Abdullaeva Kh. N., Nazirova L. A., Ablyalimov I. T.
Republican Specialized Scientific and Practical Medical Centre of Surgery, Named after Acad. V.Vakhidov, Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
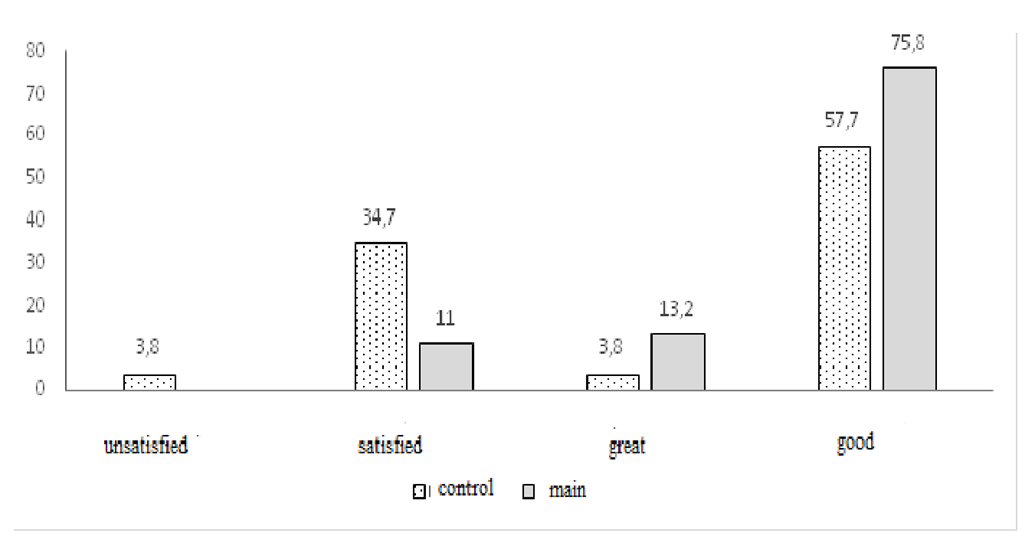
Anesthesia of the transverse abdominus plane block (TAR-block) is a new approach to blocking the afferent nerves of the anterior abdominal wall through the introduction of a local anesthetic. The efficacy and safety of this technique has been evaluated in patients with various allohernioplasty options. A comparative analysis of the analgesic efficacy of the TAP block was carried out in 25 patients (main group) aged 58.9 ± 4.0 years under standard spinal anesthesia (SA) with a 0.5% bupivacaine solution at a dose of 10-15 mg. The control group (n = 26) consisted of patients identical in gender, age, nature and time of surgery, anesthesia. Blood pressure (BP), systolic (SBP), diastolic (DBP) and mean (ABP), heart rate (HR), respiratory rate (RR), saturation (SpO2), ECG were monitored intraoperatively and in the immediate postoperative period. The dynamic analysis of the course of the immediate postoperative period and pain relief was assessed by monitoring the pain perception scores VAS and NRS at rest and during movement (1-2-4-8-12-24 hours after the operation), changes in blood pressure avg., Heart rate, the level of SpO2 and NPV, the need for used non-narcotic and narcotic analgesics, recording the time to the first requirement of anesthesia and the frequency of its administration. The number of postoperative complications in the form of nausea and vomiting, satisfaction with pain relief was recorded.Analysis of the dynamics of the degree of pain perception showed the effectiveness of TAP block anesthesia both in the first hours after surgery and during the next 24 hours. The difference in scores between groups was statistically significant, however, we were unable to completely eliminate additional pain relief. In a comparative aspect, it was found that in the next 24 hours after the operation, blood pressure cf. and heart rate practically at all stages of observation were statistically significant (p <0.001) lower on average by 7.9% and 6.6%, respectively, compared with the control. Dynamic control of saturation and NPV did not reveal significant deviations from the permissible values, the differences between the groups were not significant, the SpO2 and NPV levels remained stable and ranged from 96.20 ± 0.28 to 98.60 ± 0.10 % and 14.38 ± 0.18 to 15.69 ± 0.14 breaths per minute respectively. Comparative assessment of the degree of satisfaction of patients from the performed anesthesia showed that 3.8% of patients in the control group were not satisfied with the postoperative pain relief, 34.7% - noted satisfaction, 57.7% - noted as good and 3.8% - excellent. Different numbers were determined in the main group, where the percentage of satisfactory pain relief was 11%, good - 75.8%, excellent - 13.2%. Thus, the analysis of the efficacy and safety of the TAP block in the protocol of postoperative anesthesia in patients after allohernioplasty performed under CA conditions established that the use of an interfascial block using ultrasound navigation is a guaranteed procedure without complications. The TAP block provided effective and prolonged postoperative analgesia compared to standard therapy.
Keywords:
Anesthesia, TAP block, Alloherniplasty, Postoperative anesthesia
Cite this paper: Abdullaeva Kh. N., Nazirova L. A., Ablyalimov I. T., Assessment of the Effectiveness and Safety of the Tap-Block for Postope-Rational Painfulness in Patients with Allohernioplastics, American Journal of Medicine and Medical Sciences, Vol. 11 No. 4, 2021, pp. 340-345. doi: 10.5923/j.ajmms.20211104.17.
1. Introduction
Rational postoperative pain relief is a mandatory measure of any surgical intervention, including after alloherniplasty. Following the requirements of modern medicine, aimed at the fastest possible activation of patients, as well as to improve the quality of the operation and the comfort of the postoperative period, various options for pain relief are offered [1,2].Recently, the use of fascial-sheath regional analgesia has been expanding, including the transversus abdominis plane block (TAP block), due to its anatomical and physiological advantages, it seems promising. [5.6]. Despite the seeming routine of the recommendations for using the TAP block for postoperative pain relief, the safety of this variant of analgesia began to appear only after the introduction of ultrasound (US) assisted methods for this manipulation in recent years [3,7,12,13].Having our own experience of using the TAP block for postoperative analgesia of patients who underwent various variants of allohernioplasty, it was decided to analyze the effectiveness and safety of this technique in this group of patients, which was the purpose of the presented message.
2. Materials and Methods
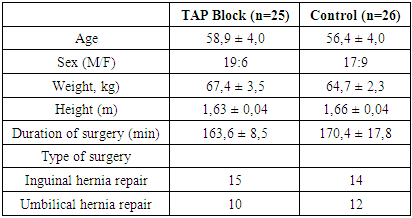
A comparative analysis of the analgesic efficacy of the TAP block was carried out in 25 patients (main group) aged 58.9 ± 4.0 years, husband 19, wives 6, after allohernioplasty for inguinal (15) and umbilical (10) hernias under conditions standard spinal anesthesia (SA) with a 0.5% bupivacaine solution at a dose of 10-15 mg.The control group (n = 26) consisted of patients identical in sex, age, nature and time of surgery, anesthesia, differing only in the use of traditional postoperative analgesia with non-steroidal anti-inflammatory drugs (NSAIDs) (Analgin 500mg - 1000mg., Baralgin 500mg - 1000mg, Ketoprofen 50 mg - 100 mg) and narcotic - Promedol 2% -1.0 in age dosages.Table 1. Clinical characteristics of patients
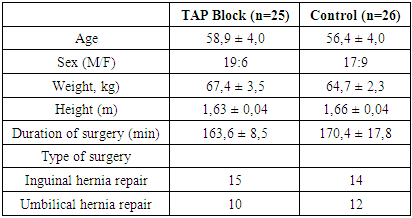 |
| |
|
Blood pressure (BP), systolic (SBP), diastolic (DBP) and mean (ABP), heart rate (HR), respiratory rate (RR), saturation (SpO2), ECG were monitored intraoperatively and in the immediate postoperative period. After the end of the operation and suturing of the skin in the main group, under ultrasound control, a unilateral classic TAP block was performed on the side of intervention for inguinal hernias, while for umbilical hernias, a bilateral TAP block was performed. The procedure was performed under ultrasound control using a Logic P6 apparatus, GE (USA) using an 11 L MHz linear transducer.First, in two mutually perpendicular planes in the transverse and sagittal (longitudinal), ultrasound anatomical structures of the zone of interest were visualized to determine the depth of their location from the skin surface.The imaging depth was from 4 to 6 cm, the sensor was positioned in the horizontal plane along the mid-axillary line, three layers of muscles of the anterior abdominal wall were identified transversely to the abdominal wall between the costal edge and the iliac crest, with the removal of the space between the internal oblique and transverse muscles.Further dynamic ultrasound scanning was carried out under sterile conditions in the selected area, when the tip of a 100 mm needle with a short cut was fixed in real time, followed by navigation of its advance using the in-plane or out-of-plane technique. The needle was inserted in the sagittal plane approximately 3–4 cm medial to the location of the ultrasound probe with optimal control of its tip. At first, the sensor was installed somewhat medial to the mid-axillary line to control the skin puncture and determine the initial direction of the needle, followed by its gradual retraction posteriorly to the mid-axillary line in order to correct the needle reaching into the transverse space. The fixation of the local anesthetic was also monitored by visualization with an ultrasound transducer, which made it possible to determine in real time not only the course of the needle, but also the administration of the local anesthetic. The blockade of peripheral nerves was provided by injection of 20 ml of local anesthetic solution bupivacaine 0.25% -20.0 into the fascial sheath, in which the peripheral nerves are located, achieving the effect of "drowning" them in the injected solution. A step-by-step protocol for performing a TAP block with ultrasound navigation provided a guarantee of the safety and quality of regional anesthesia. The effect of the TAP block on the procedure was assessed by the severity of pain syndrome at rest 20 minutes after the injection of local anesthetic using a visual analogue pain scale (VAS) and a digital pain rating scale (NRS). There were no complications associated with the TAP block. After surgery, all patients were transferred to specialized departments, where they were observed and treated before discharge from the hospital. The dynamic analysis of the course of the immediate postoperative period and pain relief was also assessed by monitoring the points of pain perception VAS and NRS at rest and during movement (1-2-4-8-12-24 hours after the operation), changes in hemodynamic parameters of blood pressure Wed, heart rate, SpO2 and NPV levels, the need for used non-narcotic and narcotic analgesics, recording the time before the first requirement for anesthesia and the frequency of its administration. The number of postoperative complications in the form of nausea and vomiting, discomfort, and satisfaction with pain relief was recorded.
3. Results and Discussion
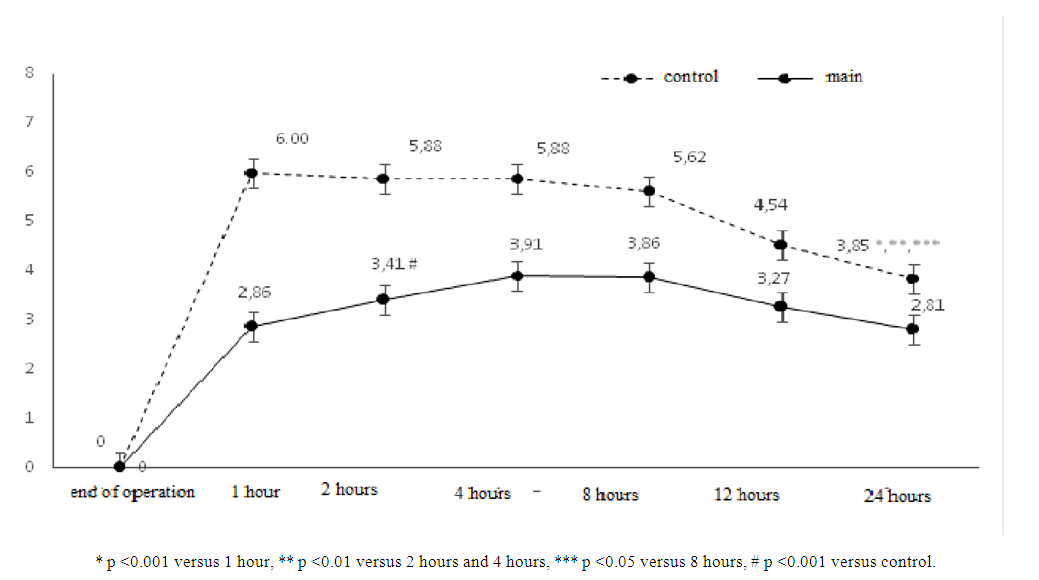
The study of the degree of pain perception in both groups showed that an hour after the end of the operation in patients who received the TAP block, the VAS and NRS scores were 2.86 ± 0.28 (mild pain), while in the control group, where there was no the TAP block was used, patients noted pain sensations corresponding to 6.0 ± 0.13 points (severe pain) (p <0.001) (Fig. 1). Given the severity of pain in the comparison group, the patients already in the first hours after the operation required anesthesia, which was carried out with non-narcotic analgesics (Analgin 500-1000 mg, Baralgin 500-1000 mg).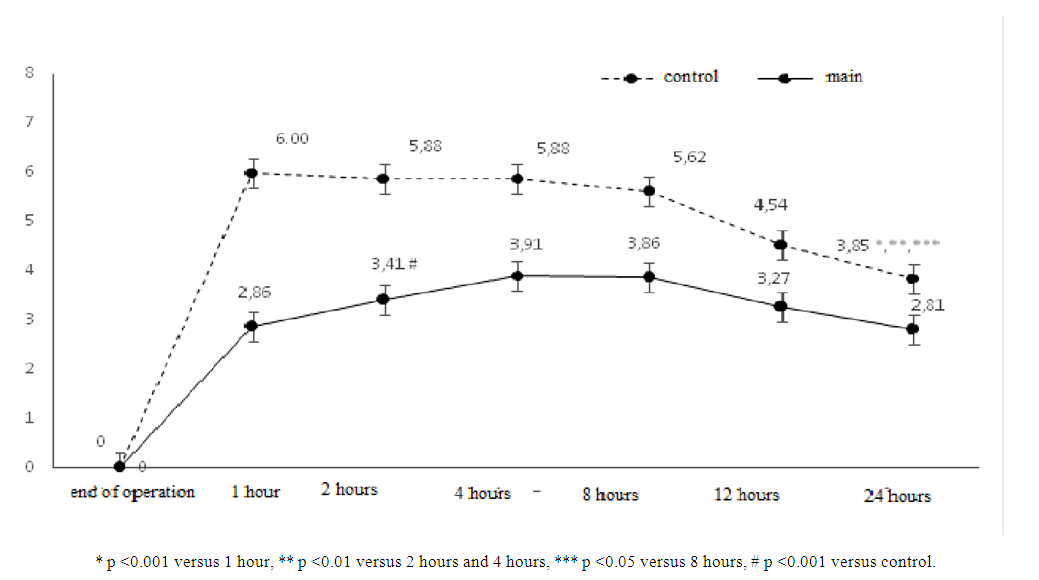 | Figure 1. The effectiveness of pain relief according to VAS |
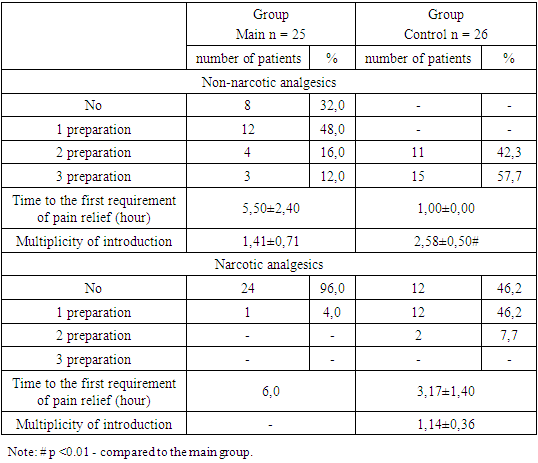
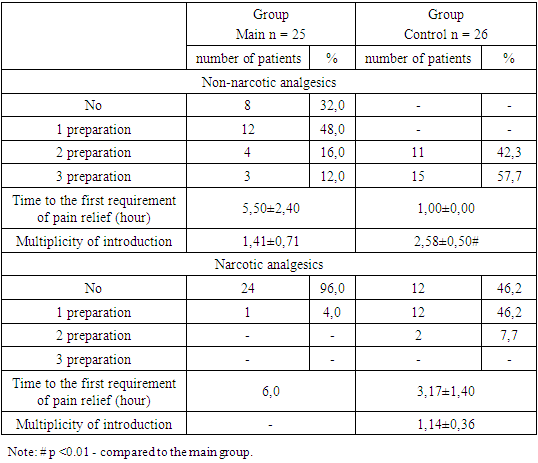
Such a significant difference in pain perception in the groups was explained by a decrease in the effects of SA, which was leveled by the applied fascial-sheath regional analgesia in the main group [9,11].The time to the first requirement of an anesthetic NSAID drug in patients in the comparison group was 1.00 ± 0.01 hours, however, it was not possible to obtain sufficient effective pain relief for these patients. Despite anesthesia, after 2 hours the number of points of pain perception in the control group was 5.88 ± 0.23 (severe pain), while in the main group it was 3.41 ± 0.35 points (- moderate), the difference of which was statistically significant (p <0.001). Patients in the main group experienced mild to moderate pain and did not need additional anesthesia.In the next 4-8 hours of observation, the dynamics of pain in the groups did not change and there was a significant difference in points between the groups (p <0.001). The patients of the main group remained active throughout this period, did not complain of discomfort and did not need additional anesthesia, which was required in a number of patients only 6 hours after the end of the operation. A completely opposite picture took place in the control group, in which the preservation of pain sensations required extended anesthetic measures in patients in the form of repeated administration of NSAIDs with a more effective effect, up to the use of narcotic analgesics already 3 hours after suturing the skin (see Table. 2).Table 2. Consumption of analgesics in groups
 |
| |
|
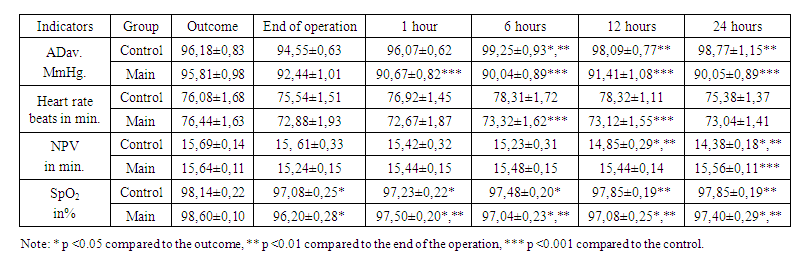
A detailed examination of the consumption of painkillers showed that in the main group, in the postoperative period, 32% (8) patients were not injected with NSAIDs, 12 (48%) patients used non-narcotic analgesics once, 16% (4) - twice, and 12% (3) - were anesthetized three times. In the control comparison group, on the contrary, all patients received non-narcotic analgesics two and three times already one hour after the operation. The frequency of administration of drugs in this group was almost two times higher than that in the main group (p <0.001). Pain relief with narcotic analgesics also differed twofold in the studied groups, as 96% (24) of patients who used the TAP block did not receive opioids, while in the control group only 46.2% of patients (12) did not need narcotic analgesics. Narcotic analgesics were administered once to only one patient in the main group versus 12 (46.2%) patients in the control group, where 7.7% (2) received opioids twice. The time to the first demand for drug pain relief was 6.0 hours in the main group versus 3.17 ± 1.4 hours in the comparison group. The applied tactics of postoperative anesthesia contributed to a decrease in pain perception after 12 hours from strong to moderate in the control group (NRS score 6.0 ± 0.13 to 4.54 ± 0.16 p <0.001) while maintaining a significant difference in scores in the groups. 24 hours after the operation, the level of pain perception decreased to weak in the main group 2.81 ± 0.15 and moderate in the control group 3.85 ± 0.17.Thus, the analysis of the dynamics of the degree of pain perception showed the effectiveness of pain relief with the TAP block both in the first hours after the operation and during the next 24 hours. The difference in scores between the groups was statistically significant; however, unfortunately, we were unable to achieve complete exclusion of additional anesthesia in patients after allohernioplasty performed under SA conditions using the TAP block.Observation of the course of the postoperative period revealed that the hemodynamic parameters of blood pressure mean, heart rate immediately after suturing on the skin were the same in the groups and were at a normal level, making up, respectively, in the control - 94.55 ± 0.63 mm Hg. st. and 75.54 ± 1.51 beats in min. in the main group - 92.44 ± 1.01 mm Hg. and 72.88 ± 1.93 beats. in min. (see Table 3).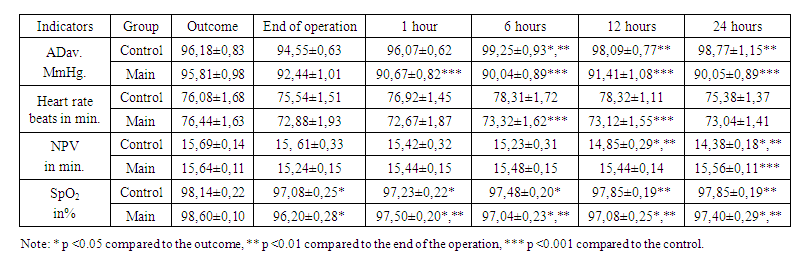 | Table 3. Indicators of hemodynamics and gas exchange at the stages of the study |
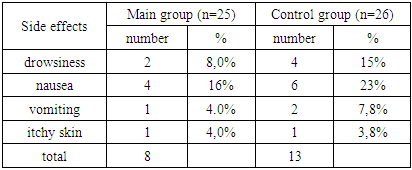
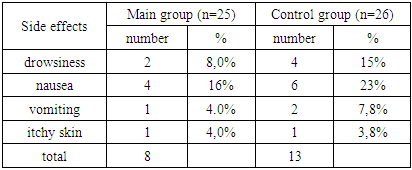
In the future, as the pain intensifies, 6 hours after the end of the operation in patients of the control group, ADav. increased tцёo numbers 99.25 ± 0.93 mm Hg, heart rate - 78.31 ± 1.72 beats. in minutes, despite the active pain relief measures. In the main group, we did not observe such a hyperdynamic reaction of the blood circulation MAP. and heart rate was stable and ranged from 90.04 ± 0.89 to 91.41 ± 1.08 mm Hg. and 72.88 ± 1.93 to 73.32 ± 1.62 beats. in min. respectively. In a comparative aspect, it was found that in the next 24 hours after the operation, blood pressure cf. and heart rate practically at all stages of observation were statistically significant (p <0.001) lower on average by 7.9% and 6.6%, respectively, compared with the control.Dynamic control of saturation and NPV for the entire observation period did not reveal significant deviations from the permissible values, significant intragroup changes were identical and depended on perioperative stages, the differences between the groups were not significant, the levels of SpO2 and NPV remained stable and ranged from 96, 20 ± 0.28 to 98.60 ± 0.10% and 14.38 ± 0.18 to 15.69 ± 0.14 breaths per minute. Nevertheless, observation of patients showed that the use of the TAP block for postoperative analgesia had its advantages, since it reduced pain perception to a better degree and, accordingly, manifested itself in lower responses of the body. The leveling of pain intensity, in turn, contributed to a decrease in the frequency of additional pain relief and decreased the number of side effects of analgesics, as well as increased comfort for patients and allowed their early activation. [4,10].In addition, it is known that the elimination of the pain syndrome after surgery should be carried out as soon as possible, using the most adequate means and methods available at the present stage of development of medicine, since it has been proven that pain that persists after surgery is an unfavorable prognostic factor that has a negative effect on the course of the postoperative period and patient rehabilitation. [8,12].Table 4 shows the postoperative complications that occurred in the groups during the observation, where it can be seen that the number of side effects in patients who received the TAP block was almost two times lower than in the control group.Table 4. The number of side effects in the immediate postoperative period by group
 |
| |
|
Comparative assessment of the degree of patient satisfaction in relieving postoperative pain showed (see Fig. 2) that 3.8% of patients in the control group were not satisfied with the postoperative pain relief, 34.7% noted satisfaction, 57.7% noted how good and 3.8% excellent. Different numbers were determined in the main group, where the percentage of satisfactory pain relief was 11%, good - 75.8%, excellent - 13.2%.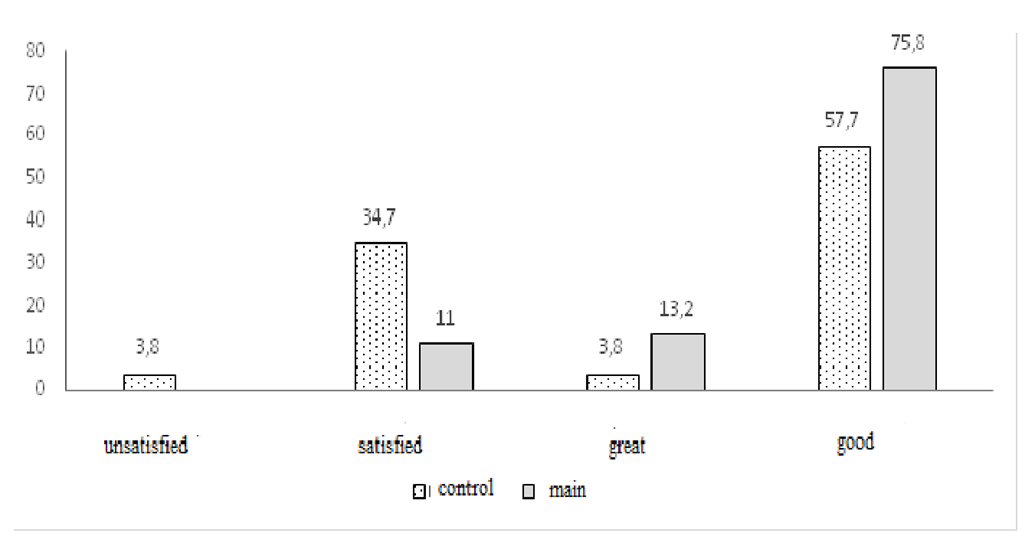 | Figure 2. Assessment of patient satisfaction with anesthesia |
Thus, the analysis of the efficacy and safety of the inclusion of the TAP block in the protocol of postoperative anesthesia in patients after allohernioplasty performed under CA conditions established that the use of an interfascial block using ultrasound navigation is a guaranteed procedure without complications. TAP block provided effective and prolonged postoperative analgesia compared to standard therapy. The available advantages of this type of analgesia were represented by a decrease in pain, postoperative stress reactions, fewer side effects and complications of the postoperative period. The use of the TAP block in patients after performing allohernioplasty can be part of the strategy of multimodality and polyvalence of postoperative pain relief in abdominal surgery patients.
References
| [1] | Vilkotsky E.A., Minov A.F., Dzyadzko A.M. Anterior abdominal wall block as a regional component of multimodal analgesia in laparoscopic bariatric operations. Proceedings of the XVII Congress of the FAR September 28-30, 2018. St. Petersburg p.21 -22. |
| [2] | Makharin OA, Zavarzin P.Zh., Zhenilo VM, Skoblo MP, QL- or TAP block: what to prefer after cesarean section ?. Journal of the Bulletin of obstetric anesthesiology 2020 №2 (28) P.5-15. |
| [3] | Desmet M., Helsloot D., Vereecke E., Missant C., Van De Velde M. Pneumoperitoneum Does Not Influence Spread of Local Anesthetics in Midaxillary Approach Transversus Abdominis Plane Block: A Descriptive Cadaver Study. Regional Anesthesia and Pain Medicine. 2015; 40 (4): 349-354 58. |
| [4] | ElkassabanyN. Ahmed. M, Malkowicz S. B, Heitjan. D.F, Isserman J. A, Ochroch E A. et.al. Comparison between the analgesic efficacy of transversus abdominis plane (TAP) block and placebo in open retropubic radical prostatectomy: a prospective, randomized, double-blinded study. J ClinA-nesth. 2013 Sep; 25 (6): 459-65. |
| [5] | Farooq M, Carey M. A Case of Liver Trauma with a Blunt Regional Anesthesia Needle While Performing Transversus Abdominis Plane Block. Regional Anesthesia and Pain Medicine 2008; 33: 274-275. |
| [6] | Hebbard P, Fujiwara Y, Shibata Y, Royse C. Ultrasound-guided transversus abdominis plane (TAP) block. Anesthesia and Intensive Care 2007; 35: 616-617. |
| [7] | Hebbard P. Laffey J, McDonnell J Subcostal transversus abdominis plane block under Ultra-sound guidance. Anesthesia and Analgesia 2008; 106: 674-675. |
| [8] | Hebbard P. Subcostal transversusabdominis plane block under ultrasound guidance. Anaes-thesia and Analgesia 2008; 106: 674-675. |
| [9] | Johns N et al., 2014 K. Webster "Transverse abdominal blockage" magazine "Up-date in Anesthesia" No. 14, pp. 18-23, 2009. |
| [10] | McDonnell J, Curley G, Carney J, Benton A, Costello J, Maharaj C, Laffey J. The Analgesic Efficacy of Transversus Abdominis Plane Block After Cesarean Delivery: A Randomized Controlled Trial. Anesthesia and Analgesia 2008; 106: 186-191. |
| [11] | McDonnell J, O'Donnell, Brian M, Curley G, Heffernan A, Power C, Laffey J. The Analgesic Efficacy of Transversus Abdominis Plane Block After Abdominal Surgery: A Prospective Randomized Controlled Trial. Anesthesia and Analgesia 2007; 104: 193-197. |
| [12] | Niraj G., Searle A., Mathews M., Misra V., Baban M., Kiani S., Wong M. Analgesic efficacy of ultrasound-guided transversus plane block in patients undergoing open appendectomy. Br. J. Anaesth 2009; 103: 601-5. |
| [13] | Siddiqui MR, Sajid MS, Uncles DR, et al.: A meta-analysis on the clinical effectiveness of transversus abdominis plane block. J ClinAnesth. 2011; 23 (1): 7-14. McDonnell J, Laffey J. Transver-sus Abdominis Plane Block. Anesthesia and Analgesia 2007; 105: 883. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML