-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(4): 301-307
doi:10.5923/j.ajmms.20211104.10
Received: Feb. 8, 2021; Accepted: Mar. 24, 2021; Published: Apr. 2, 2021

Initial Results of Implantation of Toric Phakic Intraocular Lens to Patients with High Myopia and Myopic Astigmatism: First Clinical Experience in Uzbekistan
Kamilov Khalidjan Makhamadjanovich1, Dadamukhamedova Shahida Mubashirovna2, Zaynutdinov Nozim Nadirkhodjayevich3
1Professor and Head of Ophthalmology Department, Tashkent Institute of Postgraduate Medical Education
2Chief Scientific Staff, Republican Specialized Center of Eye Microsurgery, Zaynutdinov Nozim Nadirkhodjayevich
3Independent Scientific Researcher, NAZAR Eye Center, Tashkent, Uzbekistan
Correspondence to: Kamilov Khalidjan Makhamadjanovich, Professor and Head of Ophthalmology Department, Tashkent Institute of Postgraduate Medical Education.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

We evaluate early clinical results of implantation of posterior chamber pIOL (phakic intraocular lens) for correction of patients with high myopia and myopic astigmatism during 6 months post-op period. The study is composed of first clinical experience to correct high refractive abnormalities with implantation of toric phakic IOLs (EVO + Visian ICL, implantable collamer lens) to patients in Uzbekistan.
Keywords: Refractive errors, High myopia, Astigmatism, Toric ICL, Visual acuity, Vault, Intraocular pressure
Cite this paper: Kamilov Khalidjan Makhamadjanovich, Dadamukhamedova Shahida Mubashirovna, Zaynutdinov Nozim Nadirkhodjayevich, Initial Results of Implantation of Toric Phakic Intraocular Lens to Patients with High Myopia and Myopic Astigmatism: First Clinical Experience in Uzbekistan, American Journal of Medicine and Medical Sciences, Vol. 11 No. 4, 2021, pp. 301-307. doi: 10.5923/j.ajmms.20211104.10.
1. Introduction
- At present, refractive errors are the leading pathology of the eye among population at a competent age. According to a number of epidemiological studies, a frequency of refractive error cases varies from 23 to 36% and even up to 40% [1].It is important to emphasize that the progression of refractive abnormalities can lead to serious irreversible changes in the eye and significant loss of vision. In ophthalmology, eyeglasses, contact lenses and surgical methods such as radial keratotomy, photo refraction, excimer laser surgery of the cornea, clear lens extraction, etc. are mainly used to correct the refractive anomalies. A number of studies indicate that high myopia and myopic astigmatism are the fourth to seventh disease accounting for blindness [2,3].The surgical correction of refractive errors such as high myopia and myopic astigmatism includes keratorefractive surgery, refractive lens extraction and phakic intraocular lens (pIOL) implantation. Phakic intraocular lenses are classified as anterior chamber (AC pIOL) and posterior chamber (PC pIOL). Anterior chamber pIOls are further subdivided based on the method of fixation to the ocular structures, which are angle fixated or iris fixated. They have commonly been used to treat high myopia because they can correct higher refractive errors rather than corneal refractive procedures [4,5].Initially, implantable lens consisting of a biocompatible collagen copolymer was developed by STAAR Surgical, (Monrovia CA, USA) in 1993 as a sulcus-placed posterior chamber pIOL and was called ICL. This lens can correct high refractive errors. ICL implantation has several advantages, including faster recovery, more stable refraction, and better visual quality, reversibility of the surgical procedure and exchangeability of the pIOL. However, the first models of ICL had more complications, which were revealed after implantation. Lens development and modification continues by manufacturer under supervising major scientists [6].The last modifications of toric (EVO + Visian ICL) VTICM5 model for correction of spherical and toric refraction errors were designed and manufactured in 2016. This lens has advanced optic size from 4.9 to 6.1 mm, which allows decreasing night light complaints such as halos and glare, on patients who underwent ICL implantation. These lenses have been already registered and certified to use in medical practice by The State Drugs and Equipment, Quality Control and Registration Committee of Uzbekistan.In this study, we aimed to evaluate initial clinical results during 6 months post-op period, after implantation of toric ICL to patients with high myopia and myopic astigmatism firstly in Uzbekistan. Such kind of studies and investigations had never been in this area till today.
2. Materials and Methods
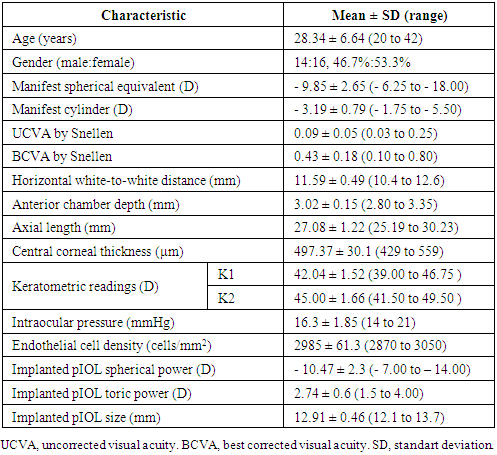
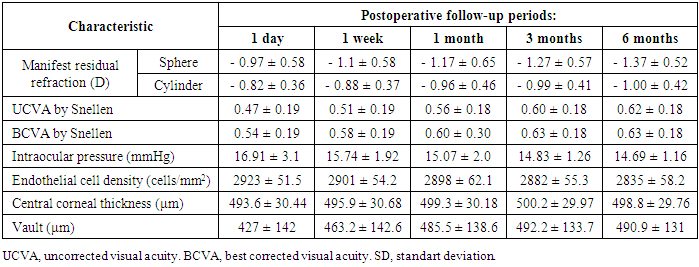
- This study comprised 54 eyes of 30 patients with high myopia and myopic astigmatism who underwent implantation of toric ICL (VTICM5 model) from May 2018 to December 2020 at NAZAR Eye Center, Tashkent, Uzbekistan. Those patients in whom LASIK surgery was contraindicated because of thin cornea and range of myopia was higher than - 6.0 diopters (D) and myopic astigmatism more than – 2.0 diopters. All patients had stable refractions within ± 0.75 D for 1 year before surgery. Each patient had undergone specialized ophthalmic examination such as bio ophthalmoscopy with dilated pupil by using 90 D aspheric lens (Volk Inc. USA), A & B ultrasound scanning of eye globe, non-contact tonopachymetry (Topcon, Japan), autorefkeratometry (Topcon, Japan), keratotopography (ORBSCAN III, ZYWAVE3, Germany), anterior and posterior segment OCT (HD - Cirrus 4000, Zeiss, Germany). IOL power calculation performed based on cycloplegic refraction, keratometry, axial length, anterior chamber depth (ACD) and lens thickness. By depending on keratopachymetric and ACD results we gave attention to anterior chamber depth from endothelium to the anterior surface of clear natural lens. This measure could not be less than 2.80 mm. Patients with peripheral retinal tears and lesions were treated by green laser coagulator (Novus spectra, Lumenis, USA). Exclusion criteria included lens opacities, peripheral retinal detachments, history of uviets, glaucoma, shallow anterior chamber, corneal pathology etc. Informed and written consents were obtained in each case. In all cases intraocular pressure measurements and gonioscopy had been done to ensure wide open angles, best corrected visual acuity (BCVA) and uncorrected visual acuity (UCVA) were recorded preoperatively and postoperatively. The White-to-White (WTW) diameter was measured using a digital biometric ruler-digital calipers. Endothelial cell count (ECC) was measured by using Tomey EM – 3000 specular microscope (Tomey Corporation, Japan). The ICL power was calculated by using the STAAR Surgical OCOS system (Online calculation and order system) https://evo-ocos.staarag.ch/Live/. Each eye had been examined by using anterior segment optic coherent tomography (OCT HD - Cirrus 4000, Zeiss, Germany) to determine (the vault) distance between ICL and anterior surface of clear natural lens in postoperative period at 1 day, 1 week and 1,3, 6 months.Surgical techniqueOn the day of surgery, patients were administered dilating and cycloplegic agents. Pupillary dilation was achieved using combination of Sol. Mydoptic (phenylephrine) 2.5% and tropicamide 1% eye drops, administered three times at 15 minutes interval, 1 hour prior to surgery. All surgeries performed under topical and subtennon anesthesia by a single high experienced surgeon using a standardized technique. Two clear corneal 1 mm paracentesis were made, and injected into AC hydroxypropylmethyl cellulose 1% - viscoelastic device. VTICM5 model of toric ICL was implanted through a 2.8 mm temporal clear corneal incision by using injector and cartridge system from STAAR Surgical. The ICL was placed and positioned into the posterior chamber by using Vukich ICL manipulator. The viscoelastic device was completely washed out of the anterior chamber with balanced salt solution, and myotic agent was instilled. All surgeries were happy ended and no intraoperative complication was observed. After surgery, combined agent (antibiotic + steroid) Sol. Tobradex 5ml 4 times a day and Sol. Timolol 0.5% - 5ml eye drops twice a day were administered topically during 2 weeks, then the dose of medications being reduced gradually.
3. Results
- A total of 54 eyes of 30 patients (24 bilateral and 6 unilateral toric ICL implanted patients) were recruited in this study. All patients had undergone Toric ICL (VTICM5 model) implantation in medical eye center by one surgeon. Preoperative demographic data are listed in Table 1. All eyes had successful surgery and there were no intraoperative complications encountered. The mean follow – up period was 6.5 ± 1.2 months.
|
|
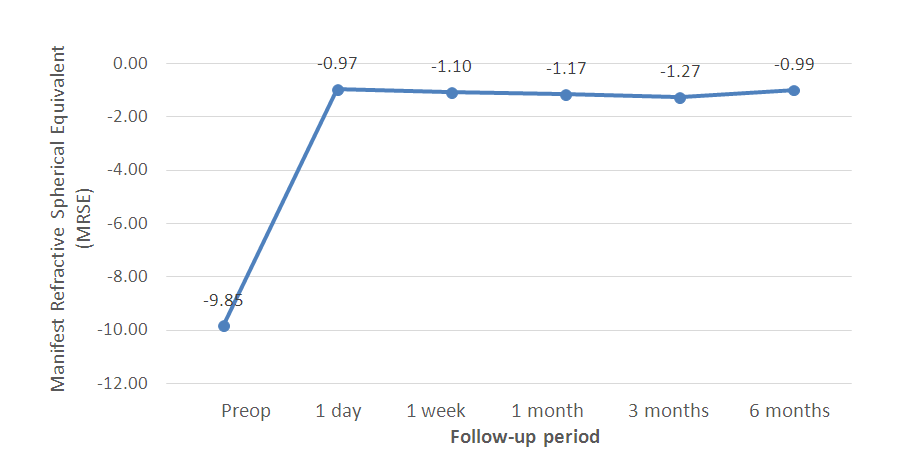 | Figure 1. Changes in mean spherical equivalent during 6 months postop period |
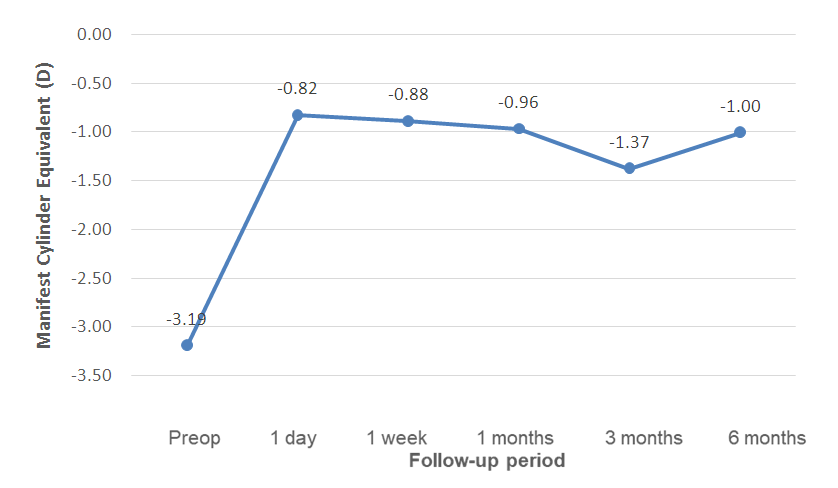 | Figure 2. Changes in mean cylinder equivalent during 6 months postop period |
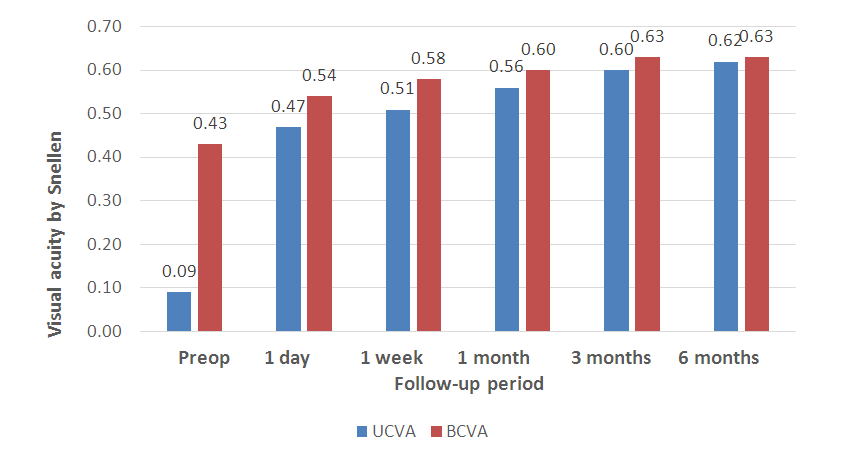 | Figure 3. Changes in UCVA and BCVA during 6 months postop period |
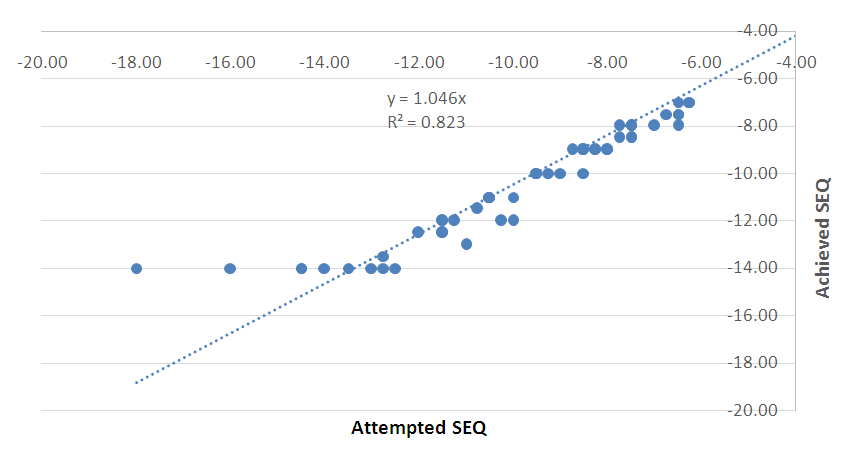 | Figure 4. Spherical equivalent refraction attempted vs achieved |
4. Discussion
- In the present study, our results showed that, in all measures of safety, efficacy, predictability and stability we gained satisfied outcomes after implantation of VTICM5 toric ICL model to patients with high myopia and myopic astigmatism during 6 months follow-up period. Concerning to the safety and efficacy of the procedure, toric ICL implantation was safe and efficacy for the correction of high myopia and myopic astigmatism with finding results that were matched in previous studies. With regard to predictability and stability, this procedure through a 2.8 mm temporal clear corneal incision, regardless of the amount of myopic correction, has negligible effect on refractive outcome, and that this surgical technique is less subject to the wound healing responses of the cornea [7]. Concerning to complications of the surgical technique, we found no significant rise of IOP during 6 months of post-op follow-up period. As mentioned above only in 5 cases we found increasing of IOP at 1 day and 1 week post op follow-up period and we reached to safe IOP values by using hypotensive eye drops. In any case, we did not find pigment dispersion symptoms in anterior segment of the eye during 6 months follow-up period. One of the first study of ICL model with central flow technology (V4c model with central hole) was performed by Shimizu et al. [8] (2012) in 20 myopic eyes (mean SE – 7.36 ± 2.13 D) reported 95% and 100% of eyes being within ± 0.50D and ± 1.00 D, respectively, of the target correction. Change in manifest refraction from 1 week to 6 months was 0.06 ± 0.28 D. Kamiya et al. [9] (2017) reported high level of results as 100% of eye being within ± 0.50D and ± 1.00 D, respectively, of the target correction with SE – 0.08 ± 0.17 D.Chen et al. [10] (2020) evaluated 22 eyes of 22 patients with high myopia and myopic astigmatism during 6 months. The mean SE was – 9.43 ± 5.01 D and the mean cylinder was – 3.75 ± 1.50 D. The mean age of patients were 26.5 ± 5.8 and the mean ACD was 3.42 ± 0.31 mm. In this study were implanted Toric ICL with the mean SE power - 12.4 ± 0.8 D and the mean cylinder 4.50 ± 1.00 D. Cao et al. [11] (2016) also followed – up 41 patients with 78 eyes after ICL implantation during 6 months postop period. In his study, the mean age of patients were 29.1 ± 8.3 and the mean SE was -12.55 ± 2.98 D. The mean WTW measures were 11.4 ± 2.98 mm. Pjano et al. [12] (2017) evaluated 28 myopic eyes (mean SE – 9.52 ± 3.69) of 16 patients and gained favorable post-op visual results UCVA (0.76 ± 0.16 by Snellen) and corrected visual acuity was (0.79 ± 0.14 by Snellen) within 1 year follow – up period after pIOL (ICL) implantation.Despite these good results, there are still concerns about whether the presence of an artificial hole in the center of the optic will deteriorate the optical quality of VTICM5 model. For example halos and glare decreasing the patient`s visual performance. However, previous studies concluded that the hole in ICL provided excellent optical quality that was essentially equivalent to that of nonhole conventional ICL. An animal model study by Shiratani et al. [13] has reported good and comparable optical quality outcomes of pIOL with and without a central hole.Except for rare complications, cataract formation is the most frequently revealed problem which is related to ICL implantation (Fernandes et al. 2011). In fact, the prevalence of cataract formation has been widely studied in the context of different ICL models, and different studies indicated that it is more common in older patients and patients with higher myopia (Sanders 2008; Schmidinger et al. 2010; Alfonso et al. 2015). In a study analyzing 781 eyes implanted with V4c ICL model (range 3- 24 months), Alfonso et al. [14] (2015) found any case of cataractous eyes. Similarly meta – analysis study (Packer 2018) described zero incidence of asymptomatic anterior subcapsular cataract formation. Other analysis indicates that Karandikar et al. [6] (2015), Bhandari et al. [6] (2016), Rizk et al. [15] (2019) and Sachdev et al. [7] (2019) reported only in one eye had revealed cataract formation. This complication mainly occurred in 9 months, one year or two years post-op follow-up periods. One of other complications is uncorrected or over corrected rotation of the pIOL. Rotation of lens more than 30° was reported in several studies (Karandikar et al. 2015; Bhandari et al. 2016; Ganesh et al. 2017; Pjano et al. 2017 and Kamiya et al. 2018). This event required re-rotation or lens exchange surgery. A comparative study of rotational stability between spheric and toric models of ICL concluded that both lenses have similar rotational stability (3.39° versus 4.17°, respectively; Hyun et al. 2017) [16].Choi et al. [17] describe the ideal pIOL vault as between 250 and 750 μm. In our study, the mean vault was 471.8± 137.5 μm and the mean minimum vault was 245.2 μm and the mean maximum vault was 755.2 μm during 6 months and this value is much similar with recommended vault. In this study, we investigated first 54 eyes in which were implanted VTICM5 toric ICL model to patients with high myopia and myopic astigmatism in Uzbekistan. The main privilege of these lenses are expended optic size. The optic size in V4c is ranges from 4.9 to 5.8 mm. EVO+ new toric ICL VTICM5 model optic size ranges from 5.0 to 6.1 mm. In this study, we found any significant difference after implantation of this lens. Patients have satisfied with results and visual complaints such as halo and glare at nighttime were significantly decreased.
5. Conclusions
- In summary, initial results of our study indicate that VTICM5 toric ICL new model implantation is safe, effective and provides predictable and stable refractive results in the correction of eyes with high myopia and myopic astigmatism in Uzbekistan. In our opinion, the lens design with expanded optic size and with central hole significantly decreases of complaints on nighttime such as halo and glare. Also adequate patient selection, accurate measurement of all parameters that are required to calculate Toric ICL size and power are all extremely important to achieve good postoperative results in follow-up period. The patient with toric refraction would get high visual performance and had increased quality of life during short post-op period time. We believe and recommend that this procedure is alternative and safe method to patients who has high refractive errors and requires more investigations for long follow-up period after toric ICL implantations.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML