Salimova G. Kh.1, Najmutdinova D. K.2, Urunbayeva D. A.3, Sadikova N. G.3, Adkhamova N. P.3, Razakova F. S.4
1Independent Researcher, Tashkent Medical Academy, Tashkent, Uzbekistan
2Doctor of Science, Professor, Tashkent Medical Academy, Uzbekistan
3PhD, Tashkent Medical Academy, Tashkent, Uzbekistan
4Independent Researcher, National University of Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
This article presents modern views on the impact of chronic heart failure on the clinical course of patients with type 2 diabetes mellitus, as well as an assessment of the quality of life of patients in this category.
Keywords:
Type 2 diabetes mellitus, Chronic heart failure, Insulin resistance, Quality of life
Cite this paper: Salimova G. Kh., Najmutdinova D. K., Urunbayeva D. A., Sadikova N. G., Adkhamova N. P., Razakova F. S., Assessment of the Clinical Condition and the Quality of Life of Patients with Type 2 Diabetes Mellitus and Chronic Heart Failure, American Journal of Medicine and Medical Sciences, Vol. 11 No. 4, 2021, pp. 271-274. doi: 10.5923/j.ajmms.20211104.03.
1. Introduction
Diabetes mellitus is one of the most important socially and economically significant problems of modern society. According to statistics from the research of the International Diabetes Federation (IDF), 425 million patients with diabetes mellitus (DM) were registered in 2017 and, according to forecasts, this figure will increase by about 1.5 times by 2045 and will amount to 629 million people. At the same time, 2/3 of all patients are in the age group from 20 to 64 years old, which indicates the rejuvenation of the pathology and its widespread prevalence among the working population [1].Despite the advances achieved in the diagnosis and treatment of this pathology, by the time type 2 diabetes is detected, half of the patients already have complications leading to a decrease in the quality of life, early disability and premature death [2]. It is known that the main cause of death in 52% of patients with diabetes is chronic heart failure (CHF) [3]. The combination of type 2 diabetes mellitus with CHF is a frequent prognostically unfavorable combination that worsens not only the quality of life of patients, but also the prognosis. Data were obtained indicating the existence of a causal relationship between these two pathologies [4] and the study of this issue is an urgent topic at the moment. Purpose of the work: To assess the clinical condition and quality of life (QOL) in patients with type 2 diabetes and chronic heart failure.
2. Material and Methods
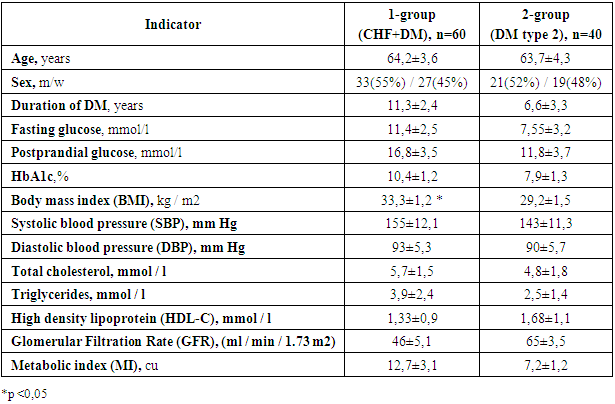
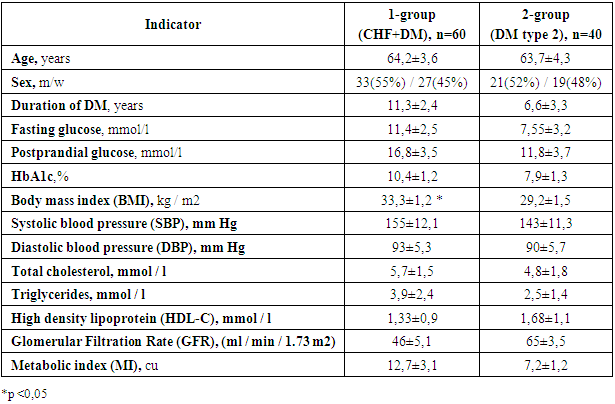
The study included 100 patients with a reliable diagnosis of type 2 diabetes at the age from 56 to 72 years. Of these, the main group (1), n = 60, average age (64.2 ± 3.6) years, consisted of patients with type 2 diabetes with CHF II-III FC according to the NYHA classification. The control group (2) included patients with type 2 diabetes without signs of CHF (n = 40), average age (63.7 ± 4.3) years. Both groups were matched for gender and age. The general clinical and functional status of patients included in the study is presented in Table 1.Table 1. General clinical and functional status of patients
 |
| |
|
All patients included in the study underwent a general clinical examination, measurement of blood pressure (BP), determination of body mass index (BMI), electrocardiography (ECG) in 12 standard leads and echocardiography with determination of ejection fraction (EF) of the left ventricle (LV). The biochemical blood test was also performed: determination of fasting and postprandial glucose levels, glycated hemoglobin (HbA1c), total cholesterol, triglycerides, HDL, LDL.Insulin resistance (IR) was assessed using a new metabolic index (MI), patented in 2014. [5], which was calculated by the formula: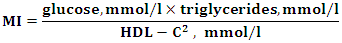 indicators: MI - metabolic index, glucose - fasting plasma glucose concentration (mmol / l), HDL-C - high density lipoprotein level (mmol / l).IR was set at MI ≥7 c.u. The higher the MI numbers, the more pronounced the IR. In addition, all patients were examined for diabetes complications. To diagnose diabetic neuropathy, each patient underwent a study of vibration, tactile, temperature and pain sensitivity. Diagnosis of diabetic retinopathy was performed using ophthalmoscopy at the enlarged pupil. The presence of CKD was determined by the level of GFR. This indicator was calculated taking into account the level of plasma creatinine using the validated formula CKD-EPI (developed by the Collaboration on the Epidemiology of Chronic Kidney Disease), which best correlates with the reference (clearance) methods of determination [6]. The quality of life of patients was assessed using the SF-36 questionnaire.
indicators: MI - metabolic index, glucose - fasting plasma glucose concentration (mmol / l), HDL-C - high density lipoprotein level (mmol / l).IR was set at MI ≥7 c.u. The higher the MI numbers, the more pronounced the IR. In addition, all patients were examined for diabetes complications. To diagnose diabetic neuropathy, each patient underwent a study of vibration, tactile, temperature and pain sensitivity. Diagnosis of diabetic retinopathy was performed using ophthalmoscopy at the enlarged pupil. The presence of CKD was determined by the level of GFR. This indicator was calculated taking into account the level of plasma creatinine using the validated formula CKD-EPI (developed by the Collaboration on the Epidemiology of Chronic Kidney Disease), which best correlates with the reference (clearance) methods of determination [6]. The quality of life of patients was assessed using the SF-36 questionnaire.
3. Results and Discussion
Analysis of the data obtained showed that the patients of both groups had diabetes decompensation. Thus, the levels of fasting and postprandial glycemia in the DM and CHF group were significantly higher than in patients with diabetes alone (11.4 mmol / L and 16.8 mmol / L versus 7.55 mmol / L and 11.8 mmol / L, respectively. Also, the median HbAlc in both groups (10.4% and 7.6%, respectively) significantly exceeded the normal indicators. (see Chart 1). 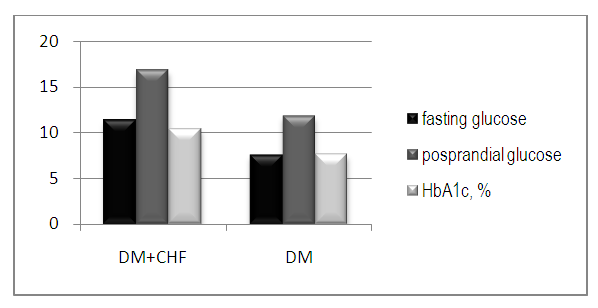 | Chart 1. Indicators of the carbohydrate metabolism |
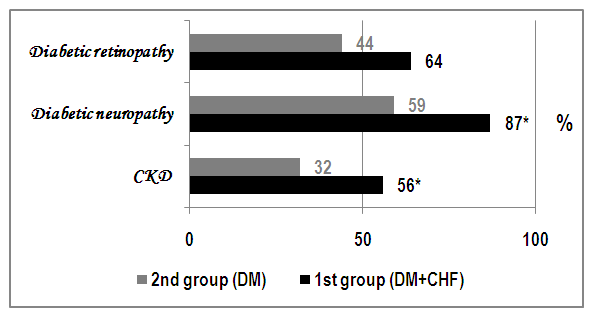
In our opinion, this can be explained primarily by insufficient control of the parameters of the carbohydrate metabolism in patients with CHF. Also, longer duration of the disease in the main group on the background of a higher IR may indirectly indicate the depletion of the reserve capacity of the pancreas, which causes decompensation of diabetes mellitus. The average blood pressure in the control group was lower than in the main group. In the control group: SBP 143 ± 11.3 mm Hg, DBP 90 ± 5.7 mm Hg, and in the main group - SBP 155 ± 12.1, DBP 93 ± 5.3. Also, in the main group, BMI numbers were significantly higher (33.3 ± 1.2 kg / m2) compared with the control group, where this indicator was 29.2 ± 1.5 kg / m2 (see Table 1). After the diagnosis of complications of diabetes mellitus, such as diabetic retinopathy, neuropathy and nephropathy, differences in the frequency of their occurrence were noted in both groups. In general, chart 2 clearly shows that the indicators in the 1st group were higher than in the 2nd in all three categories. So, after studying various types of sensitivity, it was found that diabetic distal symmetric sensory neuropathy, being the most common complication of diabetes in both groups, was found in 87% of patients in group 1, while in group 2, this indicator was 28% lower. The incidence of other complication of diabetes, diabetic retinopathy, was also higher in the study group, where this indicator was 20% higher than in the control group, 64% and 44%, respectively. CKD, being an equally serious complication, was found in more than half of the patients in the study group and in 32% of patients in the control group.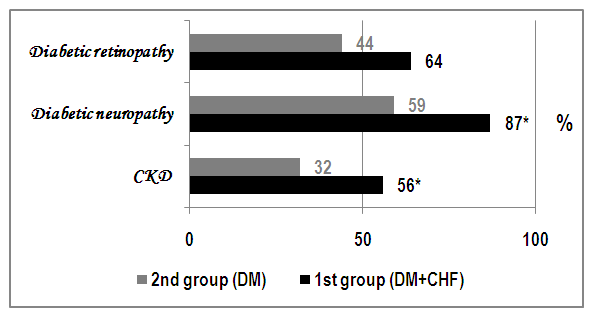 | Chart 2. The frequency of the diabetes mellitus complications. (*p <0,05) |
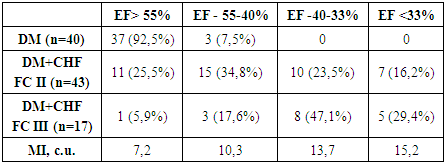
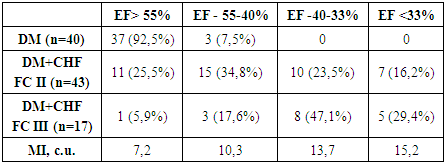
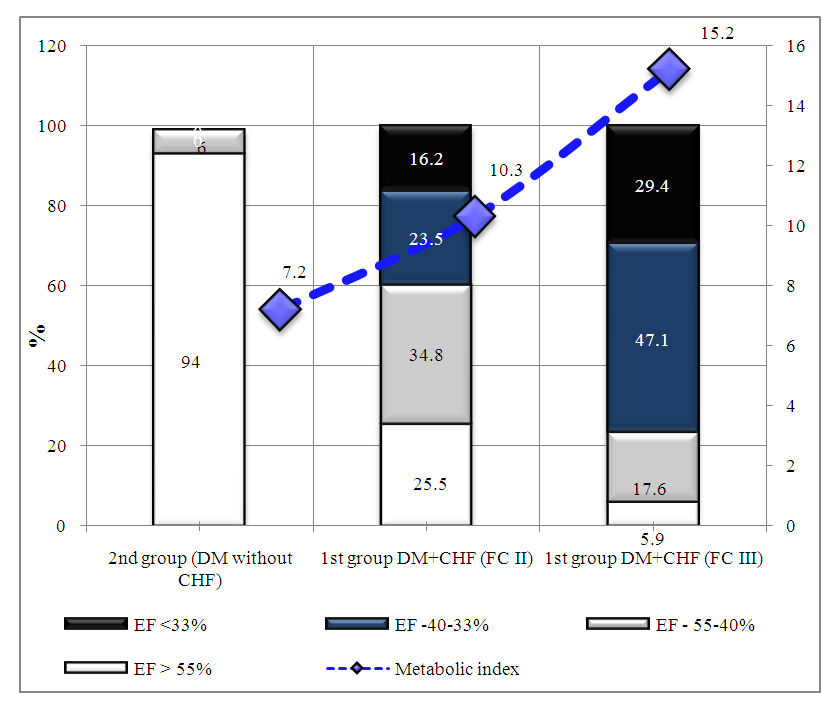
GFR numbers were also worse in patients with a combination of DM and CHF. So, in the main group, the GFR was 46 ± 5.1 ml / min / 1.73 m2, while in the control group it was 65 ± 3.5 ml / min / 1.73 m2 (see Table 1). The duration of diabetes mellitus, poorer glycemic control, and depletion of the reserve capacity of the pancreas explain the decrease in renal function in this group of patients. At the same time, patients without CHF had preserved GFR, even against the background of DM decompensation. Apparently, impaired renal function in this category of patients occurs much later. Thus, it is the combination of diabetes mellitus with chronic heart failure that has a pronounced negative effect on renal function; moreover, the severity and duration of diabetes mellitus are of decisive importance in this case. The same conclusion can be drawn regarding other diabetic complications of diabetes. The analysis of MI numbers showed that the patients of both groups showed an increase in this indicator above 7 с.u., which indicated that they had insulin resistance (see Table 1). However, MI of patients of the main group, in contrast to the control group, was significantly higher (12.7 ± 3.1 с.u. versus 7.2 ± 1.2 с.u.). In addition, in this category of patients, the EF indices varied widely, therefore, to simplify the analysis of the data obtained, it was decided to divide the main group into 2 subgroups depending on the FC of CHF (see Table 2). The table clearly shows how the MI numbers increase with a decrease in EF: in the patients of the control group, EF was above 55% and, at the same time, there was a low IR indicator - 7.2 c.u. Оn the contrary, the patients of the main group had a pronounced IR - MI above 10 a.u. with EF below 55%, as well as even more pronounced IR with EF below 33% - 15.2 conventional units. (see table 2). Table 2. MI and EF indicators in patients of both groups
 |
| |
|
Also, the average MI indices in each subgroup were calculated depending on the FC of CHF. So, with CHF II FC MI was equal to 10.3 ± 2.3 с.u., and with CHF III FC - 15.2 ± 1.5 с.u. (see chart 3). Thus, after analyzing the data of the main group, we came to the conclusion that there is a relationship between the severity of insulin resistance and the functional class of CHF.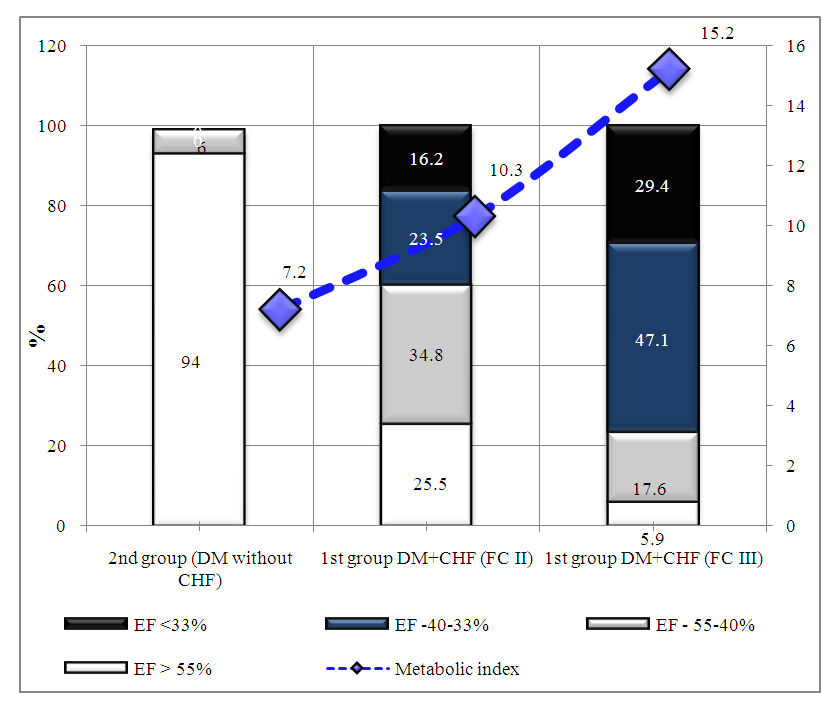 | Chart 3. Metabolic index indicators with and without CHF (taking into account EF of the LV) |
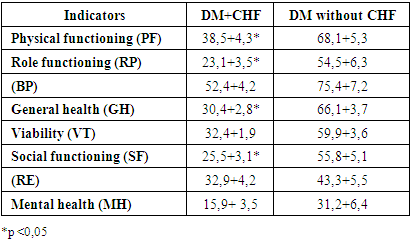
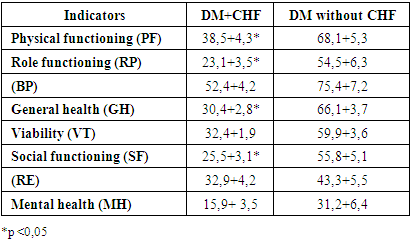
Data from a number of studies, as already mentioned, indicate a direct relationship between the severity of CHF and IR and / or GI [7,8,9,10]. So, after analyzing our data (MI and LVEF), we came to the conclusion that there is a relationship between the severity of IR, CHF FC and EF of the LV. However, in order to find out exactly how the deterioration of only one FC is reflected in the course of diabetes, a larger number of patients and a longer period of observation of the clinical state of patients and indicators of carbohydrate metabolism, C-peptide, and other neurohormones are needed. It should be noted that to assess the severity of IR, we used not the HOMA-IR, but a new metabolic index. As you know, to calculate HOMA-IR it is necessary to study the fasting insulin level, but to calculate MI this indicator is not needed. From a practical point of view, this method for assessing RI is convenient, simple and does not require additional economic costs, since to calculate it, routine laboratory data are sufficient.The analysis of the quality of life indicators showed that in the main group the values were significantly lower, in particular, in such indicators as general health, vitality, physical, role and social functioning, significant differences were obtained (see Table 3). These indicators were lower in the main group and this fact confirms the negative impact of the combined pathology on the condition of patients, because as mentioned above, decompensation and a longer course of diabetes mellitus, poorer glycemic control and hemodynamic disturbances restrict the life of patients.Table 3. Results of assessing the quality of life in patients of both groups
 |
| |
|
4. Conclusions
1. An increase in the functional class of CHF leads to the decompensation of type 2 diabetes.2. The most common complication in both groups was diabetic neuropathy (86% and 59%). Diabetic nephropathy and retinopathy in frequency in both groups were approximately the same.3. With an increase in the functional class of CHF, the MI index increases and the severity of insulin resistance increases.
References
| [1] | IDF Diabetes Atlas 2017, 8th edition. |
| [2] | Ametov A.S., Kurochkin I.O., Zubkov A.A. Diabetes mellitus and cardiovascular diseases / Endocrinology. Thyroidology № 5 (51), 2015. P. 52-58. |
| [3] | Eurich D.T., Weir D.L., Majumdar S.R. et al. Comparative safety and effectiveness of metformin in patients with diabetes and heart failure: systematic review of observational studies involving 34000 patients. Circ Heart Fail. 2013. № 6 (3). Р. 395-402. |
| [4] | O. Iu. Narusov, Iu. V. Lapina, V. Iu. Mareev, M.G. Bolotina, M.V. Shestakova, V. P. Masenko, N. A. Baklanova, Iu. N. Belenkov Influence of chronic cardiac failure severity on the course of comorbid type 2 diabetes mellitus. Ter Arkh 2009; 81(9): 52-7. |
| [5] | Roitberg G.E., Dorosh Zh.V., Sharhun O.O. and others. Possibilities of using a new metabolic index in assessing insulin resistance in clinical practice. Rational pharmacotherapy in cardiology. - 2014. No. 3. P. 264-274. |
| [6] | Levey AS, Stevens LA, Schmid CH, et al. for the CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A New Equation to Estimate Glomerular Filtration Rate. Ann Intern Med. 2009 May 5; 150: 604-612. PubMed ID: 19414839. |
| [7] | Paolisso G., Tagliamonte M.R., Rizzo M.R. et al. Prognostic importance of insulin-mediated glucose uptake in aged patients with congestive heart failure secondary to mitral and/or aortic valve disease. Am J Cardiol 1999; 83 (9): 1338- 1344. |
| [8] | Suskin N.3 McKelvie R.S., Burns RJ. et al. Glucose and insulin abnormalities relate to functional capacity in patients with congestive heart failure. Eur Heart J 2000; 21(16): 1368-1375. |
| [9] | Swan J.W., Anker S.D., Walton С et al. Insulin resistance in chronic heart failure relation to severity and etiology of heart failure. J Am Coll Cardiol 1997; 30(2): 527-532. |
| [10] | M. E. Statsenko, S. V. Fabritskaya, S. V. Turkina, S. S. Shalaeva. The clinical significance of determining insulin resistance in patients with chronic heart failure and type 2 diabetes mellitus. Bulletin of Volgograd State Medical University. Issue 1 (57). 2016: P.78-82. |


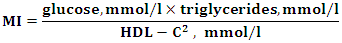 indicators: MI - metabolic index, glucose - fasting plasma glucose concentration (mmol / l), HDL-C - high density lipoprotein level (mmol / l).IR was set at MI ≥7 c.u. The higher the MI numbers, the more pronounced the IR. In addition, all patients were examined for diabetes complications. To diagnose diabetic neuropathy, each patient underwent a study of vibration, tactile, temperature and pain sensitivity. Diagnosis of diabetic retinopathy was performed using ophthalmoscopy at the enlarged pupil. The presence of CKD was determined by the level of GFR. This indicator was calculated taking into account the level of plasma creatinine using the validated formula CKD-EPI (developed by the Collaboration on the Epidemiology of Chronic Kidney Disease), which best correlates with the reference (clearance) methods of determination [6]. The quality of life of patients was assessed using the SF-36 questionnaire.
indicators: MI - metabolic index, glucose - fasting plasma glucose concentration (mmol / l), HDL-C - high density lipoprotein level (mmol / l).IR was set at MI ≥7 c.u. The higher the MI numbers, the more pronounced the IR. In addition, all patients were examined for diabetes complications. To diagnose diabetic neuropathy, each patient underwent a study of vibration, tactile, temperature and pain sensitivity. Diagnosis of diabetic retinopathy was performed using ophthalmoscopy at the enlarged pupil. The presence of CKD was determined by the level of GFR. This indicator was calculated taking into account the level of plasma creatinine using the validated formula CKD-EPI (developed by the Collaboration on the Epidemiology of Chronic Kidney Disease), which best correlates with the reference (clearance) methods of determination [6]. The quality of life of patients was assessed using the SF-36 questionnaire.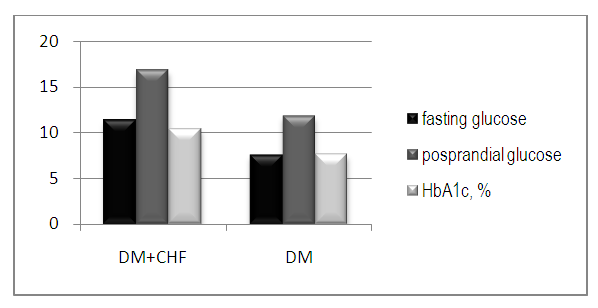
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML