-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(3): 216-218
doi:10.5923/j.ajmms.20211103.11
Received: Feb. 23, 2021; Accepted: Mar. 15, 2021; Published: Mar. 28, 2021

Peculiarities of Platelet Aggregation Activity Indicators and von Willebrand Factor in Young Patients with Myocardial Infarction
Kamilova Umida, Pulatov Olimjon
Department of Therapy, Tashkent Medical Academy, Uzbekistan, Tashkent, Uzbekistan
Correspondence to: Kamilova Umida, Department of Therapy, Tashkent Medical Academy, Uzbekistan, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The features of platelet aggregation capacity and von Willebrand factor were studied in young patients with acute myocardial infarction (AMI). An increase in the parameters of platelet aggregation capacity and the level of von Willebrand factor (VWF) in blood plasma, which is more pronounced in young patients with acute MI, was found.
Keywords: Myocardial infarction, Young age, Platelet aggregation activity, Von Willebrand factor
Cite this paper: Kamilova Umida, Pulatov Olimjon, Peculiarities of Platelet Aggregation Activity Indicators and von Willebrand Factor in Young Patients with Myocardial Infarction, American Journal of Medicine and Medical Sciences, Vol. 11 No. 3, 2021, pp. 216-218. doi: 10.5923/j.ajmms.20211103.11.
Article Outline
1. Introduction
- Endothelial dysfunction plays an important role in the pathogenesis of cardiovascular diseases (CVD). Long-term experimental and clinical studies have shown that vascular homeostasis is largely due to the normal functioning of the vascular endothelium - a thin semi-permeable membrane that separates the systemic blood flow from the internal structure of the vascular wall [1,2]. All substances secreted by the endothelium and participating in hemostasis and thrombosis can, to a certain extent, conditionally be divided into two groups - thrombogenic and atrombogenic. Substances that initiate platelet adhesion and aggregation include von Willebrand factor, platelet activating factor, adenosine diphosphate (ADP), thromboxane A2 [3,4]. Under physiological conditions, the formation of atrombogenic substances in the endothelium prevails over the formation of thrombogenic ones, which ensures the preservation of the liquid state of the blood in case of damage to the vascular wall, including minor, accidental ones, which may occur normally. The secretion of atrombogenic substances determines the thromboresistance of blood vessels [5,6]. An important role in hemostasis is given to von Willebrand factor, a complex multimeric adhesive glycoprotein synthesized by endothelial cells and megakaryocytes. The most important function of this factor is that it is a carrier-stabilizer for the procoagulant protein FVIII: C, which circulates in the serum in the form of a non-covalently bound complex and is an adhesion protein during hemostasis [7,8].
2. Purpose of Work
- Study of indicators of platelet aggregation activity and VWF in young patients with myocardial infarction.
3. Material and Research Methods
- 74 patients with acute myocardial infarction (AMI) were examined. The study included male patients with primary Q-wave MI not more than 6 hours old from the onset of anginal pain. The diagnosis was established on the basis of the WHO criteria in the presence of the following signs: a characteristic attack of anginal pain or its equivalent lasting at least 30 minutes; the appearance of pathological Q or QS waves in two or more ECG leads. The patients were divided into 2 groups: The first group consisted of 38 AMI patients of young age - the average age is 44.28 ± 5.28 years and the second group consisted of 36 AMI patients over 60 years old - the average age is 65.48 ± 4.58 years. The control group consisted of 16 healthy volunteers. activity of platelet aggregation (APA) was determined by the method of G.V. Born. ADP was used as an inductor. The activity of platelet aggregation (APA), rate and maximum amplitude of aggregation were determined. The level of VWF was determined using a quantitative enzyme-linked immunosorbent assay using RPA «RENAM» (research and production association of the Russian society of patients with hemophilia) reagents. Statistical processing of the research results was carried out on a Pentium-IV personal computer using the Microsoft Office Excel-2012 software package, including the use of built-in statistical processing functions. Methods of variational parametric and nonparametric statistics were used with the calculation of the arithmetic mean of the studied indicator (M), standard deviation (σ), standard error of the mean (m), relative values (frequency,%), the statistical significance of the obtained measurements when comparing the mean values was determined by the criterion Student's t (t) with the calculation of the error probability (P) when checking the normal distribution (by the kurtosis criterion) and the equality of the general variances (Fisher's F-test.).
4. Research Results and Their Discussion
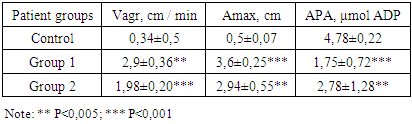
- The analysis of the obtained results showed that anterior myocardial infarction occurred in 43 (41.9%) patients, posterior wall infarction was observed in 31 (72.9%) patients. Arterial hypertension in anamnesis had 54 (72.9%), preinfarction angina in 38 (51.3%) patients.The study of platelet aggregation ability in patients with MI of both group 1 and group 2 showed that the initial indicators of activity of platelet aggregation (APA) were significantly higher than in healthy individuals, amounting to 1.75 ± 0.72 μmol ADP and 2.78 ± 1,28 μmol ADP versus 4.78 - 0.22 μmol ADP in healthy individuals (P <0.001) and P <0.005). In group 1 patients, the rate of platelet aggregation (Vagr) was also significantly high. In group I they were 2.9 ± 0.3.6 cm / min and in group 2 1.83±0.41 cm / min versus 0.34±0.5 cm / min in healthy individuals, respectively, P <0, 01. In patients with MI, the maximum aggregation amplitude (Amax) was also significantly higher than in healthy volunteers and was 3.6 ± 0.55 cm in group I, 2.94 ± 0.55 cm in group II versus 0.5±0.07 cm in healthy individuals, respectively (P <0.001) (table 1).
|
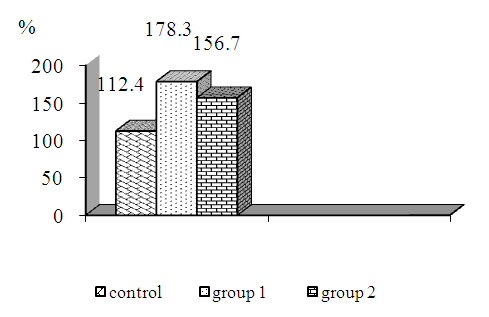 | Figure 1. Baseline values of EFV in AMI patients |
5. Conclusions
- Thus, in acute MI patients, there is an increase in the activity of platelet aggregation and the level of VWF in the blood plasma, which is more pronounced in young acute MI patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML