD is a chronic multifactorial liver disease with a tendency to progression, which can be presented as hepatic steatosis, steatohepatitis, or liver cirrhosis. The prevalence of dyslipidemia among patients with NAFLD reaches 75%, and these figures are twice as high as in the population [5,9,21]. In 2003, at the I World Congress on Insulin Resistance in Los Angeles, it was suggested that NAFLD, along with obesity, type 2 diabetes, dyslipidemia, arterial hypertension, is a component of metabolic syndrome. The reasons for the development of NAFLD are varied, but more often there is a combination [8,10,19,33,37,40,42]. The main etiological factors of NAFLD are: eating foods high in saturated fat; low physical activity; hormonal disorders; primary and secondary insulin resistance (IR); obesity [4,7,34,38]. Thus, the high prevalence, the tendency to an increase in the incidence, the progression of the disease, the coverage of the most efficient part of the population, the severity of clinical manifestations only in the late stages allows us to classify NAFLD as socially significant, of course, makes NAFLD one of the urgent problems of clinical medicine [6,33,41,42,43].Purpose of the study: To determine the clinical and laboratory features of non-alcoholic fatty liver disease at the stage of fatty hepatosis and steatohepatitis.
2. Materials and Research Methods
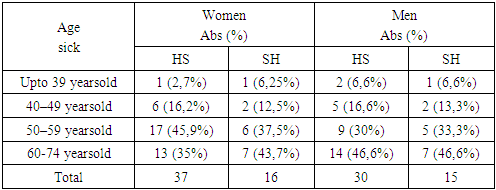
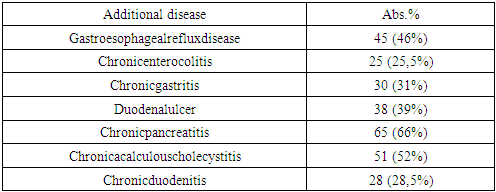
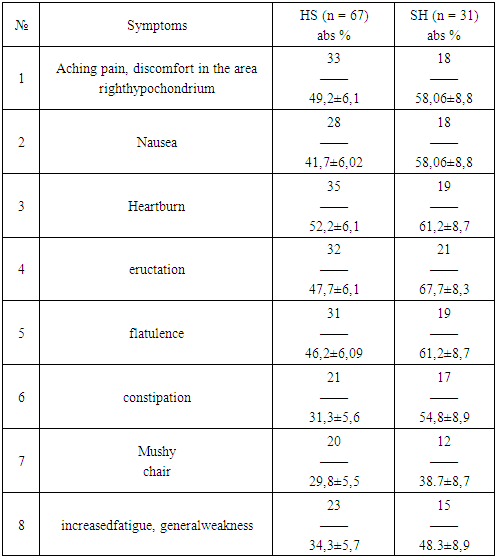
- To solve the set tasks, 98 patients with NAFLD were examined, including 67 (68.3%) patients at the stage of hepatic steatosis (HS) and 31 (31.6%) patients with steatohepatitis (SH). Of these, 45 (46%) men and 53 (54%) women aged 20 to 75 years (average age 49.2 ± 4.2). The research results were recorded in the developed clinical information cards (questionnaire). The consent of the participants and members of the ethical committee for human rights in biomedicine at the Bukhara medical institute was obtained for the study. When selecting patients, we took into account the criteria for including and not including patients in the study. Criteria for the inclusion of patients in the study: - men and women aged 20 - 75 years; - the presence of fatty hepatosis and steatohepatitis; - the presence of a signed informed consent. The exclusion criteria were suspicion of alcohol or drug dependence, drug, viral, autoimmune liver damage, storage diseases, oncological diseases, severe diseases (uncorrected arterial hypertension (AH), type 2 diabetes in the stage of decompensation, chronic heart failure (CHF) III – IV functional class, heart attacks, strokes), pregnancy, lactation and low compliance. The criterion for not including from the survey was alcohol consumption in patients with fatty liver disease. We took into account the data of the anamnesis (absence of alcoholic beverages consumption regularly). We also used a special CAGE questionnaire [12,29].We compared the results obtained in the course of the study with the indicators of the control group, formed of 24 apparently healthy individuals aged 20 to 65 years, who had no abnormalities in the hepatobiliary system. The diagnosis of non-alcoholic fatty liver disease was made on the basis of anamnesis, laboratory tests, and ultrasound examination of the liver. To detect NAFLD, ultrasound of the hepatobiliary system and liver elastography were performed. Ultrasound examination of the hepatobiliary system was performed in 500 patients with risk factors for NAFLD: obesity, dyslipidemia, impaired carbohydrate tolerance. Ultrasound of the liver revealed steatosis and steatohepatitis in 98 patients with NAFLD. The following signs of hepatic steatosis were noted: an increase in the size of the liver, an increase in its echogenicity, a relatively reduced density of the liver compared to the spleen (hepatic-splenic index less than 1), a decrease in sound conductivity, and a deterioration in visualization of the branches of the portal and hepatic veins. Ultrasound elastography was performed in 98 patients in order to exclude fibrosis in the liver parenchyma. Lipid metabolism was studied in terms of serum cholesterol (CS), high density lipoprotein (HDL), low density lipoprotein (LDL), very low density lipoprotein (VLDL) and triglycerides (TG). The LDL and VLDL values were calculated using the formula: VLDL = TG / 2, LDL = CHCR- (VLDL + HDL). Based on the results obtained, the atherogenic coefficient (CA) was calculated using the formula:CA= CS LDL + CS VLDL/ HDL. Determination of the degree of obesity was carried out according to the Quetelet index, calculating it by the formula: BMI = weight (kg) / height (m2).The results obtained were processed statically using the Student's t-test and the difference was considered significant in those cases when p <0.05 was expressed.
3. Results and Discussion
- According to the results of our study, the ratio of women to men was 1.3: 1. The distribution of patients with hepatic steatosis and steatohepatitis by age is shown in Table 1.
|
|
|
|
|
|
|
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML