Sh. N. Khudaybergenov, O. D. Eshonkhodjaev, B. B. Amanov, B. A. Saidkhanov
Republican Specialized Scientific and Practical, Medical Center of Surgery Named after Academician V. Vakhidov, Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Aim of the study was to analyze the results of membrane plasmapheresis using in combination with drug therapy in patients, depending on the severity of myasthenic syndrome. Introduction. Thymomas are the most common neoplasms of the mediastinum and account 10-20% among them. However, in general, they belong to rare human tumors, as they account for less than 1% of all oncological diseases. The age of the patients is generally varied from 40 to 60 years. The incidence of thymomas is traditionally considered relatively low - 0.15 per 100,000 populations. However, it has been established that the majority of patients suffering from thymus disease are in the active, working age of 40-55 years. Material and methods. The article presents the experience of treating 291 patients with thymomas and myasthenic syndrome. The article describes the technique of plasmapheresis. Depending on the severity of the disease, one course of membrane plasmapheresis consisted of 1 to 6 sessions. Plasma substitution was carried out after the sessions with amino acid solutions or protein preparations. All patients, both in the comparison group and in the main group, were performed drug therapy. But plasmapheresis, as an obligatory component of conservative treatment, was introduced only in the main group. Results and discussion. The inclusion of membrane plasmapheresis in the protocol of preoperative preparation of patients with thymomas and myasthenic syndrome as an extracorporeal detoxification was an effective method. Reliable statistics showed that the number of patients with severe myasthenia gravis in the main group had decreased. Conclusion. Complex therapy in combination with plasmapheresis allowed to significantly increase the number of patients with mild forms of myasthenia gravis, to reliably reduce the quantity of myasthenic crises in patients of the main group in the postoperative period.
Keywords:
Thymoma, Myasthenia gravis, Myasthenic syndrome, Plasmapheresis, Efferent therapy
Cite this paper: Sh. N. Khudaybergenov, O. D. Eshonkhodjaev, B. B. Amanov, B. A. Saidkhanov, Plasmaferesis in Complex Treatment of Thymomas with Myasthenic Syndrome, American Journal of Medicine and Medical Sciences, Vol. 11 No. 4, 2021, pp. 328-333. doi: 10.5923/j.ajmms.20211104.15.
1. Introduction
Thymomas are the most common neoplasms of the mediastinum and account 10-20% among them. However, in general, they belong to rare human tumors, as they account for less than 1% of all oncological diseases. The age of the patients is generally varied from 40 to 60 years. The incidence of thymomas is traditionally considered relatively low - 0.15 per 100,000 populations. However, it was found that the majority of patients suffering from thymus disease are in the active, able-bodied age of 40-55 years [1-3].An important feature of thymus disease is their combination with various, mainly autoimmune systemic syndromes (the so-called associated diseases or syndromes: neuromuscular, endocrine, hematological and diffuse connective tissue diseases). Generalized myasthenia gravis (from 30 to 50%) is the most common among the autoimmune syndromes that are typical for thymomas [4-6]. Thymomas, in turn, are found in approximately 17-20% of patients with myasthenia gravis [7-8].There have been more and more reports of the use of plasmapheresis in the treatment of myasthenia gravis in recent years. The improvement of the patients’ clinical condition as a result of using plasmapheresis is associated with the antibodies removal along with the plasma, including a decrease in the concentration of antibodies to acetylcholine receptors (AChR) and other plasma components that have pathological significance. A significant decrease in the concentration of antibodies to AChR has been confirmed by a number of researchers [3]. However, it was not possible to establish an exact correlation between the clinical effect of plasmapheresis and a decrease in the concentration of antibodies to AChR. The relatively recent beginning of the active use of plasmapheresis in the clinical treatment of myasthenia gravis has led to a lack of consensus among researchers on the indications and methods of its implementation.Aim of the research was to study the results of using plasmapheresis in combination with drug therapy in patients with thymomas with myasthenic syndrome.
2. Materials and Methods
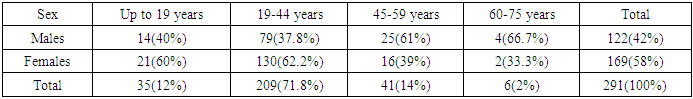
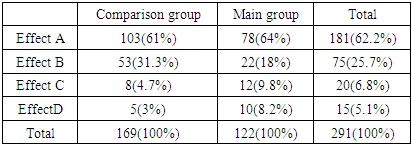
291 patients with thymomas and myasthenic syndrome who were undergoing in patient examination and treatment in the Department of Lung and Mediastinal Surgery of the Republican Specialized Scientific and Practical Medical Center of Surgery named after academician V. Vakhidov for the period from 1994 to 2019 were the basis for this research. The distribution of patients into two groups was carried out depending on the differentiated approach to the choice of diagnostics, treatment tactics and surgical intervention.Thus, the comparison group (CG) consisted of 169 patients who were hospitalized in the period from 1994 to 2009. A differentiated approach was not used in the choice of surgical tacticsin this period. For large tumor sizes, as well as for severe forms of myasthenic syndrome, surgical treatment was not performed. Patients were referred for further conservative treatment to a neuropathologist at their place of residence. Also, only longitudinal sternotomy was used as a surgical approach during this period.The main group (MG) included 122 patients who were on inpatient treatment in the period from 2010 to 2019. During this period, the approach to the diagnostics and treatment of patients with thymomas and myasthenic syndrome, regardless of the tumorsizeand the severity of myasthenia gravis, totally changed. In the main group, a differentiated approach was used to determine the treatment tactics depending on the severity of myasthenia gravis, the size of the tumor, the choice of the surgical approach and the nature of the intervention.The age of the patients ranged from 19 to 75 years. There were no patients older than 75 years. Females predominated among patients with thymomas - 169 (58% of the total number of patients).There were 122 (42%) male patients. Young and middle-aged persons accounted for 86% - 250 patients, which undoubtedly indicates the social significance of the studied problem. The distribution of patients by sex and age is shown in Table 1.Table 1. The distribution of patients by sex and age
 |
| |
|
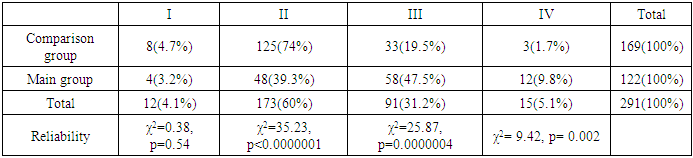
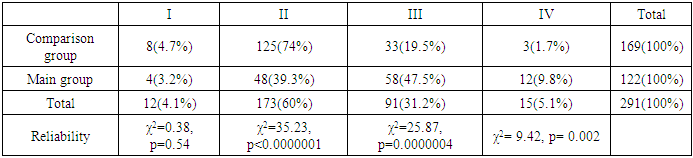
When analyzing the anamnestic data, we found the following: 27 (9.3%) patients associated the onset of the disease with the influenza, 8 (2.7%) patients noted the connection with the nervous stress and 256 (88%) patients did not note the connection with past illnesses and any other reasons. We used the classification of K. Osserman and G. Jenkins, adopted as international in 1959 and modernized in 1971 when assessing the severity of myasthenic syndrome. The distribution of patients according to the severity of myasthenic syndrome is presented in Table 2.Table 2. Distribution of patients according to the severity of myasthenic syndrome
 |
| |
|
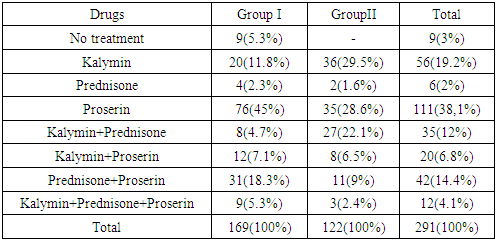
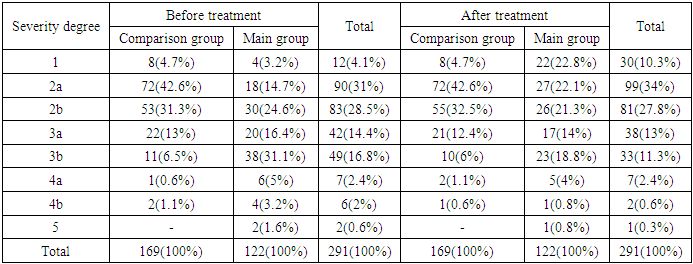
There was a significant (χ2 = 35.23, p <0.0000001) greater number of patients with grade II severity of myasthenic syndrome in the comparison group - 125 (74%). There were significantly (χ2 = 25.87, p = 0.0000004) more patients with grade III - 58 (47.5%) and with grade IV - 12 (9.8%) - χ2 = 9.42, p = 0.002in the main group. The prevalence of patients with grades III and IV in group II was due to the fact that in the period from 1994 to 2009, patients were refused surgical treatment and were referred for conservative treatment to endocrinologists and neuropathologists. From 2010 to the present, the approach to the treatment of patients with thymomas with severe forms of myasthenic syndrome has been totally changed. According to the duration of the disease, we noted that the majority of patients sought medical help in the first two years from the onset of the disease.The set of medications is quite wide, but the main are anticholinesterase drugs (kalymin, proserin) in combination with potassium drugs (calcium chloride, orotatepotassium), the use of corticosteroid drugs (prednisone, methylprednisone). This is necessary in order to the temporary deterioration of the patient's condition in the postoperative period does not lead to inhibition of vital body functions and to the development of a crisis. The applied treatment regimens with anticholinesterase drugs and glucocorticosteroids (GCS) are presented in Table 3.Table 3. Distribution of patients by taking anticholinesterase drugs and glucocor-ticosteroids in groups before surgery
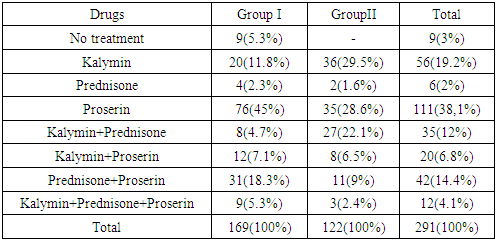 |
| |
|
We used anticholinesterase drugs and glucocorticosteroids both in monotherapy and in combination to achieve the most positive effect. As it was mentioned above, the approach to treatment in the comparison group was different from the main group (MG).Thus, 9 (3%) patients in the CG received no drug treatment.The largest number of patients - 111 (38.1%) received proserin in monotherapy: 76 (45%) from CG and 35 (28.6%) in MG. Kalymin in monotherapy was used in 56 (18.2%) cases: in 20 (11.8%) in the CG and in 36 (29.5%) from the MG. Prednisone monotherapy was used in 6 (2%) patients: 4 (2.3%) in CG and 2 (1.6%) inMG.42 (14.4%) patients received the combination of proserin and prednisone and the combination of kalymin and prednisone was used in 35 (12%) patients. The combination of kalymin and proserin was used in 20 (6.8%) cases: 12 (7.1%) in CG and 8 (6.5%) in MG. In 12 (4.1%) patients, a scheme including prednisolone, kalymin and proserin was used: in 9 (5.3%) from CG and in 3 (2.4%) in MG. Plasmapheresis was usedat an exacerbation of the disease and at a myasthenic crisis, when myasthenic disorders are not stopped by anticholinesterase drugs and hormones. Plasmapheresis has been also used as a component for the comprehensive preparation of patients for thymectomy. This procedure promotes the elimination of the corresponding antibodies from the blood, including those that are a key factor in the pathogenesis of myasthenia gravis.We used the "Hemophenix" device (Russia) (Fig. 1). During plasmapheresis blood separation occurs not in a centrifuge (by gravitational method), but in a “Rosa” nanofilter which excludes traumatization of blood corpuscles.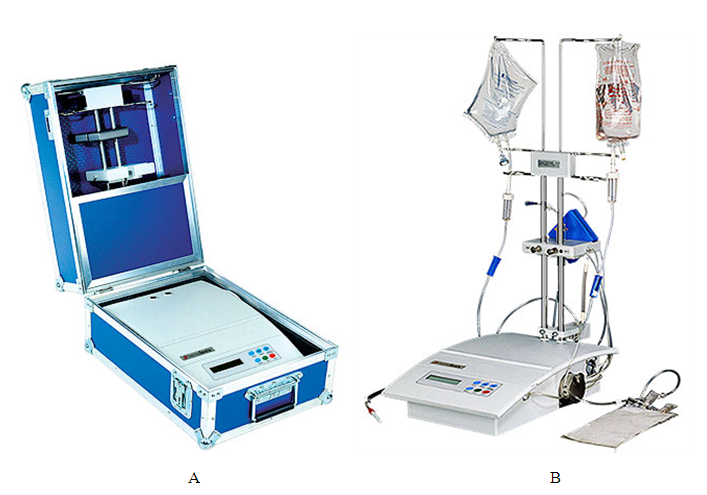 | Figure 1. "Hemophenix" device: a). folded view; b). working view |
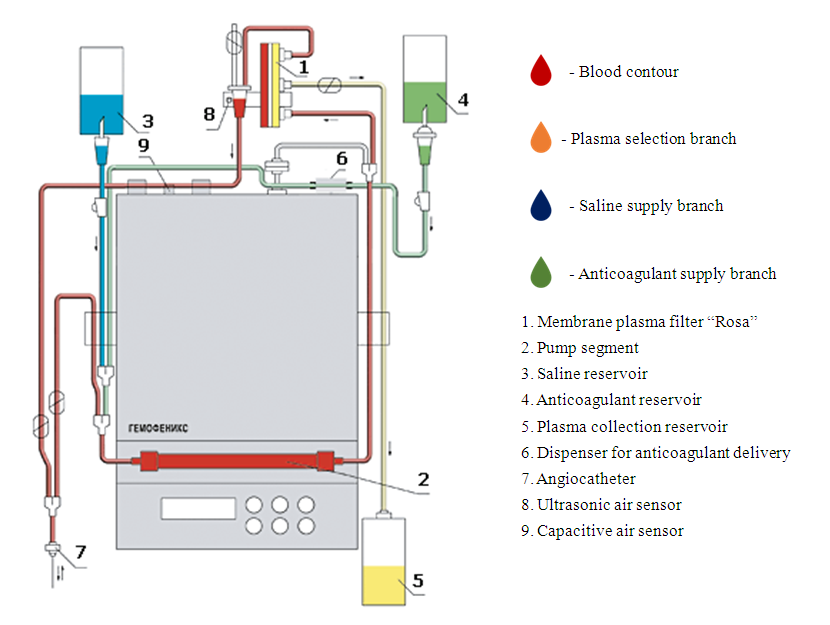
"Hemophenix" operates in an adaptive mode: it takes from as much blood the patient as he is able to "give" per cycle which eliminates unpleasant sensations. Blood collection and return occurs during catheterization of one peripheral vein. The process is automated. It is absolutely safe. While the procedure is in progress, the device provides all information about the process in the system and the patient's condition.The continuous process of membrane plasmapheresis on the “Hemofenix” apparatus is carried out according to a single-needle scheme in a sterile extracorporeal single-use circuit (Fig. 2).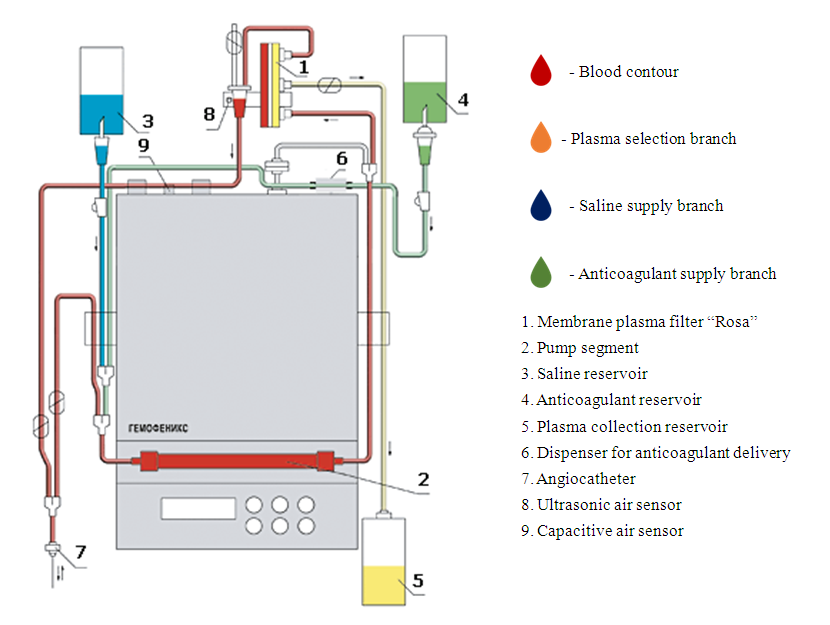 | Figure 2. "Hemophenix" device with the "Rosa" plasma filter:scheme of operation |
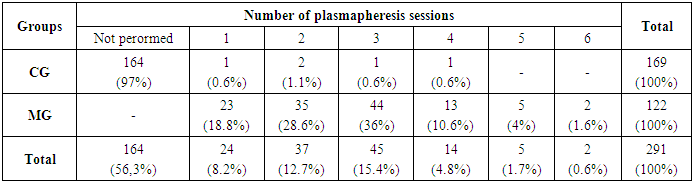
During the procedure the shaped elements are returned to the patient's bloodstream, the plasma is collected in a special receiver and plasma replacement is performed. Donor plasma obtained on the "Hemopheniks" devise and "Rosa" plasmofilter meets the regulatory requirements of the Blood Service. The course of plasmapheresis usually consisted of 1-6 sessions (depending on the severity of the disease, in particular for patients on artificial lung ventilation (ALV) - 4-6 sessions) with an interval of 1-2 days. The volume of plasma removed in one operation is 35 - 45 ml of plasma / kg of the patient's body weight. Replenishment is carried out with isotonic sodium chloride solution, solutions of Rheosorbilact and 5% albumin in a 1: 1: 1 ratio. Plasmapheresis is performed in isovolemic mode. Heparin was used as an anticoagulant. The distribution of patients depending on the number of plasmapheresis sessionsin groups performed is presented in Table 4.Table 4. Distribution of patients by the number of performed plasmapheresis sessions in groups before surgery
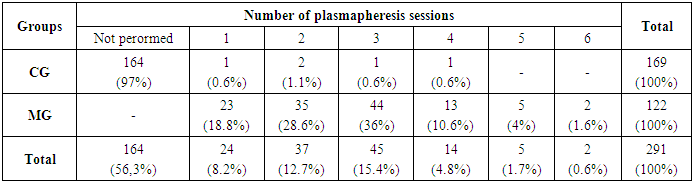 |
| |
|
In most cases, 1-4 sessions of plasmapheresis were carried out with a volume of substituted plasma of about two liters. Plasmapheresis was performed in 127 (43.6%) from 291 patients. In 164 (56.3%) cases efferent therapy was not performed. All 164 patients who were not performed plasmapheresis in the preoperative period were CG. Efferent therapy was carried out in only 5(3%) patients of CG as a preoperative preparation. Plasmapheresis was performed for all patients in MG, taking into account changes in treatment tactics. Patients of MG significantly (χ2 = 271.3, p <0.05) underwent more plasmapheresis sessions before surgery.
3. Results
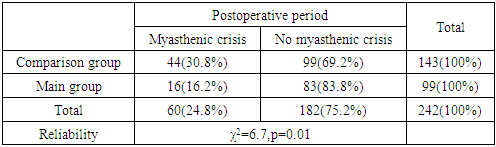
The analysis of drug treatment efficiency was carried out in accordance with the international classification of the clinical effect:• complete drug-free remission - no symptoms of the disease> 1 year without specific therapy (effect A);• drug remission - the absence of symptoms of the disease or minimal manifestations against the background of constant use of anticholinesterase drugs or immune-suppressive drugs (effect B);• good compensation of the condition - a significant regression of symptoms and the absence of disease progression against the background of constant anticholinesterase and / or immune-suppressive therapy (effect C);• no effect of therapy: progression of the disease, exacerbation with a frequency of ≥1 times a year, the presence of persistent myasthenic manifestations impairing the efficiency and self-care of patients (effect D).The results of the drug therapy carried out in the groups are presented in Table 5.Table 5. The efficiency of drug therapy in groups
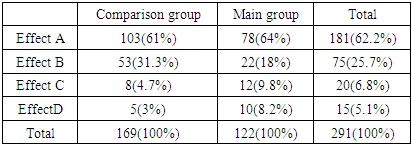 |
| |
|
As it can be seen from the table, effect A was achieved in 181(62.2%) patients: 103 (61%) in the comparison group and 78 (64%) in the main group. Effect B was achieved in 75 (25.7%) patients: in 53 (31.3%) cases of the comparison group and in 22 (18%) patients of the main group. Effect C in the comparison group was 8 (4.7%) and in the main group itmadeup10 (9.8%). Effect D in the main group was 8.2%, while in the comparison group this indicator was 3%. The deterioration in the effectiveness of drug therapy in the main group in terms of effects C and D was due to the fact that there were more patients with severe forms of myasthenic syndrome in the main group - 70 (57%). In the comparison group there were 36(21%) patients with severe forms of myasthenic syndrome. After drug therapy and plasmapheresis, we repeated the analysis of myasthenic syndrome severity before and after treatment. At the same time, an increase in the number of patients with 1 and 2 degrees of severity and a decrease in the number of patients from 3a to 5 degrees of myasthenic syndrome severity were found (Tab. 6).Table 6. Distribution of patients by severity degree before and after treatment
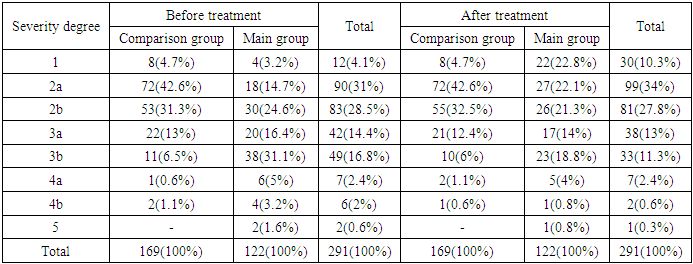 |
| |
|
4. Discussions
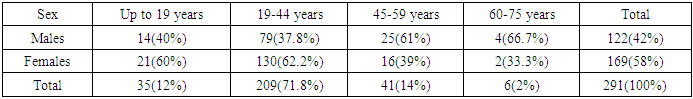
Statistical data was carried out according to the following criteria:1. The difference between the main and compared groups before plasmapheresis - χ2 = 55.17, df = 7, p <0.0000001 has a high significant difference.2. The difference between the main and compared groups after plasmapheresis χ2 = 38.61, df = 7, p = 0.000002315 has a high significant difference.3. The difference in the main group before and after plasmapheresis - χ2 = 20.7, df = 7, p = 0.004235, the difference is significant.Thus, after the therapeutic measures in the main group, there was a significant decrease in the severity of myasthenia gravis in compare with the comparison group. The effect of plasmapheresis, according to many authors, is associated with a rapid decrease in the concentration of antibodies to cholinergic receptors, however, an improvement also occurs at seronegative myasthenia gravis. In general, after treatment with plasmapheresis, an improvement in motor functions was observed while taking anticholinesterase drugs in almost all patients. This is especially clearly seen in the results of the main group, where a combination of drug and efferent therapy was used.From 291 patients included in this study, 242 (83.1%) were performed surgical treatment and 49 (16.8%) patients were discharged without surgery. In the postoperative period, in addition to infusion, antibacterial, analgesic and standard anticoagulant therapy, patients were obliged to undergo anticholinesterase therapy, regardless of the presence of myasthenia gravis. The dosage and frequency of taking were selected individually. Glucocorticosteroids in the postoperative period were used only in cases when symptoms of myasthenia gravis were manifested and progression of symptoms of myasthenia gravis was noted in dynamics.Plasmapheresis as an obligatory component of therapy was used in all patients of the main group. In the comparison group plasmapheresis was used only in 16 patients, which made up11.1%, and plasmapheresis was not performed in 127 (88.8%) patients. In the comparison group, 1 session of plasmapheresis was performed in 3 (2%) cases, 2 sessions - in 8 (5.6%) patients, 3 sessions - in 3 (2%) cases, and 5 sessions - in 2 (1.4%) patients. In the main group, 1 session was performed in 23 (23.2%) patients, 2 sessions - in 31 (31.3%) cases, 3 sessions - in 41 (41.4%) patients and 5 sessions were conducted in 4 (4%) cases.In the postoperative period myasthenic crisis (MC) was observed in 60 patients and it made up 24.8%: in the comparison group MC was observed in 44 (30.8%) patients and in 16 (16.2%) cases of the main one. The incidence of MC in the compared groups is presented in Table 7.Table 7. Distribution of patients by the presence of myasthenic crisis in groups in the postoperative period
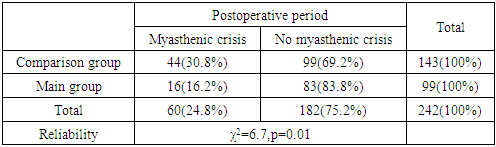 |
| |
|
In the postoperative period, the myasthenic crisis in patients of the main group was significantly (χ2 = 6.7, p = 0.01) reduced in compare with the control group. In the comparison group, the number of MCs was 30.8%, which is almost two times higher than in the main group, where the same indicator was 16.2%. The number of patients in whom the postoperative period proceeded without MC in the main group was 83 (83.8%) and in the comparison group this indicator was 99 (69.2%).As the results of the preoperative preparation of patients with myasthenic syndrome have clearly shown, the combination of drug therapy with the obligatory performance of plasmapheresis is considered an obligatory component of the complex treatment of myasthenia gravis, both as a preoperative preparation and in the postoperative period.
5. Conclusions
Plasmapheresis as a preoperative preparation is an effective method complementing drug therapy, which allowed to reliably (p <0.05) reduce the number of patients with severe myasthenia gravis in the study group from 57% to 38%. Conducting drug therapy in combination with plasmapheresis allowed to increase significantly (p <0.05) the number of patients with mild forms of myasthenia gravis in the main group from 42% to 63%; in the postoperative period it was a significant (χ2 = 6.7, p = 0.01) reduce of the number of myasthenic crises development from 30.8% in the comparison group to 16.2% in the main group. In the postoperative period, the number of MCs in the comparison group was 30.8%, which was almost two times higher than in the main group, where the same indicator was 16.2%.The number of patients in whom the postoperative period proceeded without MC in the main group was 83 (83.8%), and in the comparison group this indicator made up 99 (69.2%) cases.
References
| [1] | Kharchenko V.D., Chkhikvadze P.E., Kolesnikov S.V., Eoncharov, O.A. Yadikov // Bulletin of the Russian Scientific Center for Roentgenoradiology of the Ministry of Health of Russia. - 2011. - V. - 2. - No. 11. - P. 14. |
| [2] | Gajdos P, Chevret S, Toyka K., Plazma exchange for generalized myasthenia gravis. Cochrane Database of Systematyc Reviews 2011, Issue 4. |
| [3] | Saperstein D.S., Barohn R.J.. Management of myasthenia gravis. Semin Neurol 2004; 24: 41. |
| [4] | Bayramalibeyli I.E., Gadzhiev D.B., Ragimov A.A. The use of plasma pheresis in patients with thalassemia // In the collection: "Actual problems of extracorporeal therapy", mater. of conferences. - M., 2007. - P. 52-54. |
| [5] | Lobzin S.V. Myasthenia gravis, diagnosis and treatment / Lobzin S.V. - SPb.: Spetslit 2015 .-P. 160. |
| [6] | Baybekov I.M., A.I. Ibragimov, S.M. Rizaeva, A.I. Baybekov Application of laser therapy for reduction of changes in erythrocytes and cells of body in their pathology. Photodiagnosis and photodynamic therapy. Abstracts of Laser Helsinki 2010 15th International congress of EMLA, P 13. |
| [7] | Kolesnikov P.G. Diagnostics and treatment of thymoma: author. dis. ... Cand. med. sciences / P.G. Kolesnikov. - Moscow, 2011 – P. 22. |
| [8] | Voinov V.A. Efferent therapy. Membrane plasmapheresis. M. Trepkor Technology - M 2009. - P. 38. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML