-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(4): 286-289
doi:10.5923/j.ajmms.20211104.06
Received: Mar. 3, 2021; Accepted: Mar. 22, 2021; Published: Mar. 28, 2021

Results of Studying the Structure of Endometric Pathology and Myometry in Women with Abnormal Uterine Bleeding during Perimenopause
Askarova Zebo Zafarjonovna 1, Alieva Dilfuza Abdullaevna 2
1Samarkand Medical Institute, Samarkand, Uzbekistan
2Professor, Doctor of Medical Sciences, Republican Specialized Obstetrics and Gynecology Scientific-Practical Medical Center, Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

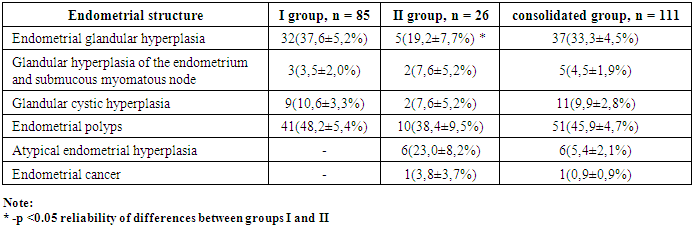
Purpose study of the structure of the endometrium in women with abnormal uterine bleeding during perimenopause. We analyzed the case histories of 125 patients with abnormal uterine bleeding who received inpatient treatment in the gynecological department of the 1st clinic of SamMI from January 2019 to May 2020. According to the histological study of group I, 32 (37.6 ± 5.2%) were diagnosed with glandular hyperplasia of the endometrium, 3 (3.5 ± 2.0%) of patients, glandular hyperplasia of the endometrium was combined with a submucous myomatous node, in 9 (10.6 ± 3.3%) - glandular-cystic hyperplasia of the endometrium, endometrial polyps - in 41 (48.2 ± 5.4%) patients. According to the histological examination of group II scraping, 5 (19.2 ± 7.7%) were diagnosed with glandular hyperplasia of the endometrium, 2 (7.6 ± 5.2%) had glandular cystic hyperplasia, polyps were diagnosed in 10 (38.4 ± 9, 5%), 2 (7.6 ± 5.2%) patients with glandular hyperplasia of the endometrium revealed a submucous myomatous node, atypical endometrial hyperplasia in 6 (23.0 ± 8.2%) and endometrial cancer in 1 (3.8 ± 3.7%) patient. Thus, during histological examination of endometrial scraping in patients with abnormal uterine bleeding in the group with recurrent AMC, atypical endometrial hyperplasia was verified 6 (23.0 ± 8.2%) and endometrial cancer was detected in one patient, while patients of group I had atypical endometrial hyperplasia and no endometrial cancer was detected.
Keywords: Coagulopathic, Oncological alertness, Precancer, Adenomyosis, Submucous myomatous, Endometrial glandular
Cite this paper: Askarova Zebo Zafarjonovna , Alieva Dilfuza Abdullaevna , Results of Studying the Structure of Endometric Pathology and Myometry in Women with Abnormal Uterine Bleeding during Perimenopause, American Journal of Medicine and Medical Sciences, Vol. 11 No. 4, 2021, pp. 286-289. doi: 10.5923/j.ajmms.20211104.06.
1. Introduction
- Abnormal uterine bleeding (AMB) is one of the most common reasons for visiting a gynecologist and performing intrauterine interventions. The term AMB covers severe uterine bleeding, which can be caused by anatomical pathology of the reproductive system and women with normal anatomy in whom AMK can be caused by ovulatory dysfunction, coagulopathic and iatrogenic causes [11,13]. Endometrial hyperplastic processes are a common pathology, the frequency of which increases towards the period of age-related hormonal changes in perimenopause. Endometrial hyperplastic processes in most cases are manifested by abnormal uterine bleeding [12].The most frequent morphological substrate of abnormal uterine bleeding (AMB) during perimenopause in women is endometrial hyperplastic processes [2,5]. As you know, the causes of AMB are chronic anovulation, which is characteristic of this age period of life due to age-related hormonal changes [5].Endometrial hyperplasia (EH) is one of the main forms of pathological proliferative changes in the uterine mucosa, characterized by excessive proliferation of the predominantly glandular and, to a lesser extent, its stromal component. However, one should not forget about oncological alertness.According to a number of authors, in 70% of cases of uterine cancer during perimenopause, hyperplastic processes of the endometrium precede, and in 30-79% of cases within 1-3 years, atypical endometrial hyperplasia turns into cancer [1,5].So, in the studies of Barbieri R.L. et al. the risk of transformation of simple hyperplasia into atypical hyperplasia was about 10.5%, and into endometrial cancer - 2% [7,4].Endometrial polyps, glandular and glandular-cystic hyperplasia of the endometrium refer to background processes and only atypical hyperplasia is a true endometrial precancer. Glandular hyperplasia during perimenopause in 0.4-1% of cases turn into atypical hyperplasia and endometrial cancer. Atypical hyperplasia turns into endometrial cancer in 40% of cases [1]. Precancerous EH transforms into endometrial cancer in 10% of patients (according to different authors, from 2 to 50%) [8,9,10].As you know, the gold standard for determining the background of AMK is morphological - the study of histological preparations of endometrial scrapings [3,9].The aim of our study was to study the structure of the endometrium in women with abnormal uterine bleeding during the perimenopause.
2. Materials and Methods
- We analyzed the case histories of 125 patients with abnormal uterine bleeding who received inpatient treatment in the gynecological department of the 1st clinic of SamMI from January 2019 to May 2020.The age of women varied from 43 to 51 years, on average 46.9 ± 1.6 years. According to generally accepted standards, all patients underwent clinical and anamnesis examination, transvaginal ultrasound examination, and hysteroscopy.As you know, uterine bleeding is a syndrome diagnosis, which can be caused by a large number of different diseases. In the period of per menopause, which is a critical period in terms of the occurrence of various neoplasm’s, with abnormal uterine bleeding, along with ultrasound, a morphological examination of the uterine mucosa is mandatory.
3. Results
- All patients with endometrial hypertrophy 111 (88.8 ± 2.8%), we underwent a morphological examination of scrapings (Table 1). The exception was 14 (11.2 ± 2.8%) in whom the ultrasound diagnosed the thickness of the endometrium from 1 to 4 mm.
|
|
4. Conclusions
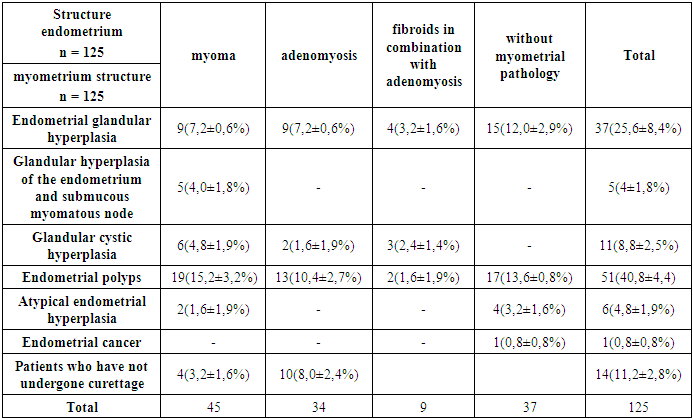
- 1. Thus, during histological examination of endometrial scraping in patients with abnormal uterine bleeding in the group with recurrent AMC, atypical endometrial hyperplasia was verified 6 (23.0 ± 8.2%) and endometrial cancer was detected in one patient, while patients of group I had atypical endometrial hyperplasia and no endometrial cancer was detected.2. Thus, GHPE was detected in 15 (12.0 ± 2.9%) patients without myometrial pathologies, PE was detected in 17 (13.6 ± 0.8%) patients without myometrial pathology, AHE in 4 (3.2 ± 1, 6%) of patients without myometrial pathology and in 1 (0.8 ± 0.8%) patient with endometrial cancer, no myometrial pathology was detected by ultrasound data.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML