Samiev Asliddin Sayitovich1, Mavlyanova Zilola Farhadovna2
1Lecturer, Department of Neurology and Neurosurgery, Faculty of Postgraduate Education, Samarkand State Medical Institute, Candidate of Medical Sciences, Samarkand State Medical Institute, Uzbekistan
2Head of the Department of Medical Rehabilitation, Candidate of Medical Sciences, Associate Professor, Sports Medicine and Traditional Medicine, Samarkand State Medical Institute, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The presented article studies the effectiveness of nutritional support in the complex rehabilitation of severe forms of cerebral palsy in children of different ages. To date, there are no or very few data on the use of nutritional support in the process of rehabilitation of children with cerebral palsy, as well as on its influence on the course and prognosis of infantile cerebral palsy.
Keywords:
Children and cerebral palsy, GMFCS scale, Nutritional support
Cite this paper: Samiev Asliddin Sayitovich, Mavlyanova Zilola Farhadovna, Nutritive Support in Comprehensive Rehabilitation of Children with Cerebral Paralysis, American Journal of Medicine and Medical Sciences, Vol. 11 No. 4, 2021, pp. 334-339. doi: 10.5923/j.ajmms.20211104.16.
1. Introduction
According to foreign and domestic researchers a one second leading cause of child disability in the pathology of the nervous system is the e etsky cerebral palsy. Thus hours pilots at complicated eny cerebral palsy directly proportional to motor deficits, and n redstavlennost this group of diseases is significantly increased not only in preterm and very preterm infants [1,5,11,12], but also have a direct dependency on other factor s prenatal risk during the current pregnancy, turn the soup 's intrauterine development of the fetus, the clinical manifestations of preeclampsia, edema, proteinuria and hypertension, multiple pregnancy, bleeding in the 3rd trimester and the male sex of the fetus, fetal infections, infection or intoxication of the mother, the most common T ORCH infections and influenza infection [3,6]. The factors of intrauterine risk on the part of the mother also include a burdened obstetric and gynecological history [2,4].On reliably marker of asphyxia n When birth is to assess on a scale Apgar at 1st and 5th minute of life; the association of a low score - from 6 to 4 or less points - with an unfavorable outcome of perinatal encephalopathy has been repeatedly noted [7,8].In everyday life, the Global Motor Function Classification System (GMFCS) is used to assess the motor function of a child with cerebral palsy. Its use is mandatory for dynamic monitoring of a child during the rehabilitation period [9]. Since, due to eating disorders, severe forms of nutritional deficiency develop precisely in children with severe cerebral palsy (on the GMFCS scale at levels III - IY) [10], they need nutritional support. That is why a ktualnostyu of this study served as the interest in the use of enteral nutritional support, as a way to improve the effectiveness of rehabilitation in severe forms of children of cerebro of paralysis and.
2. Materials and Research Methods
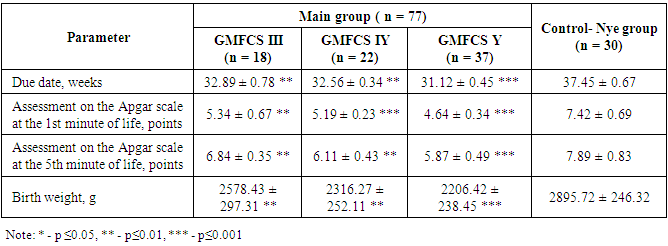
We examined 77 children with severe cerebral palsy at the age from 2 to 17 years. The control group consisted of 30 healthy children b ithout ities stvuyuschey neurological symptoms. All of the patients ranged in age groups under the age classification of the classification systems of large motor functions GMFCS (of Global Motor the Function the Classification the System) as follows: 2-4 years - 14 children (18.18%), 4-6 years - 16 children (20, 78%), 6-12 years old - 27 children (35.07%), over 12 years old - 20 children (25.97%). Figure 1 shows the age characteristics of patients with cerebral palsy and neurologically healthy children in the control group, indicating the predominance of children aged 6 to 12 in both groups: 35.07% in the main group and 36.67% in the control group.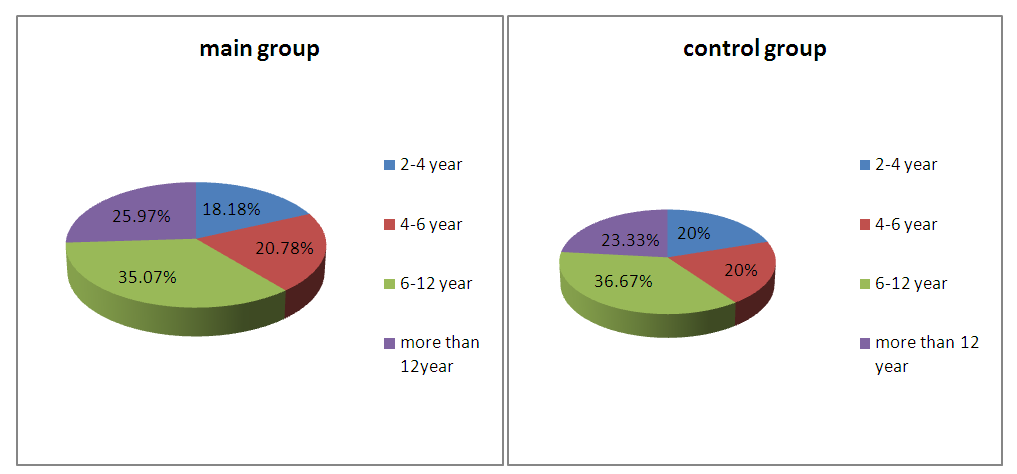 | Figure 1. Distribution of examined children by age |
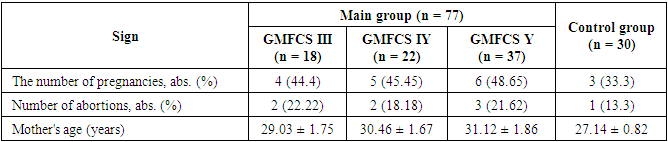
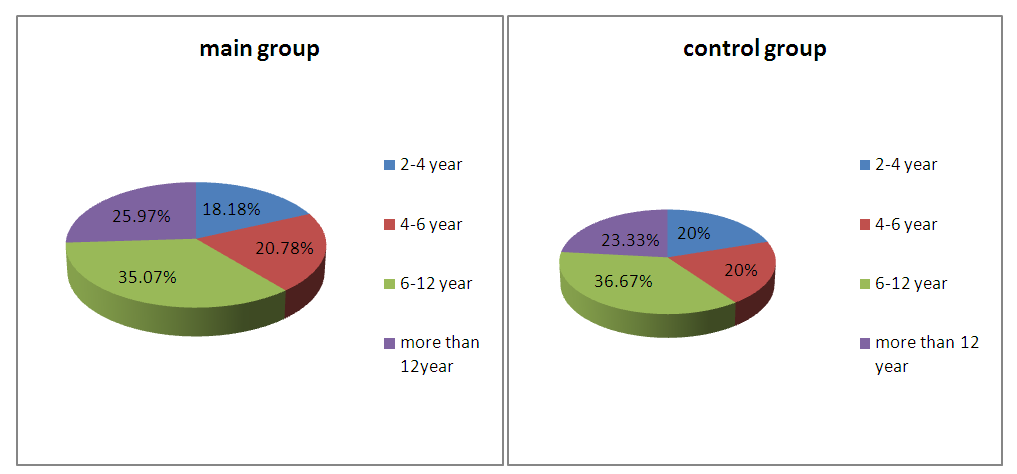
77 sick children with severe cerebral palsy - 40 boys (51.9%) and 37 girls (48.1%) were divided into 3 subgroups according to the severity of motor disorders and clinical manifestations on the GMFCS scale : GMFCS level III - 18 children (23.38%), GMFCS IY level - 22 children (28.57%), GMFCS Y level - 37 children (48.05%), with almost 2 times predominance of patients with the most severe course of cerebral palsy - Y level of GMFCS (Figure 2).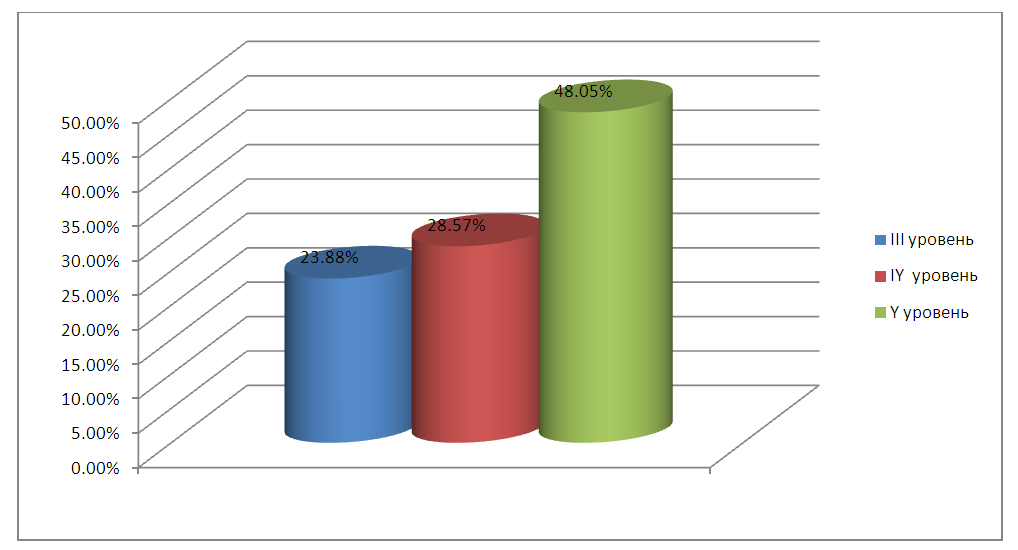 | Figure 2. Distribution of examined patients depending on motor deficit according to the GMFCS scale |
In the process of nutritional support, all patients were divided into 2 groups: the main group - 41 patients (53.25%, age - 11.12 ± 6.2 years), in whom a complex of rehabilitation measures was carried out against the background of correction of nutritional deficiency with enteral mixture, and comparison group - 36 children (46.75%, age - 12.13 ± 4.03 years) who received an identical set of rehabilitation measures without nutritional correction.All patients were performed the whole complex of clinical and neurological research methods, including a survey of children and their parents or guardians on the subject of complaints, including the features of eating disorders. If necessary, an analysis of exchange cards maternity and the history of th disease outpatient and inpatient; assessment of nutritional status; examination of related specialists (consultation with an ophthalmologist, pediatrician, orthopedist, logo ped, medical psychologist).
3. Research Results
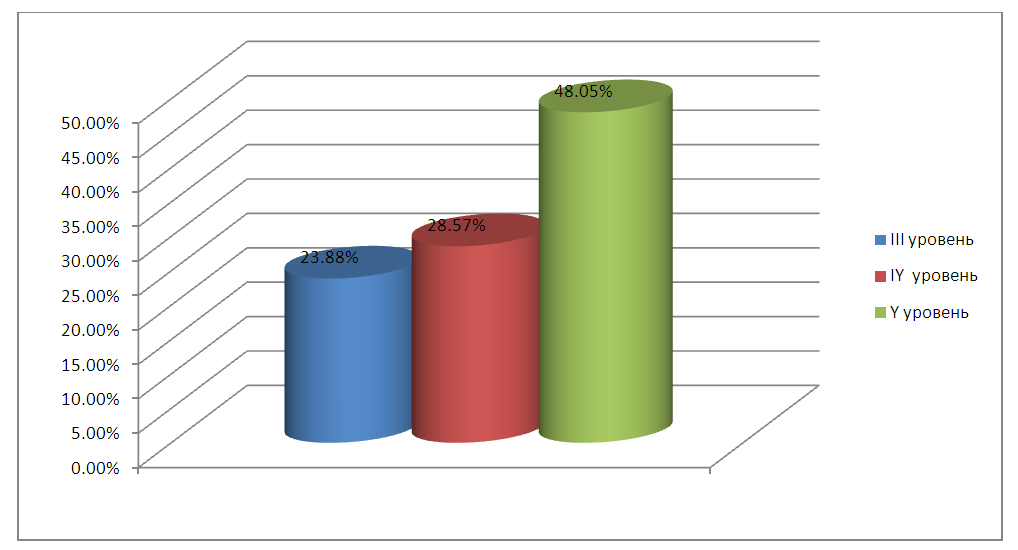
P on the results of neurological examination established f Orma cerebral palsy: spastic diplegia - 9.09%, hemiparetic form - 9.09%, hyperkinetic form - 16.88%, atoniko-astatic form - 12.99%, with a predominance of the most severe type movement disorders - double hemiplegia - 51.95% (Figure 3).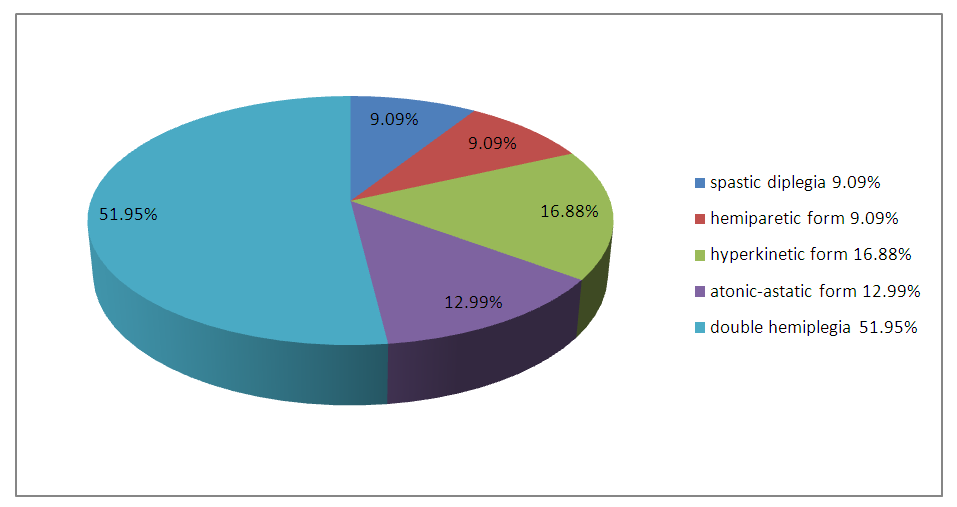 | Figure 3. Frequency of occurrence of various forms of cerebral palsy in the examined children |
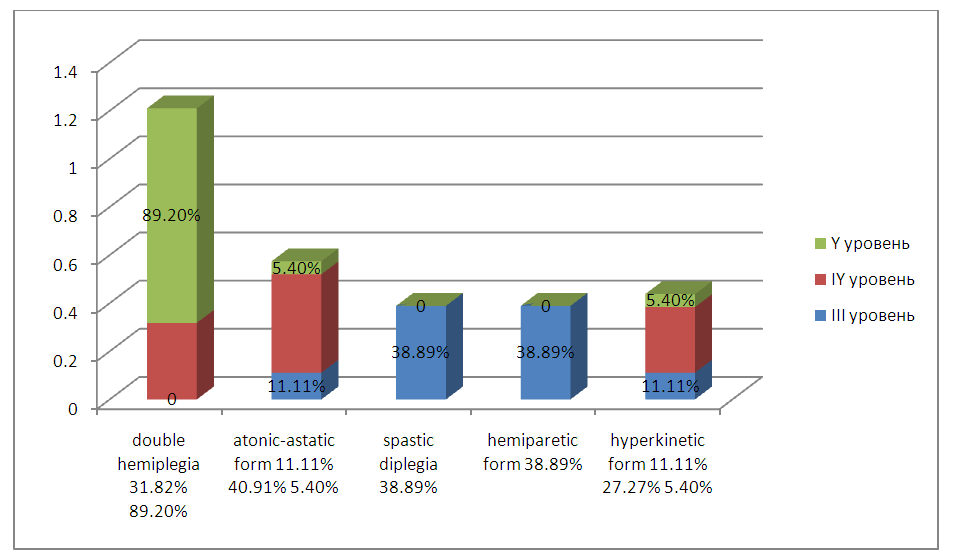
Depending on the form of infantile cerebral palsy, the patients had different levels of motor abilities (Figure 4). In more severe forms of cerebral palsy, such as double hemiplegia, the level V of the classification of motor abilities composed l to 89.2%, which corresponds ovalo pronounced disturbances of motor function. For children with V level it GMFCS was characterized by the strongest movement disorders, expressed very limited independent movement and self almost always impossible, including self meal. At the IY level, double hemiplegia (31.82%) and atonic-astatic form (40.91%) prevailed. In 38.89% of cases with level III motor disorders, spastic diplegia and hemiparetic form were diagnosed.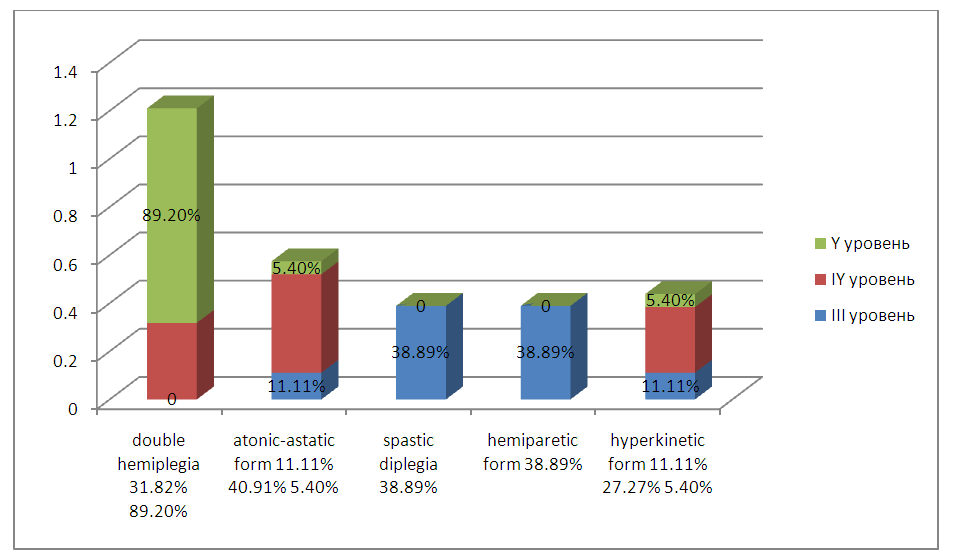 | Figure 4. Frequency of occurrence of various forms of cerebral palsy at different levels of motor function impairment on the GMFCS scale |
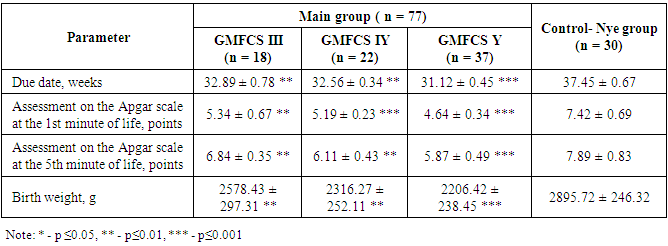
A nalysis terms of delivery and basic parameters of the newborn in the representation of the group at the mill sludge statistically significant th correlation th between the scores on the scale of Apgar at 1st and 5th minute of life of the newborn and the subsequent level of mo iterated deficit on a scale GMFCS, as well as the accuracy of th differences a indicators in the main and control groups ah (table 1).Table 1. About the main indicators of newborns of the main and control groups
 |
| |
|
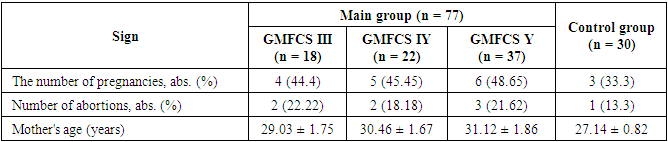
N roveden ny retrospective analysis revealed the dependence of the level of severity of motor disorders burdeness obstetric-gynecologic anamnesis mothers of children with cerebral palsy. The results of the influence of the age of mothers, the course of previous pregnancies, childbirth and the presence of abortions (spontaneous and medical) on the incidence of cerebral palsy and the severity of movement disorders are presented in Table 2.Table 2. Obstetric and gynecological history of the mothers of the examined children
 |
| |
|
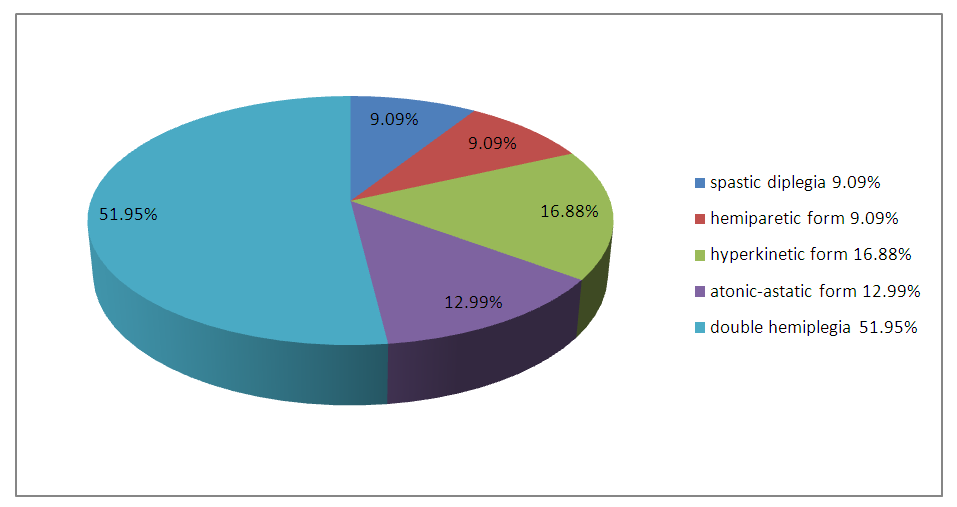
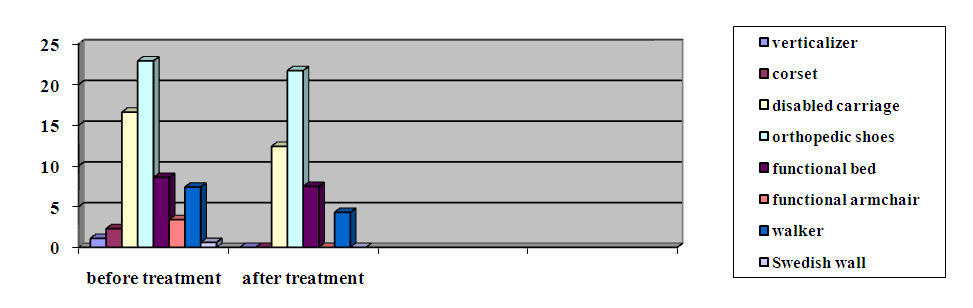
Characterization of the functional status of patients with infantile cerebral palsy as part of the assessment of the clinical and neurological status included a description of the child's daily activity according to the GMFCS classification scale for large motor functions. For the mobility of a child with cerebral palsy the most critical IY - th GMFCS level. 31.82% of patients with this level of movement disorders could not move even within their room; 22.73% of patients could leave the house using their hands. All children with the Y level of GMFCS were practically immobilized, and only 8.1% could move independently only in the form of crawling. At the same time, eating difficulties were more often experienced by children with more severe motor impairments. For example, children of the third level of classification GMFCS feeding problems arose whether in 16.67% of cases. On the most difficult - the V level - because of the limited rd is arbitrary th control I have over voluntary movements, etc. atsienty could not there to monitor the position of the head and body and resist the force of gravity; they need help from adults in taking care of themselves, moving around and feeding in 94.59% of cases. It should be noted that regardless of the form of cerebral palsy the Supervisory l by a high percentage of children with swallowing disorders, which potentially will build Valo prerequisites for the development of eating disorders.During dynamic examination 6 months after the start of a complex of rehabilitation measures with correction of nutritional status, the increase in height in children with cerebral palsy in the main group ranged from 1, 2 to 4, 9 cm (Δ height + 2.8 cm), while in children in the comparison group, the growth rate varied from 0.4 to 1.6 cm (Δ height + 0.67 cm). It should be noted that all indicators characterizing the dynamics of growth in patients with infantile cerebral palsy against the background of nutritional status correction were higher than in children in the comparison group.When gemipar e cal form of cerebral palsy in the study group as early as the beginning of treatment indicated a significant Restore Lenie Dvigatelno x function d of the lower limbs: decreased spasticity in the muscles, the children dragged lower leg longer walked, tried to jump. The vocabulary has also increased, the possibilities of social communication have expanded. Subsequently increased Xia amount of active x motion first in the hand, children often take toys more manipulated by them in the course of the games s. In the course of subsequent rehabilitation, intellectual capabilities improved: memory, attention, thinking, increased interest in learning and communication with peers. Lower results were noted in children in the comparison group. In such children, at the beginning of rehabilitation measures, it was possible to achieve only a slight decrease in spasticity, better fixation of the head, and understanding of the addressed speech. Gradually, the range of motion in the hands increased, the children reached for the toys, grabbed them. In the process of further rehabilitation, many children tried to sit, stand, walk with support, that is, restore gross motor skills. Patients in the study group after developed comprehensive rehabilitation performance in the category of Self Expand were 2.3 times, in the communication category (12 times) in the gaming activity (4.5-fold), orientation (by 3.8 times), movement (3.3 times).H Amet also a positive trend to reduce the need of sick children the main group in the special equipment and aids already in the early stages of rehabilitation. At the same time, the need for a disabled child suffering from infantile cerebral palsy for special equipment and aids before and after rehabilitation measures differed significantly in the observation groups (Figure 5).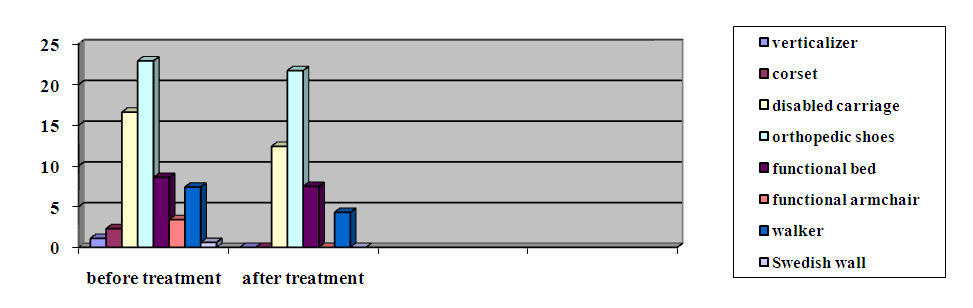 | Figure 5. The need for a disabled child in the main group for special equipment and technical means |
4. Conclusions
As a result of the study, it was found that the frequency of nutritional deficiency depends on the level of motor disorders on the GMFCS scale and the form of cerebral palsy. The classification system of major motor functions GMFCS is an easy-to-use method and can be used not only for the assessment of motor abilities in children with cerebral palsy, called on and serve as predictor of nutritional deficiency.Feeding difficulties for infants with cerebral palsy are directly related to their motor abilities, such as independent movement and self-care. That is why children with cerebral palsy are statistically more prone to very low physical development than children in the control group. In patients with infantile cerebral palsy, disharmony in physical development occurs with a very high frequency and is primarily caused by nutritional disorders. That is why the positive dynamics of growth indicators is a reliable parameter of the effectiveness of rehabilitation measures against the background of nutritional correction.Nutria and tive support in children with cerebral palsy is an important part of the rehabilitation program, with posobstvu I not only improve the anthropometric parameters in the dynamics of observation, but also a reduction of pathological reflexes, muscle spasticity. Enteral nutritional support is also used lagopriyatno affects the reduction and the needs of sick children in special equipment and aids already in the early stages of rehabilitation.
References
| [1] | Abdel- Hamid, HZ Cerebral Palsy [electronic resource] / HZ Abdel- Hamid, AS Zeldin, AT Bazzano [et al] // Medscape. - 1994 - 2018. - Access mode: https://emedicine.medscape.com/article/1179555-overview. |
| [2] | Alfirevic, Z. Amniocentesis and chorionic villus sampling for prenatal diagnosis [electronic resource] / Z. Alfirevic, K. Navaratnam, F. Mujezinovic // Cochrane Database Syst. Rev. - 2015. - V.9: CD003252. - Access mode: https://www.cochrane.org/CD003252/PREG_amniocentesis-and-placental-samplingpre-birth-diagnosis. |
| [3] | Arner, M. Hand function in cerebral palsy. Report of 367 children in a populationbased longitudinal health care program / M. Arner, AC Eliasson, S. Nicklasson [et al] // J. Hand Surg. Am. - 2008. - V. 33 (8). - P.1337 – 47. |
| [4] | Bartlett, D. Interrelationships of Functional Status and Health Conditions in Children With Cerebral Palsy: A Descriptive Study / D. Bartlett, E. Dyszuk, B. Galuppi, JW Gorter // Pediatr. Phys. Ther. - 2018. - V.30 (1). - P.10 - 16. |
| [5] | Benfer, KA The Eating and Drinking Ability Classification System in a populationbased sample of preschool children with cerebral palsy / KA Benfer, KA Weir, KL Bell [et al] // Dev. Med. Child Neurol. - 2017. - V.59 (6). - P.647 - 654 |
| [6] | Boychuck, Z. Age at referral for diagnosis and rehabilitation services for cerebral palsy: a scoping review [electronic resource] / Z. Boychuck, A. Bussières, J. Goldschleger, A. Majnemer // Dev. Med. Child Neurol. - 2018. - [Epub ahead of print]. - Access mode: https://onlinelibrary.wiley.com/doi/abs/10.1111/dmcn.14034. |
| [7] | Cobanoglu, M. The effect of hip reconstruction on gross motor function levels in children with cerebral palsy / M. Cobanoglu, E. Cullu, I. Omurlu // Acta Orthop. Traumatol. Turc. - 2018. - V.52 (1). - P.44 - 48. |
| [8] | Colver, A. Cerebral palsy / A. Colver, C. Fairhurst, PO Pharoah // Lancet. - 2014. - V. 383 (9924). - P.1240 - 9. |
| [9] | Compagnone, E. Functional classifications for cerebral palsy: correlations between the gross motor function classification system (GMFCS), the manual ability classification system (MACS) and the communication function classification system (CFCS) / E. Compagnone, J. Maniglio, S. Camposeo [et al] // Res. Dev. Disabil. - 2014. - V. 35 (11). - P.2651 - 7. |
| [10] | Gilles, F. Hypoxia-ischemia is not an antecedent of most preterm brain damage: the illusion of validity / F. Gilles, P. Gressens, O. Dammann, A. Leviton // Dev. Med. Child Neurol. - 2018. - V.60 (2). - P.120 - 125. |
| [11] | Farhadovna MZ, Sabrievna VA Dependence Of Protein-Energy Insufficiency On The Degree Of Motor Disorders In Infantile Cerebral Palsy // The American Journal of Medical Sciences and Pharmaceutical Research. - 2020 - T. 2. - No. 11. - p. 32-41. |
| [12] | Mavlyanova Z. et al. IMPROVING THE TACTICS OF TREATING CHILDREN WITH SEVERE CEREBRAL PALSY // European Journal of Molecular & Clinical Medicine. - 2020 - T. 7. - No. 2. - p. 2020. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML