-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(5): 406-410
doi:10.5923/j.ajmms.20211105.10
Received: Apr. 26, 2021; Accepted: May 10, 2021; Published: May 26, 2021

Results of Traditional Methods of the Therapy of Gastroduodenal Ulcer Bleeding in Patients with Ischemic Disease
Abdukhakim Muminovich Khadjibaev1, Rasulbek Ibrokhimovich Rakhimov2
1Doctor of Medical Sciences, Professor, Minister of Health of the Republic of Uzbekistan
2Candidate of Medical Sciences, Deputy Chief Physician of Tashkent City Ambulance Clinical Hospital
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article is devoted to the issues of determining the possibilities of the generally accepted tactics of treating patients with ulcerative gastroduodenal bleeding combined with ischemic heart disease. At the same time, a separate analysis of the results of treatment obtained after conservative therapy and endoscopic therapy, as well as surgical correction of these combined pathologies, was carried out.
Keywords: Ulcerative gastroduodenal bleeding, Ischemic heart disease, Conservative therapy, Endoscopic interventions, Surgical correction
Cite this paper: Abdukhakim Muminovich Khadjibaev, Rasulbek Ibrokhimovich Rakhimov, Results of Traditional Methods of the Therapy of Gastroduodenal Ulcer Bleeding in Patients with Ischemic Disease, American Journal of Medicine and Medical Sciences, Vol. 11 No. 5, 2021, pp. 406-410. doi: 10.5923/j.ajmms.20211105.10.
Article Outline
1. Introduction
- The actuality of the problem: It is known that among the concomitant diseases, against the background of which ulcerative gastroduodenal bleeding (UGHB) is especially difficult, a special place is occupied by heart diseases accompanied by coronary insufficiency, such as unstable angina pectoris, acute coronary syndrome (ACS) with and without ST elevation, as well as acute myocardial infarction [1: 31-34; 2:52-54; 4:50-55; 6:31-35; 9:203-207; 12:14-24].In cases of such a combined development of these nosologies, a mutually aggravating effect of one pathological process on another is observed, which significantly aggravates the course of the disease and worsens its prognosis [3:25; 5:98-117; 7; 8:1-46; 10:932-934; 11:386-390].In this regard, it seemed to us expedient to conduct clinical studies to determine the effectiveness of the application of the generally accepted tactics of treatment of gastroduodenal ulcerative bleeding in patients with these combined diseases.In this regard, the purpose of this work was to elucidate the possibilities of the generally accepted tactics of treating ulcerative gastroduodenal bleeding when the latter is combined with heart disease accompanied by acute coronary insufficiency.
2. Material and Research Methods
- The study was carried out in 413 patients with gastroduodenal ulcerative bleeding combined with heart disease accompanied by myocardial ischemia, who were treated at the Department of Emergency Surgery of the Republican Scientific Center for Emergency Medicine from 2010 to 2020. Among the examined patients there were 219 men and 194 women. The average age of the patients was 66.7 ± 1.2 years.All patients with ulcerative gastroduodenal bleeding with ischemic heart disease underwent a comprehensive examination in accordance with the diagnostic and treatment standards of the emergency medical service of the Republic of Uzbekistan, including general clinical, laboratory and special instrumental research methods. The main method of studying the examined patients was esophagogastroduodenoscopy (EGFDS), which we used in 413 patients not only for diagnostic, but also for therapeutic purposes. At the same time, 283 patients had acute ulcers, and 130 patients had chronic ulcerative process. Moreover, in 215 patients, ulcers were located in the stomach, in 198 patients in the duodenum 12.Emergency EGFDS for verification of the source of bleeding and implementation of hemostasis in all examined patients under local anesthesia with 10% lidocaine solution was carried out by us using gastroduodenoscopes EVIS-130, XQ-30 from Olympus (Japan) and endoscopic video system OTV-2, instrumentation of the same firms (catheters PR-8Q, PR-10Q, PR-11Q). At the same time, Olympus GIF series fibro-gastroscopes made it possible to visualize a bleeding ulcer, both through the eyepiece and on the monitor screen. In severe patients with unstable hemodynamics, this study was carried out in the shock ward or in the intensive care unit.Acute ulcers were observed in 283 patients during EGFDS, and in 130 patients, chronic ulcerative process. Moreover, in 215 patients, ulcers were located in the stomach, in 198 patients in the duodenum 12.We established the activity of the existing bleeding from gastroduodenal ulcers according to the endoscopic classification of Forrest J.A. (1974). At the same time, we evaluated the results obtained taking into account the nature and localization of gastroduodenal ulcers. So, in 86 patients, ulcerative bleeding at the time of endoscopy continued. At the same time, 11 of them had jet, arterial bleeding (F 1 A), and in 75 patients blood was sucked in the form of venous bleeding (F 1 B) In 57 cases, continued bleeding was observed from acute, and in 29 cases from chronic gastroduodenal ulcers. We established the activity of the existing bleeding from gastroduodenal ulcers according to the endoscopic classification of Forrest J.A. (1974). At the same time, we evaluated the results obtained taking into account the nature and localization of gastroduodenal ulcers. So, in 86 patients, ulcerative bleeding at the time of endoscopy continued. At the same time, 11 of them had jet, arterial bleeding (F 1 A), and in 75 patients blood was sucked in the form of venous bleeding (F 1 B) In 57 cases, continued bleeding was observed from acute, and in 29 cases from chronic gastroduodenal ulcers.In 323 patients, during endoscopic interventions, ulcerative bleeding was stopped. At the same time, an ulcer covered with a loose, red thrombus (F2 A) was diagnosed in 180 cases, a gray, fixed thrombus (F2 B) in 122 cases. In 21 cases, ulcers were covered with fibrin, and small thrombi (F2 C) were detected around them, which indicated the reliability of hemostasis (Fig. 1, 2). In 4 patients, the presence of gastroduodenal ulcers without signs of bleeding was found during EGFDS (F3).
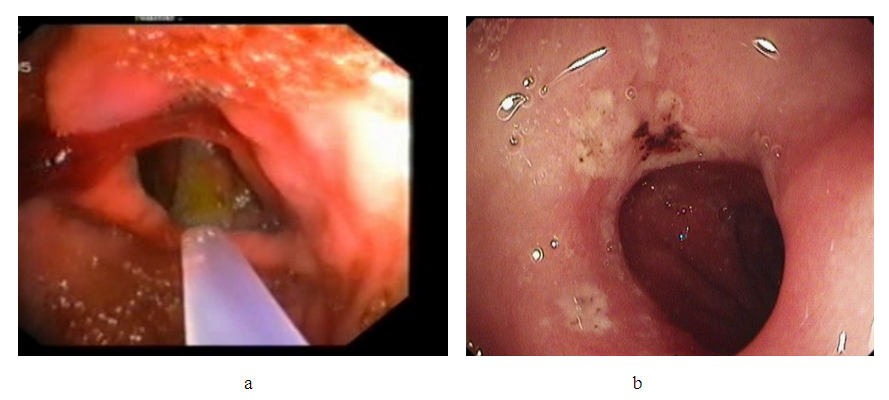 | Figure 1. Endophotogram: ulcerative bleeding according to F1A (a) and F1B (b) |
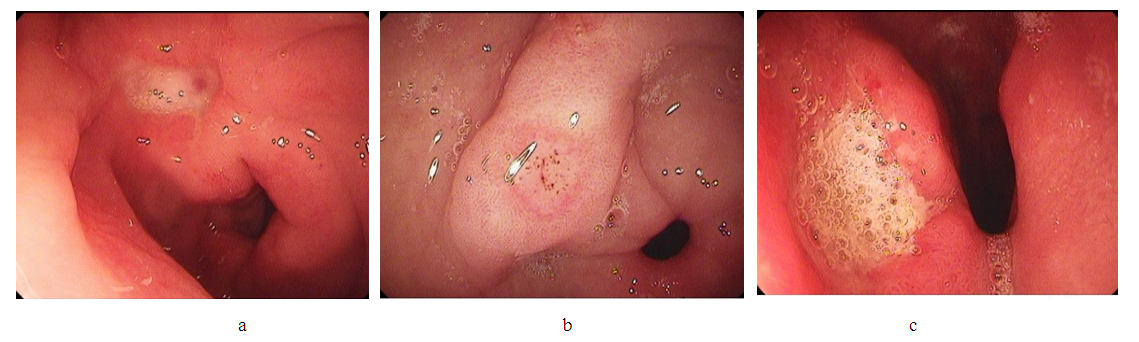 | Figure 2. Endophotogram: ulcerative bleeding according to F2A (a), F2B (b), F2C (c) |
3. The Results of the Research
- Depending on the nature and intensity of ulcerative gastroduodenal bleeding, assessed with EGDFS according to the Forrest classification, according to the generally accepted tactics, we used various methods of endoscopic hemostasis in 301 (72.9%) patients as the primary method of hemostasis, as well as prophylactic antiulcer and hemostatic conservative therapy in 112 (27.1%) patients with completed bleeding according to F2B, F2C and F3 (Fig. 3).
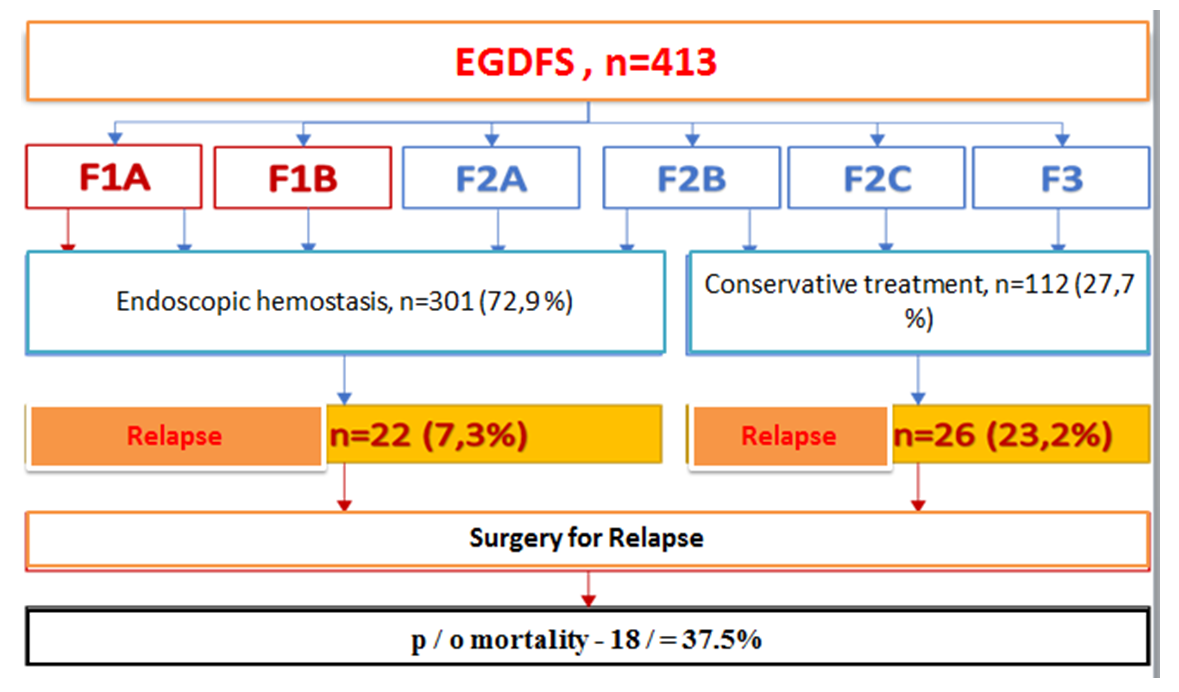 | Figure 3. The effectiveness of the primary methods of hemostasis |
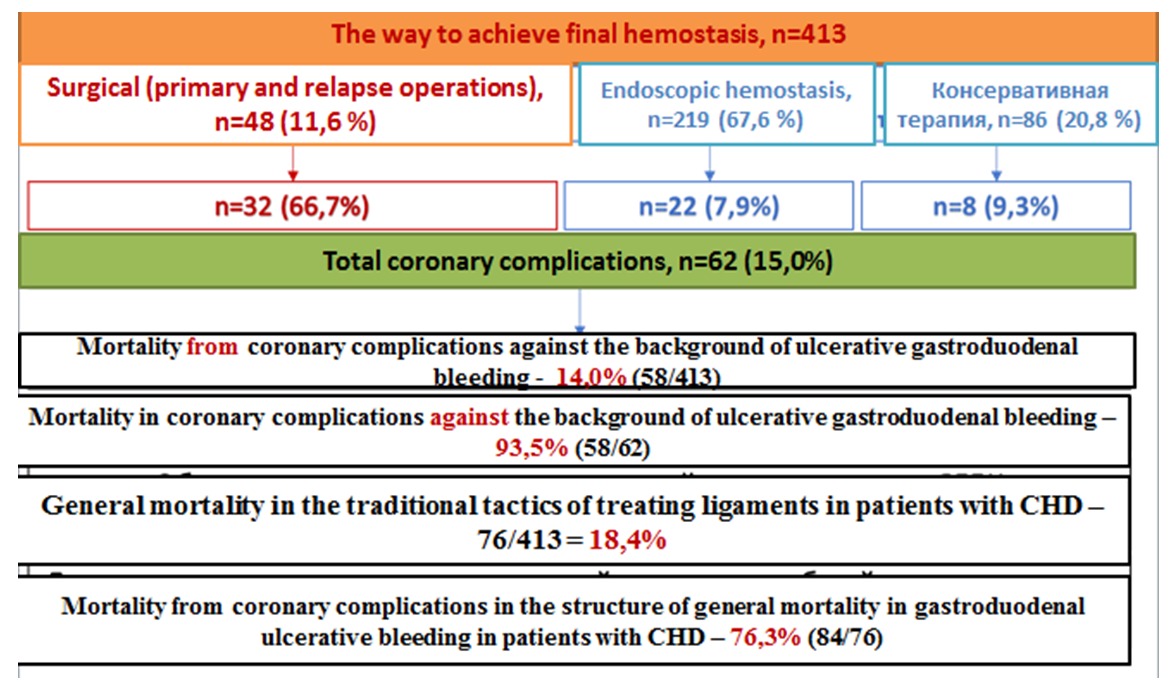 | Figure 4. Mortality from coronary complications in gastroduodenal ulcer bleeding in patients with coronary heart disease |
4. Discussion of the Results
- Summarizing all the results obtained, it should be noted that although all patients with ulcerative gastroduodenal bleeding with coronary heart disease followed the generally accepted clinical and endoscopic treatment tactics, however, in the practical interpretation of approaches to it in terms of the implementation of ulcerative hemostasis, there were peculiar features. Depending on this, the tactics of treatment in the examined patients gastroduodenal ulcer bleeding with ischemic heart disease varied from cautious, predominantly conservative, to more aggressive, predominantly active surgical.The predominantly conservative tactics in the implementation of ulcerative hemostasis assumed a wider use of drug therapy and the possibilities of traditional endoscopic methods. The use of this tactic of treatment was justified by the desire to minimize the effect on coronary circulation of concomitant coronary heart disease. In contrast, the predominantly active surgical tactics involved the implementation of ulcerative hemostasis with extensive use of the possibilities of endoscopic and surgical interventions.The obtained results of treatment indicate that the use of both tactical approaches in patients with ulcerative gastroduodenal bleeding with coronary heart disease was accompanied by the development of various complications that worsen the outcome of the disease.This circumstance prompted us to search for ways to expand the indications for endoscopic hemostasis, increase its reliability and safety, revise traditional intensive care regimens with a greater emphasis on the prevention and treatment of acute coronary syndromes, personalize the choice of treatment tactics for ulcerative bleeding in patients with shemic heart disease based on reliable scales for predicting the severity of gastroduodenal ulcerative bleeding in patients with shemic heart disease.
5. Conclusions
- Thus, concluding all the above data, it can be stated that the applied conventional tactics for the treatment of ulcerative bleeding with concomitant ischemic heart disease, due to its limitations, turned out to be insufficiently effective.This tactic provided for either excessive conservatism in the treatment of ulcerative bleeding accompanied by a large number of their relapses, or excessive surgical activity of ulcerative hemostasis leading to an increase in coronary complications from concomitant ischemic heart disease.In this regard, there is currently an urgent need to develop and apply in practice improved tactics of treatment of ulcerative gastroduodenal bleeding combined with various forms of ischemic heart disease based on an integral objective assessment of the patient's condition, as well as predicting the severity of these combined pathologies in each specific clinical situation.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML