-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(5): 367-372
doi:10.5923/j.ajmms.20211105.03
Received: Apr. 11, 2021; Accepted: Apr. 30, 2021; Published: May. 7, 2021

Off-pump Coronary Artery Bypass Graft in Patients with Multi-vessel Coronary Artery Disease
Abdurakhmanov A. A., Anvarov Kh. E.
Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the study was retrospective analysis of the single center experience with off-pump coronary artery bypass graft in patients with multivessel coronary artery disease. Introduction. Surgical revascularization in patients with multi-vessel coronary artery disease still raises many questions. Material and methods. This retrospective study includes 1221 patients with coronary artery disease operated in the department of cardiac surgery in the Republican Research Center of Emergency Medicine in 2013-2020. 1000 patients (81.9%) were male and 221(18.1%) female, average age 56.2 ± 0.9 years. Results. In the early postoperative period 41 patients died, hospital mortality was 3.3%. In 60 cases off-pump to on-pump coronary artery bypass graft conversion was made (conversion rate – 4.9%). In the univariate analysis, we observed that a history of acute myocardial infarction, diabetes mellitus, and COPD were not a risk factor for death, while an unstable state on admission (OC 15.38, CI -4.86-48.6 p0.0001) and conversion to on-pump for emergency indications (OR - 30.25, CI - 9.46 - 96.7, p<0.0001) can be considered reliable risk factors for the development of the lethal outcome in the early postoperative period, a low ejection fraction also showed a high probability of a mortality, but the variables were not statistically significant (OR = 1.07, CI = 0.44-2.57, p = 0.88). Follow-up was completed in 89.9% (1098 of 1221 patients) of the patients. During the follow-up period (2-48 months on average 24.1 ± 0.34), 12 (1.1%) patients died. Freedom from the combined endpoint of cardiac death and myocardial infarction, was 97.1% at 40 months; freedom from recurrent angina was 92.3% and freedom from repeated revascularization was 99.1%. Conclusion. Patients with multivessel coronary disease and unstable angina in most cases can undergo to off-pump coronary artery bypass graft with favorable early results. Haemodynamical problems can force surgeon to turn on-pump. Emergent on pump conversion following haemodynamical instability can be a significant factor for mortality. In our series coronary artery bypass graft surgery showed favorable immediate and mid-term results.
Keywords: Coronary artery bypass graft, Coronary artery disease, Off-pump coronary artery bypass graft
Cite this paper: Abdurakhmanov A. A., Anvarov Kh. E., Off-pump Coronary Artery Bypass Graft in Patients with Multi-vessel Coronary Artery Disease, American Journal of Medicine and Medical Sciences, Vol. 11 No. 5, 2021, pp. 367-372. doi: 10.5923/j.ajmms.20211105.03.
1. Introduction
- Coronary artery bypass grafting (CABG) occupies a special place in the treatment of coronary heart disease (IHD). Its effectiveness in eliminating the symptoms of angina pectoris, and increasing the life expectancy in some patient groups is currently undeniable. There are two methods of surgical revascularization of the cardiovascular system: a standard procedure of CABG with the use of cardiopulmonary bypass (on-pump), and CABG on beating heart (off-pump) [1-2]. Since the late 1990, beating heart CABG has become increasingly popular, as a result of introduction in clinical practice of devices that stabilize the heart for the application of anastomosis [1-4]. In the literature and modern periodical publications, we can note an active discussion about how, whichever method is preferred. A number of authors indicate a low efficiency of off-pump CABG associated with the risk of incomplete revascularization, and as a consequence of perioperative myocardial infarction and late graft failure [1,5-8]. Other authors emphasize the absence of statistically significant differences in the mortality rate, postoperative complications, infarction and stroke in the postoperative period, as well as other advantages and disadvantages when comparing both methods, emphasizes the same duration of functioning of shunts in the long-term follow-up period [3,9-10]. Other researchers pay attention to the efficacy and safety of the method on the beating heart, both in patients with low and high risk [2,11-12]. In particular, according to the latest publications, off pump myocardial revascularization is accompanied by a short period of stay in the intensive care unit, a reduction in ventilation time and hospitalization, a low rate of atrial fibrillation, blood transfusions compared to conventional CABG, a low requirement for inotropic support, low incidence of respiratory tract infections, stroke, delirium and postoperative myocardial infarction [11,13-15].The aim of the study was a retrospective analysis of the single center immediate and mid-term results of off-pump CABG in patients with multivessel coronary artery disease.
2. Material and Methods
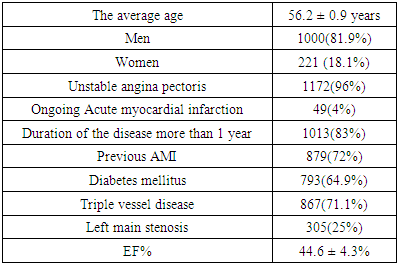
- This retrospective study includes 1221 patients with coronary artery disease (CAD) operated in the department of cardiac surgery in the Republican Research Center of Emergency Medicine in 2013-2020. 1000 patients (81.9%) were male and 221(18.1%) female, average age 56.2 ± 0.9 years. The initial patients data are shown in Table 1.
|
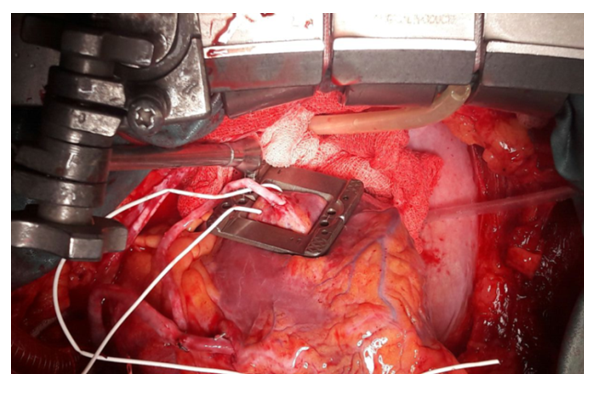 | Figure 1. Intraoperative photo. Autovenous bypass on the Cx artery using stabilizer and deep pericardial stitches |
3. Results
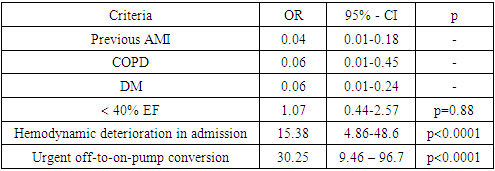
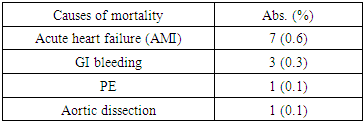
- The immediate results of the hospital period, including hospital mortality and complications of the postoperative period were evaluated. In the early postoperative period, 41 patients died, hospital mortality was 3.3%. Among the causes of mortality there were perioperative myocardial infarction – 15(1.2%); low cardiac output syndrome – 21(1.7%), complex rhythm disturbances - 7(0.6%); pulmonary artery embolism – 3 (0.2%) and stroke – 1(0.1%) (some patients suffered two or more complications, leading to mortality). In 60 cases, off-pump to on-pump CABG conversion was made (conversion rate –4.9%), of which, in 29 (2.4%) cases, the conversion was made urgently due to severe haemodynamical destabilization. In the remaining 31 (2.5%) patients, the conversion was performed in a planned manner for anatomical reasons, due to the inaccessibility of the vessels or large left ventricle. In the univariate analysis, we observed that a history of acute myocardial infarction, diabetes mellitus, and COPD were not a risk factor for death, while an unstable state on admission (OC 15.38, CI -4.86-48.6 p0.0001) and conversion to on-pump for emergency indications (OR - 30.25, CI - 9.46 - 96.7, p<0.0001) can be considered reliable risk factors for the development of the lethal outcome in the early postoperative period, a low ejection fraction also showed a high probability of a mortality, but the changes were not statistically significant (OR = 1.07, CI = 0.44-2.57, p = 0.88) (Table 2).
|
|
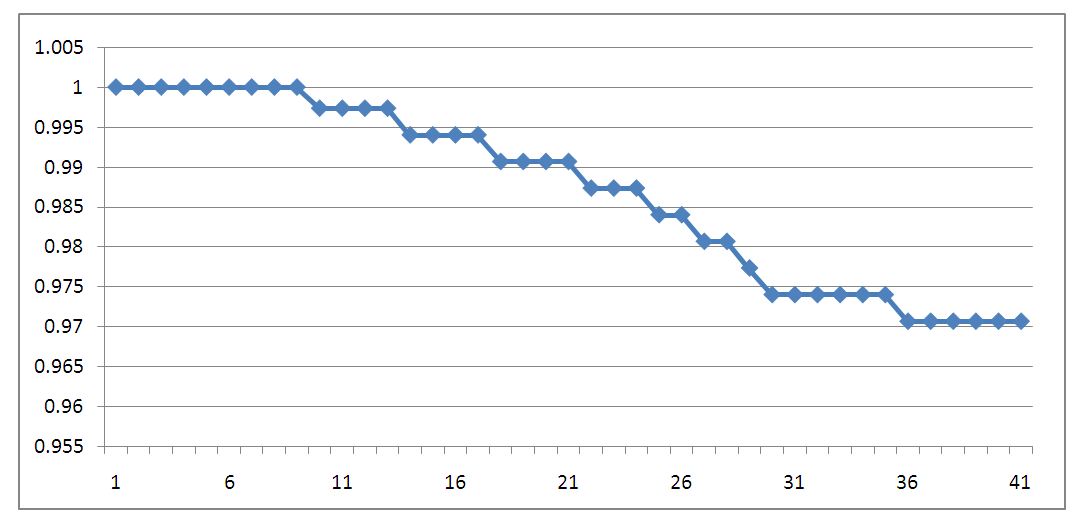 | Figure 2. Kaplan-Meier curve - survival of patients in the 40 month follow-up period |
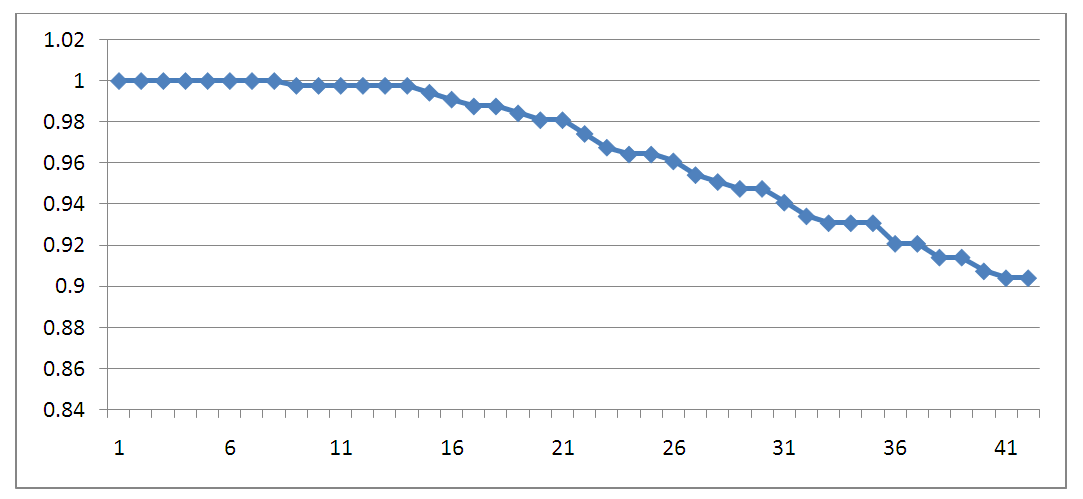 | Figure 3. Kaplan-Meier curve - freedom from the recurrence of angina pectoris |
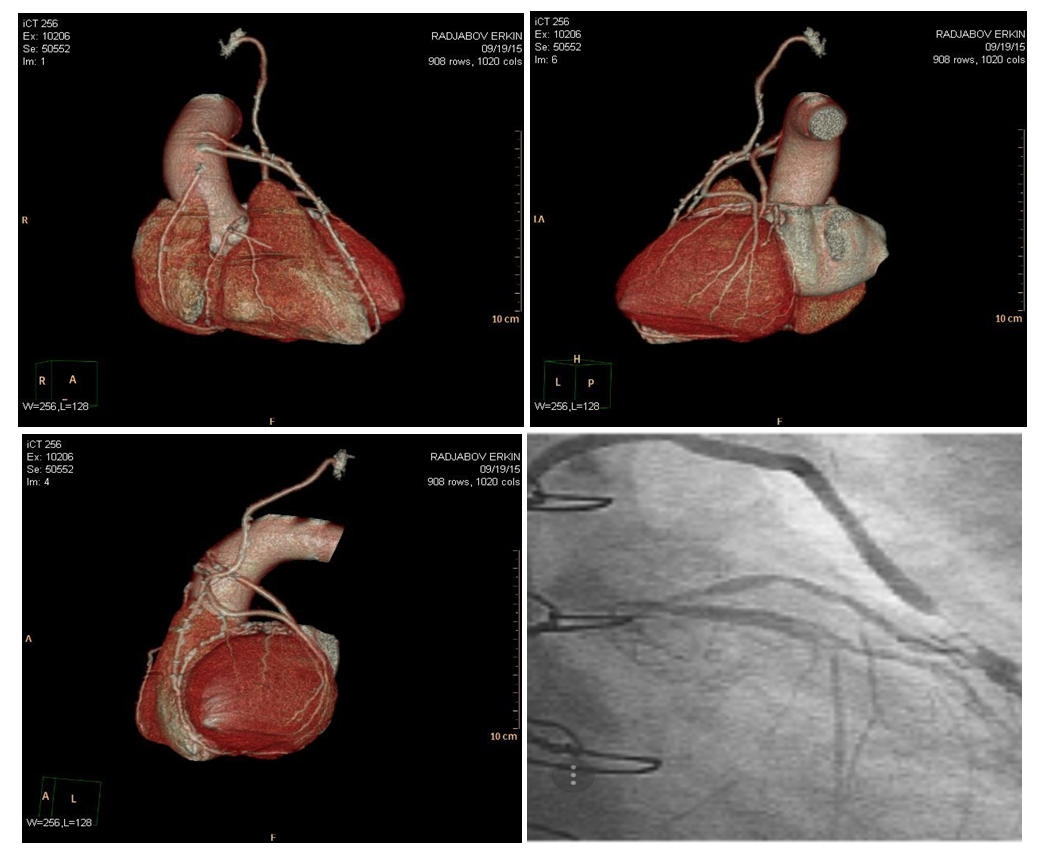 | Figure 4. MSCT coronary angiography allows assessing the state of grafts |
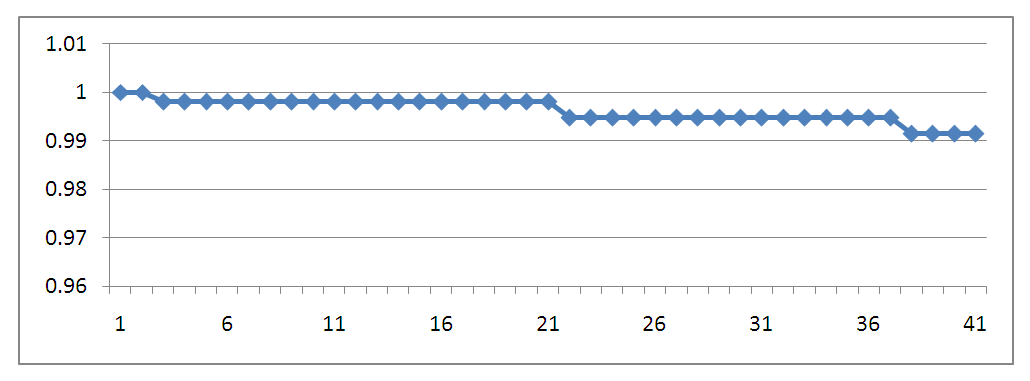 | Figure 5. Kaplan-Meier curve - freedom from repeated revascularization |
4. Discussion
- Since its invention in 1960 coronary artery bypass grafting has been a standard procedure in treatment of multiple coronary artery stenosis. Off-pump CABG technique can reduce the morbidity associated with cardiopulmonary bypass, which can lead to severe systemic inflammatory responses [1,16-18]. Some recent studies and meta-analyses have proven the safety and effectiveness of OPCAB with favorable early outcomes and has described OPCAB as a safe alternative to conventional CABG, regarding to death rate and postoperative morbidity [1,11,14,12,19]. On the other hand, many authors have underlined that off-pump surgery can lead to incomplete revascularization [5-7,20]. Some studies have showed that [1,6-7,18] the mean number of bypass grafts in off-pump patients was significantly smaller than that in on-pump patients. Complete myocardial revascularization is one of the important goals of CABG, although the definition of completeness differs among studies. Kleisli and colleagues [20] demonstrated that the 5-year survival rate of complete revascularization was superior to that of incomplete revascularization (82.4% versus 52.6%). In their report, the anatomic reasons for incompleteness were small, such as severely diseased, arteries, nondominant right coronary artery, the presence of prior infracted tissue, significant collateral circulation, and lack of conduit availability. In our series 5 year survival after off-pump CABG was 97,1%. Toshihiro Fukui and colleagues have revealed that the number of distal anastomoses per patient (3.6±1.4) in their study was similar to that in the on-pump patients [17], and complete revascularization was achieved in 99.2% of patients. In the present study the number of distal anastomoses per patient (3.6) was the same as in Toshihiro Fukui’s study. We can state that complete myocardial revascularization using an off-pump technique can be safely performed, and this method is fully reproducible. Despite the fact that early outcome shows excellent results, there are still lack of information on the midterm and long-term outcomes after OPCAB [2-5,17]. Sabik and colleagues [19] in their work described the equivalent midterm outcomes after off-pump and on-pump CABG, 4-year survival after OPCAB was 87.5%. The results of the present study, with a 40 month survival rate and freedom from cardiac death of 97.1% ± 0.6%, are almost identical to those of previous studies. The reduction of graft patency can increase the need for repeat revascularization with time. Puskas and coworkers [21] revealed that graft patency in OPCAB patients is similar to that in conventional CABG patients at 30 days (99.0% versus 97.7%) and 1 year (93.6% versus 95.8%) after surgery. In present study 90,4% of patients complained on angina recurrence, but overall early graft patency rate was 99.1% what is almost identical to their results. Based on our results we suppose that the same early graft patency rate can be obtained in patients treated with OPCAB as compared with those undergoing conventional CABG. Some investigators stated that SVG is associated with reduced patency rate in patients undergoing OPCAB [22]. In present work most grafts were SVG it means that even SVG can demonstrate good mid-term patency. There are still some patients who cannot be treated with OPCAB, such as those with a large heart and impaired left ventricular function or intramyocardial coronary arteries, which sometimes can lead to off-pump to on-pump conversion. Recent studies revealed that off-pump to on-pump conversion can be performed in 5-10% of all cases [23-25]. The rate of performing OPCAB in our isolated CABG patients was 90,8% and overall conversion rate was 9,2% with 55,7% cases being converted urgently due to haemodynamical disturbances. Some studies have underlined that conversion can be an independent risk factor for mortality in early postoperative period [25-26]. Our findings also support these data, mortality rate were higher among urgently converted patients. A recent meta-analysis clearly revealed the favorable outcomes of OPCAB [1,18], and concluded that OPCAB should be considered a safe alternative to conventional CABG with respect to mortality risk. Similar completeness of myocardial revascularization and graft patency can be achieved by OPCAB procedures using modern technology and techniques. Thus, we suggest that OPCAB should be performed whenever possible in patients undergoing isolated CABG.
5. Conclusions
- Patients with multivessel coronary disease and unstable angina in most cases can undergo to off-pump CABG with favorable early results. Anatomical peculiarities and haemodynamical problems can force surgeon to turn on-pump. Emergent on pump conversion following haemodynamical instability can be a significant factor for mortality. In our series CABG showed favorable immediate and mid-term results. MSCT can be informative method to assess patients with recurrence angina.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML