-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(3): 253-260
doi:10.5923/j.ajmms.20211103.19
Received: Mar. 2, 2021; Accepted: Mar. 24, 2021; Published: Mar. 28, 2021

Research on Hypnosis at the Doctor D Hospital of Uzbekistan
Sakellion D. N.1, Irgashev D. S.2, Alimov U. Kh.3, Sultanov Sh. Kh.4, Dikeos D.5
1Doctor of Psychology, Psychiatrist, Scientific Consultant at the Multidisciplinary Hospital "Doctor D", Associate Professor of the Department of Therapeutic Directions III, Tashkent State Dental Institute, Uzbekistan
2Candidate of Medical Sciences, Director of the Multidisciplinary Hospital "Doctor D", Uzbekistan
3Professor, Head, Department of the Tashkent Institute for Advanced Training of Doctors, Uzbekistan
4Associate Professor of the Department of Therapeutic Directions III, Tashkent State Dental Institute, Uzbekistan
5Professor of Psychiatry Department of Athens «Kapodistrian» University Medical School, Athens, Greece
Correspondence to: Sakellion D. N., Doctor of Psychology, Psychiatrist, Scientific Consultant at the Multidisciplinary Hospital "Doctor D", Associate Professor of the Department of Therapeutic Directions III, Tashkent State Dental Institute, Uzbekistan.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Hypnotherapy has been successfully used as an effective method for treating neuroses, affective, dissociative, emotional and behavioral disorders. Encephalographic methods of recording the psychotherapeutic effect of hypnotherapy have been studied. Differences in the EEG activity of the brain in hypnotic catalepsy and in the state of catatonic stupor in schizophrenia were found. Clinical hypnosis is the most dynamic method of psychotherapy, and experimental hypnosis is a unique scientific method for studying human mental processes.
Keywords: Hypnosis, Catalepsy, EEG, Schizophrenia, Psychotherapy
Cite this paper: Sakellion D. N., Irgashev D. S., Alimov U. Kh., Sultanov Sh. Kh., Dikeos D., Research on Hypnosis at the Doctor D Hospital of Uzbekistan, American Journal of Medicine and Medical Sciences, Vol. 11 No. 3, 2021, pp. 253-260. doi: 10.5923/j.ajmms.20211103.19.
Article Outline
1. Introduction
- Psychiatrists around the world, arguing the positive impact of behavioral, cognitive, psychoanalytic and other types of psychotherapy on the patient's psyche, provide objective parameters obtained using the latest advances in modern technology (MRI, PET, SQUID, digital EEG). These laboratory methods allow visualizing the processes of anatomical and physiological changes occurring in the brain as a result of psychotherapeutic treatment.The Universal Decimal Classification system recognizes with the code 612.821.71. "Hypnosis and the physiological nature of suggestion in hypnosis."In Greece, some well-known scientists recommend the use of hypnosis in the treatment of a number of diseases that often cannot be treated with medicinal preparations. [1,2,3,4].In the West in America, England, France, Germany, Italy, Canada and Australia, many psychotherapists use hypnosis in their practice [5,6,7,8,9,10,11]. All publications of Harrison's Principles of Internal Medicine, without exception, recommend the use of hypnosis for therapeutic purposes [12,13,14].In Uzbekistan, in the Hospital "Doctor D" in Tashkent and the higher educational institutions of the country, for many years, together with Greek scientists, hypnotherapy has been studied, taught, practiced and popularized. [15,16,17,18,19,20,21,22].In psychiatry, psychokinetic disorders are often observed, which are based on a violation of volitional processes. The cause of such disorders is not always organic brain damage, metabolic or hormonal disorders of the organism, or the impact of physical or chemical environmental factors, it may be a response to chronic stress [23,24,25,26].Hypnosis is a psychotechnical method that allows you to transfer the patient to an altered state of consciousness, which increases the suggestibility of a person. The quality and degree of the patient's suggestibility depends on the level of his hypnotizability, his active participation in the process of hypnotherapy, confidence in the hypnologist and the level of preparedness of the hypnotherapist. Objectification of the results of therapy is important [27,28,29].The method of clinical hypnosis includes various techniques of muscle relaxation and autosuggestion. The patient may be in a state of sensory deprivation contributing to maintaining contact only with the hypnotherapist (repport), and ignoring any external influences [30].The main symptoms of clinical hypnosis studied by most scientists are such as anesthesia, non-medicinal analgesia, hallucinations in altered states of consciousness [31]. In some cases, such states resemble euphoria with the use of psychoactive substances and religious ecstasy [32].
2. Goal and Tasks
- The purpose of this work is to analyze some diseases that can be treated by the method of suggestion in hypnosis. Comparison of the available information with our own research in hypnotherapy.
3. Methods and Materials
- Analyzing the possibilities of using clinical hypnosis, we tried to systematize diseases in the treatment of which hypnosis is especially effective:Psychosomatic disorders (migraine, irritable bowel syndromes, chronic pain and chronic fatigue, tenonditis, bronchial asthma attacks, dermatitis, etc.) [33,34,35,36].Mental (amnesia of various etiologies, dissociative and somatoform disorders, phobias, chronic anxiety problems, etc.) [37,38,40,41].Neurotic disorders (sleep disorders, a state of intense arousal, sexual impotence, interpersonal problems) [42,43,44].Drug and alcohol addiction [45,46,47,48].It is believed that psychological stress and hereditary factors can cause memory loss and disruption of connections between the constituent elements of human consciousness. This leads to amnesia, fugue or multiple personalities and relationship problems. Psychogenic amnesia is usually caused by severe trauma associated with natural disasters, wars, personal losses, psychosocial conflicts, etc.Dissociative memory disorders are characterized by a change or impairment of the integral and organized functioning of memory, consciousness and self-identification [3,49,50].The emergence of dissociative symptoms is accompanied by a decrease in the level of anxiety and, as a consequence, the syntony of the personality increases (interest, attention, sympathy and concern for other people). However, the symptomatology itself can lead to patient disability.The symptoms of dissociative disorder cause significant internal discomfort, disruption of work in social, professional or other important areas of a person's functioning.Dissociative amnesia is defined as having one or more episodes of inability to retrieve important personal information from memory. This condition is usually traumatic and distressing to the patient. During the episode, the person is embarrassed and confused in thinking, cannot remember "who is he?" Amnesia usually occurs suddenly and can take minutes, days, or even longer.The dissociative fugue has all the features of dissociative amnesia, combined with purposeful movement of the personality that goes beyond the usual daily limit. Although amnesia occurs during the fugue, to outside observers, the patient's behavior during this time may seem completely normal.Fugue is characterized by amnesia with an inability to remember the past and accept a new identity in whole or in part. Suddenly, an unexpected fugue can last for months.The return to the previous identity in cases of fugue and dissociative amnesia with memory recovery can occur after a few hours, but can take long periods of time. If the stress factors that led to the occurrence of these conditions reappear or continue to exist, then a relapse is possible [51].Narcohypnosis using amobarbital is reported to help restore lost memories. When memory returns, patients need help to understand the reasons that led to memory loss and to resolve the problems that caused this disorder.Recovering the memory of a painful event or conflict during clinical hypnosis can not only bring the patient back to the event, but also bring emotional relief to the patient. [3,7].Psychotherapy helps patients reconstruct past traumatic experiences and reduce their pathogenic effects. [50].Professors Masdrakis V., Zervas I.M., Liapas I.A., 2013 [34] proposed a variant of cognitive and behavioral psychotherapy with objectively confirmed results of treatment of generalized anxiety disorder in which a subject's memory disorder occurs [40]. However, dissociative disorders and fugue can be effectively controlled by suggestion in clinical hypnosis [11].Modern brain research has shown that depression-related anxiety leads to a decrease in the volume of the frontal cortex, hippocampus and basal ganglia and an increase in the volume of the amygdala in the left hemisphere. A decrease in the response to stress factors of the external or internal environment decreases metabolic activity in the dorsal part and increases it in the ventricular part of the frontal lobe of the cerebral cortex and adjacent to the limbic nuclei of the thalamus of the left temporal lobe [52].Perhaps hypnotherapy will help turn off this pathological mechanism and promote the regeneration of brain structures [53,54,55,56].
4. Results
- In a long-term study of hundreds of volunteers and patients from various psychiatric hospitals, we used the method of clinical hypnosis with parallel registration of brain biorhythms [57].Systematic screening of volunteers showed the absence of mental and neurological diseases [58].A rating scale for hypnotic catalepsy was formed [59].
5. Clinical Hypnosis Scale
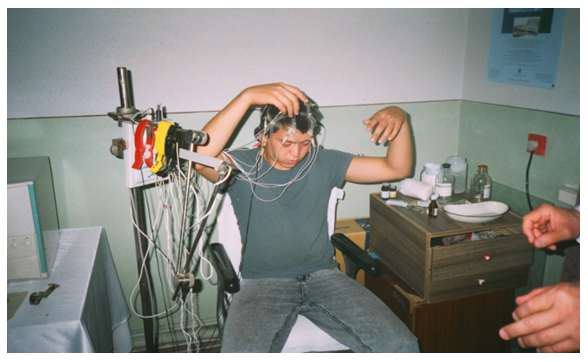
- Cataleptoid state (light - superficial trance). Drowsy state, drowsiness, general passivity. Blinking, closing the eyes (opening them can be arbitrary). Tremor of the eyelids. Delay in speech. Slight muscle weakness. Free movements are saved. Short-term catalepsy is possible. The hypnotized person hears, understands and analyzes «what is happening around». Comes out of hypnosis on his own. There is no amnesia. This condition is characteristic of low-hypnotic subjects.Cataleptiform state (medium hypnotic trance). The subject is asleep. Breathing is even, calm, deep, slow. The pulse is rare, rhythmic. Swallowing and blinking movements are absent. The facial muscles are relaxed. There is no muscle resistance. Loss of friendly and voluntary movement. Catalepsy is spontaneous or suggested. Eye catalepsy - the inability to open the eyes. The hypnotized person hears dimly, perceiving only harsh, strong sounds. Good repport. The hypnologist's words are learned and remembered. The subject cannot independently emerge from hypnosis. Amnesia is incomplete or absent. Average degree of hypnotizability.Somnambulistic state (deep hypnotic trance). Spontaneous persistent catalepsy occurs. The subject can walk without waking up and perform complex movements while standing and sitting with eyes open. The «cataleptic bridge» is reproduced. Complete amnesia. Anesthesia and analgesia - spontaneous or suggested. Sensory deprivation (lack of perception of external stimuli). Contact only with a hypnologist. Full repport. Complete submission. Suggestion of various dreams and illusions is possible. Induced hallucinations (positive and negative) can be olfactory, tactile, visual, acoustic and kinesthetic in nature. Implementation of post-hypnotic suggestions. Inherent in highly hypnotizable subjects.Lethargic type (a form of hypnosis not used for suggestion). Increasing muscle flaccidity. Severe hypodynamia (the raised hand falls «like a whip»). The body bends in an arc, the head «falls» on the chest. The hypnotized person may fall from the chair on which he is sitting. Pronounced weakness. Not able to make any movement. Rigid catalepsy (cogwheel phenomenon). General decrease in reflexes. Hypesthesia prior to analgesia. Partial amnesia (remembers «what is happening in hypnosis», not reacting in any way to «what is happening»). Difficulty in implementing post-hypnotic suggestions.We used the author's method of induction of «lightning» catalepsy with immobilization of the subject, acting on the kinesthetic system that maintains the balance of the body in space (multiple proprioceptors of joints, tendons and muscles, such as Golgi bodies, Pacini bodies, etc.).We taught the subject to abstract from the environment, focusing on the fulcrum, standing or sitting. Commands were given: "Relax, breathe deeply, close your eyes." We applied the sudden loss of balance by pulling the subject's wrists. To adapt it to external noises, we played the Charcot noise effect (clapping hands). The tactile test was carried out by designating the points of aesthesia on the subject, for the subsequent test of hypnotic anesthesia, while instilling a feeling of «wood» (stiffness). An analgesia test was performed after the subject had achieved sustained catalepsy by inserting a disposable needle into the forearm area (observing its response).Our method differs from existing methods of hypnosis in its high susceptibility to hypnotic suggestion of the subject and minimal use of verbal influence. The cataleptoid and cataleptiform states were also differentiated [60].The symptomatic picture of catalepsy was photographically documented.
 | Figure 1. Waxy body rigidity in hypnosis |
 | Figure 2. Somnambulistic state of hypnosis |
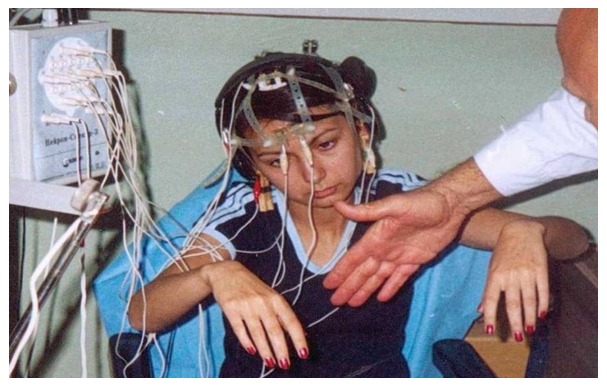 | Figure 3. The patient has not visual perception |
6. Discussion
- Our studies made it possible to differentiate hypnotic catalepsy as a physiological phenomenon from pathological catotonic stupor [68].Catalepsy can serve as a model for the deliberate limitation of the subject's chaotic voluntary movements with the ability to control this process. [69,70,71,72].In hypnosis, the emotional state and motor activity become regulated, which is confirmed by the corresponding changes in the delta- and theta-rhythms on the EEG. Low-frequency delta activity in the frontal leads of the left hemisphere may be associated with immobilization of the subject in hypnosis, and an increase in theta-rhythm in the temporal leads, with a positive emotional response to catalepsy. The paradoxical increase in the alpha-rhythm in the occipital leads of both hemispheres during the «open eyes» test indicates that the subject does not see the environment, i.e. he is in a state of hypnotic somnambulism [73,74,75,76,77].In hypnotic catalepsy, the visual, auditory, and kinesthetic sensory systems are blocked. This is tantamount to sensory deprivation, in which, without physical and chemical influence, suggestion changes the behavior model [78].Hypnotic catalepsy is accompanied by complex neurophysiological shifts in the relationship of certain brain structures. Low-frequencies in hypnosis can be associated with subcortical formations of the brain, such as the reticular formation and limbic systems, etc. [79,80,81].
7. Conclusions
- Hypnotic catalepsy in its psychophysiological basis is a state of kinesthetic deprivation, possibly allowing to stabilize the mental processes of the individual, while the subject more productively perceives psychotherapeutic suggestion.We have found that hypnotic techniques are effective and not associated with simulation. This is evidenced by objective EEG - parameters obtained in laboratory conditions.Experiments with volunteers in deep hypnosis showed that subjects without resistance followed the hypnologist's instructions with enthusiasm. It is important to emphasize that after the experiment, the subjects were emotionally satisfied.The data obtained suggest that with the help of hypnosis it is possible to restore the memory, volitional, emotional and behavioral processes of patients.Psychophysiological experiments with clinical hypnosis and the use of EEG may help to understand the biorhythmic interaction of the cortex and subcortical formations of the brain in the study of mental illness.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML