A. A. Nizomov
Republican Scientific and Practical Medical Center for Specialized Therapy and Medical Rehabilitation, Tashkent, Uzbekistan
Correspondence to: A. A. Nizomov, Republican Scientific and Practical Medical Center for Specialized Therapy and Medical Rehabilitation, Tashkent, Uzbekistan.
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Thirty patients (group I) with a diagnosis of ACS in the form of an elevated ST segment on an electrocardiogram at the age of 57.9 ± 10.3 years and 30 patients (group II) with a diagnosis of stable angina II-IV were examined. The control group included 20 healthy individuals (50.5 ± 6.1 years). According to the results, there is an increase in the amount of cytokinesIL1β, IL6 and TNF-α based on the immune-inflammatory response in ACS, and the dysfunction of the vascular endothelium is associated with an imbalance of the NO system. Based on TNF-α and IL-6 aggression, the vascular endothelial function is impaired, and endothelial dysfunction (ED) is aggravated by a sharp decrease in NO and eNOS due to the activation of iNOS expression and an increase in ONO2 concentration.
Keywords:
Acute coronary syndrome, Endothelial dysfunction, Cytokines
Cite this paper: A. A. Nizomov, Role of Endothelial Dysfunction and Immuno-Inflammatory Processes in Acute Coronary Syndrome, American Journal of Medicine and Medical Sciences, Vol. 11 No. 4, 2021, pp. 275-279. doi: 10.5923/j.ajmms.20211104.04.
1. Introduction
Today, despite the serious development of medical technologies, ischemic heart disease remains one of the leading causes of disability and death in all developed countries [14]. This, in turn, forces us to seek new opportunities for disease prediction, risk assessment, diagnosis, prevention and treatment. In particular, one of the most dangerous manifestations of ischemic heart disease is acute coronary syndrome (ACS), which is characterized by high mortality and hospitalization among all cardiovascular diseases. At this stage, it is important to show that under the influence of all risk factors, the development of UIC occurs through endothelial dysfunction (ED), which is considered a universal mechanism. Today it is known that endothelial dysfunction depends on the localization of the pathological process, the state of hemodynamic changes and various humoral factors [2]. Thus, the study of the effect on ED and its specificity in ACD is of scientific interest.According to the literature available in recent years [6,7], the development of inflammatory processes based on the pathogenesis of CHD is one of the motivating factors of acute cardiovascular complications. In addition, the inflammatory process plays a significant role in the formation of atherosclerotic plaques, as well as in the formation of stable foci of atheroma with the subsequent development of thrombotic occlusion and cardiovascular complications [1,11]. In turn, this process is mediated by pre-inflammatory cytokines, including interleukins (IL) and tumor necrosis factor-α (TNF-α), which show their effects on the cardiovascular system through various mechanisms. Should note that the pre-inflammatory cytokines IL 6 and TNF-α cause different levels of changes in the vascular wall [12]. However, the enhancement of the synthesis of enzymes of matrix metalloproteinase based on this process is one of the leading factors in the formation of the clinical picture of CHD. Indeed, according to sources in the literature [5], an increase in the amount of IL-6 in the arterial walls indicates the development of atherosclerosis, plaque growth and coronary complications. An epidemiological study conducted over 9 years as part of the Physicians' Health Study [14] showed that increased IL-6 levels in healthy men were associated with an increased risk of myocardial infarction. According to other literature [15], a sharp increase in the amount of IL 6 and S-reactive protein can be considered as a marker of inflammation in the development of ACS. However, the fact that these cytokines lead to ED through their action on the vascular wall can serve as a marker of unstable angina pectoris, myocardial infarction and even ACS, that is, acute forms of CHD [5].Today, in addition to hemodynamic and neurohumoral theories, the interaction of ED with the activation of the immune system has been sufficiently developed. However, the fact that the immune system not only reacts to infectious factors, but also develops its own specific reactions to any stressful influences, including ischemia, exacerbation of hemodynamic disorders and changes in the blood coagulation system, requires further research on this problem. In addition, according to various theories, the development of any disease can be explained by a number of factors, ranging from the negative effects of environmental factors [4] and ending with the profile of the immune status, which is influenced by ED [9]. Therefore, the study of the dependence of the development and progression of ACS ED on the body's immune response in various situations is of scientific and practical importance.The aim of the study was to evaluate changes in pre-inflammatory cytokines and parameters of the NO-system in patients with ACS.
2. Material and Research Methods
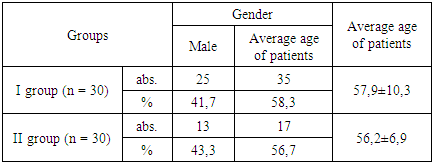
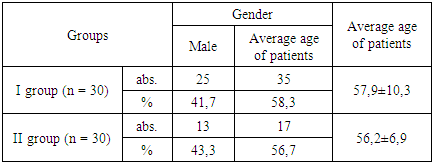
During the study, 30 people (group I) and 30 patients with stable angina pectoris II-IV degrees were hospitalized in the intensive care unit of the Republican Scientific Center for Emergencies with an electrocardiogram from 41 to 56 years old (57.9 ± 10.3). (group II). The control group included 20 healthy individuals (50.5 ± 6.1 years). The groups were approximately the same in age and sex (Table 1).Тable 1. Description of the patients who participated in the study
 |
| |
|
The study did not include patients with grade II arterial hypertension (AH), severe heart failure, complex heart rhythm disturbances, diabetes mellitus, severe liver, kidney, lung and blood diseases. In addition, patients with active inflammatory processes, oncological and immunopathological diseases were excluded from the study.All patients underwent laboratory and instrumental examinations, including electrocardiography (ECG) and echocardiography (EhoCG), taking into account such characteristics as lifestyle, diet, smoking, duration of the disease, heredity and level of physical activity. Endothelial function was assessed by a potentiometric method using chromatography based on the determination of the levels of nitrates (NO3) in plasma and erythrocytes and the amount of L-arginine in the plasma. ImmunoassaysIL1β, IL6 andTNF-α were used to study the immune-inflammatory process.Statistical processing of the research results was carried out using the Microsoft Office Excel 2013 software package and the established statistical methods. Correlation analysis used Pearson's level (r) and Spearman's correlation.
3. Results and Its Discussion
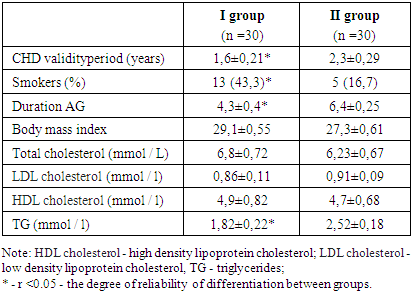
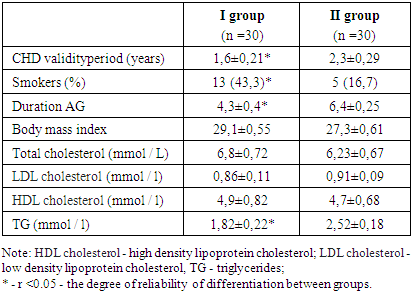
Most of the patients who took part in the study were women - 61.7%. Based on the analysis of the data of the anamnesis of the disease, the average age of patients at the time of the appearance of the first signs of PEC was 47.1 ± 4.9. With the onset of the first symptoms, the mean time to CHD diagnosis was 6.7 ± 1.22 months. In turn, the patients developed chest pain and took an average of 2.1 ± 0.83 hours to be admitted to hospital with ACS. According to the results obtained, i.e. Table 2, in both groups of patients, dyslipidemia and overweight were observed. Alternatively, there was a difference (p <0.05) between groups in the duration of hypertension. At the same time, there were more cases of ACS (p <0.05) due to smoking.Table 2. Clinical description of the patients who participated in the study
 |
| |
|
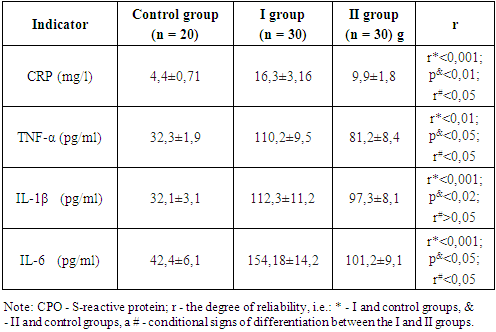
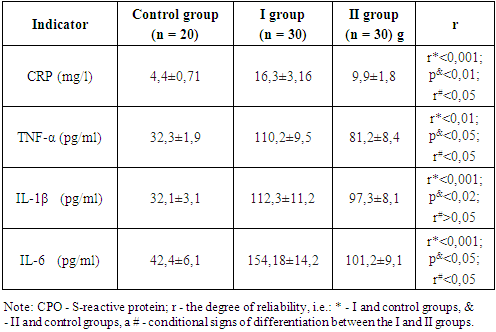
It is known that inflammatory processes based on specific ischemic changes in the myocardium that are observed due to coronary atherosclerosis also play an important role in CHD. Among the wide range of immunological markers used to assess the activity of the inflammatory process, the most studied is C-reactive protein (CRP), which belongs to the family of proteins of the acute phase of inflammation. The results showed that there were statistically significant differences between the three groups in the CRP. At the same time, with ACS, i.e. in group I, this indicator (table 3) differed 4 times (r <0.001) compared with the control group and 2 times (r <0.05) compared with group II. So, as mentioned above, certain stress in the body is expected to lead to structural changes due to the response of the immune process to the situation. In particular, activation of the cytokine system in the mechanism of the immune system is aimed at tissue repair, depending on the degree of ischemic state of the myocardium in ACS [5]. Among them, TNF-α is one of the most important mediators of inflammatory reactions; it is involved in many reactions in combination with other cytokines. In particular, it stimulates the formation of pathological NO through NOS-2. In addition, it increases the expression of adhesive receptors in the endothelium, enhances the migration of leukocytes into tissues and leads to the destruction of endothelial cells [3]. As a result, the activation of effector cells leads to the formation of inflammatory mediators. Indeed, the study showed that the amount of TNF-α increased depending on the exacerbation of ischemic conditions in the myocardium, i.e., as shown in Table 3, in contrast to the control and group II, this cytokine was significantly present in group I (r <0, 01 and r <0.05 respectively).Table 3. Indicators of the immune-inflammatory process, M ± m
 |
| |
|
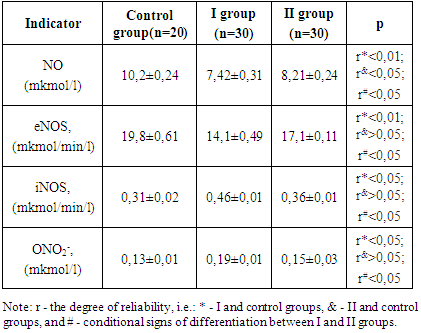
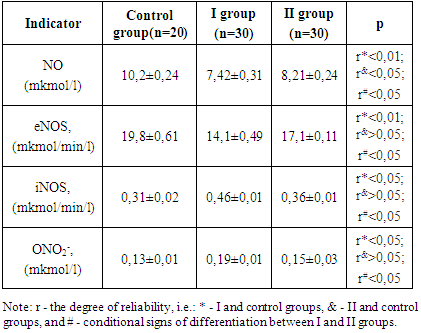
IL-6 normally activates endothelial cells, facilitating the expression of the cell adhesion molecule [5]. In turn, the cell adhesion molecule located in the arterial vessel wall is an important factor in the development and progression of atherosclerosis. According to the results of our research, the IL-6 CHD increased its volume as a result of the improvement in the situation (Table 3). At the moment, it was quite different (r <0.001 and r <0.05 respectively) in group I compared to the control in group II. In addition, in patients with CHD, an increase in the level of IL 1β was observed compared with healthy people, but the numbers between groups I and II were not statistically significant.Thus, according to the results obtained, in ACS, an immune-inflammatory response is observed with an increase in the amount of cytokines IL 1β, IL 6 and TNF-α in the serum of patients. Therefore, it is desirable to determine the role of cytokines in the development of ED.It should be noted that the effect of pre-inflammatory cytokines on myocardial function is mediated by modulation of endogenous NO production [8]. In this case, cardiomyocytes represent such types of NO synthesis (NOS) as eNOS and iNOS. In turn, eNOS activity is controlled by myocardial contraction, while iNOS depends on the amount of cytokines [10].It is known that NO serves as a major factor in vasodilation. In this case, the NO level is regulated by eNOS. In turn, when eNOS is reduced due to hypoxia and ischemia, iNOS comes to the fore as the main source of NO production in tissues. In addition, the presence of iNOS produces 100-1000 times more NO than eNOS [13]. Therefore, NO has vasoconstrictor properties rather than a vasodilator. In addition, when NO is overexposed, the processes leading to the formation of superoxide anion radical (O2) are simultaneously intensified.Under these conditions, NO is synthesized with O2- to form the highly cytotoxic compound ONO2. In turn, the study of the vascular NO-system revealed differences between the indicators of the groups.As can be seen from Table 4, the NO and eNOS values in group I were significantly different from those in the other groups with a sharp decrease compared to the control group (r <0.01). In turn, in group I iNOS and ONO2 - a statistically significant increase (r<0.05) was observed.Table 4. Indications of endothelial vascular function, M ± m
 |
| |
|
Thus, in patients with ACS, there was a significant decrease in serum NO - 27.2% and eNOS - 28.8% (Fig. 1).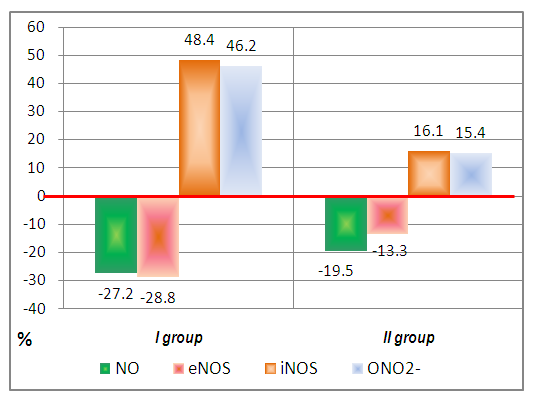 | Figure 1. Change in the productivity of the NO-system in the groups relative to the control group (red line) (%) |
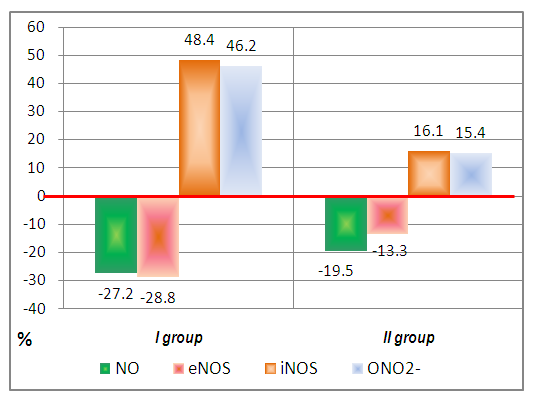
Thus, vascular endothelial dysfunction in ACS is associated with an imbalance of the NO-system, in which ED is formed due to a sharp decrease in NO and eNOS due to activation of iNOS expression and an increase in ONO2 concentration.The study of changes in ED levels in relation to the profile of cytokines observed in ACS was carried out based on the analysis of correlation correlations between indicators.Based on analysis, TNF-α and IL-6 positively correlated with iNOS and ONO2 in the control group and negatively correlated with NO and eNOS. In turn, increases in serum TNF-α and IL-6 in UIC patients, especially OCD (group I), reversed these associations. As can be seen from Figure 2, the graph of the NO-system indicators, based on the results of their correlation with these cytokines, was transformed into a horizontal diamond in the control group, while in the control groups I and II. At the same time, the correlation of iNOS and ONO2 with TNF-α was positive in the control group r = 0.56 and r = 0.33, respectively, and in patients of group I these indicators turned into a negative feedback (r = -0.65 and r = - 0.57; r <0.05). However, the correlation of NO and eNOS with TNF-α was inversely correlated based on the increase in this cytokine in patients (groups I and II), appeared to be correct binding (group I: r = 0.52 and r = 0.6, respectively; r <0, 05). In addition, the correlation of iNOS and ONO2 with IL-6 turned out to be correct in healthy people (r = 0.43 and r = 0.73, respectively), while in patients of group I this correlation was inversely proportional (r = -0, 65 and r. = -0.76, respectively; r <0.05). | Figure 2. Correlation between NO-system and cytokines |
Thus, in ACS, vascular endothelial dysfunction is exacerbated on the basis of the immune-inflammatory process, i.e. aggression of pre-inflammatory cytokines TNF-α and IL-6.
4. Conclusions
Thus, there is an increase in the amount of cytokines IL 1β, IL 6 and TNF-α based on the immune-inflammatory response in ACS, and the dysfunction of the vascular endothelium is associated with an imbalance of the NO-system. Based on the aggressiveness of TNF-α and IL-6, vascular endothelial function is impaired. At the same time, ED is aggravated by a sharp decrease in NO and eNOS due to activation of iNOS expression and an increase in ONO2 concentration.
References
| [1] | Abbas M. et al. Endothelial microparticles from patients with acute coronary syndrome cause premature aging of coronary artery endothelial cells and thrombogenicity: the role of Ang II / AT1 receptor / NADPH oxidase in the activation of MAPK and PI3 kinase pathways // Circulation. - 2017. - T. 135. - No. 3. - S. 280-296. |
| [2] | Abbate R. et al. Thrombosis and acute coronary syndrome // Thrombotic research. - 2012. - T. 129. - No. 3. - S. 235-240. |
| [3] | Adams MR. Clinical assessment of endothelial function. Endothelium. 2006.13 (6): 367-374. |
| [4] | Akhmedov K. et al. Changes in the immune system in rheumatoid arthritis against the background of the influence of environmental factors // International Journal of Advanced Science and Technology. Vol. 29, no. 5, (2020), pp. 1907-1917. |
| [5] | Cherneva ZV et al. Inflammatory cytokines at admission - independent prognostic markers in patients with acute coronary syndrome and hyperglycemia // Emergency cardiac care. - 2012. - T. 14. - No. 1. - S. 13-19. |
| [6] | Corti R., Fuster V., Badimon J. J. Pathogenetic concepts of acute coronary syndromes // Journal of the American College of Cardiology. - 2003. - T. 41. - No. 4S. - S. S7-S14. |
| [7] | Forte L. et al. C-reactive protein is released into the coronary circulation and causes endothelial dysfunction in patients with acute coronary syndromes // International Journal of Cardiology. - 2011. - T. 152. - No. 1. - S. 7-12. |
| [8] | Gaubert M. et al. Uric acid levels are associated with endothelial dysfunction and severity of coronary atherosclerosis during the first episode of acute coronary syndrome // Purinergic signaling. - 2018. - T. 14. - No. 2. - S. 191-199. |
| [9] | Lu Y. et al. Endothelial microparticles have different effects on Th1 functions in patients with acute coronary syndrome // International Journal of Cardiology. - 2013. - T. 168. - No. 6. - S. 5396-5404. |
| [10] | Matsuzawa Y., Lerman A. Endothelial dysfunction and coronary heart disease: assessment, prognosis and treatment // Ischemic heart disease. - 2014. - T. 25. - No. 8. - P. 713. |
| [11] | Oz F., Gul S., Kaya MG, Yazychi M., Bulut I., Elitok A., Ersin G. et al. Does aspirin prevent acute coronary syndrome in patients with pneumonia: a multicenter prospective randomized trial ... Coron Artery Dis. 2013. 24 (3): 231-237. |
| [12] | Srikanth Babu B. MV et al. Polymorphisms of cytokine genes in predisposition to acute coronary syndrome // Genetic testing and molecular biomarkers. - 2012. - T. 16. - No. 5. - S. 359-365. |
| [13] | Zahid JA et al. The effect of melatonin on endothelial dysfunction in patients after acute coronary syndrome: a randomized clinical trial MEFACS // Journal of Pineal Research. - 2019. - T. 67. - No. 3. - S. e12600. |
| [14] | Mayanskaya SD, Kuimov AD Endothelial dysfunction and acute coronary syndrome // Russian Journal of Cardiology. - 2001. - No. 2. - S. 76-84. |
| [15] | Rebrov AP, Sazhina E. Yu., Toma M. Ya. Endothelial dysfunction and changes in the level of cytokines and C-reactive protein in severe chronic heart failure // Russian Journal of Cardiology. - 2005. - No. 2. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML