-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(3): 211-215
doi:10.5923/j.ajmms.20211103.10
Received: Feb. 19, 2021; Accepted: Mar. 17, 2021; Published: Mar. 28, 2021

Diagnostics of Precancerous Diseases of Oral Mucosa
Kamilov Kh. P., Kadirbaeva A. A., Aripova D. U.
Department of Hospital Therapeutic Stomatology, Tashkent State Dental Institute, Tashkent, Uzbekistan
Correspondence to: Kadirbaeva A. A., Department of Hospital Therapeutic Stomatology, Tashkent State Dental Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

With a variety of modern diagnostic methods, the issue of non-invasive early diagnostics of precancerous diseases is considered relevant. In the whole world, the fight against malignant neoplasms is considered an important problem not only in medicine, but also in society, since malignant neoplasms occupy the first place among the causes of death in the population of industrialized countries. Currently known techniques are stomatoscopy, photostomatoscopy, luminescence study when exposed to ultraviolet rays (Wood's rays), fluorescent diagnostics. The purpose of the study improved diagnosis of precancerous processes, as well as cancer of the oral mucosa, using minimally invasive examination methods. There were 50 patients with precancerous diseases of the oral mucosa at the age of 25-80 years examined on the base of the Department of Hospital Therapeutic Dentistry of the Tashkent State Dental Institute for 2017-2020. Methods of research were clinical, AFD, cytology. 16 people (31.3%) endogenous fluorescent glow different from the glow of healthy mucosa. Of these, 42 patients (84%) with erosive and ulcerative diseases of oral mucosa revealed fluorescence quenching, which rendered as dark areas with no visible glow. Early detection of potential precancerous processes allows avoiding interventional diagnostic methods, as well as reducing the risk of developing cancer of the oral mucosa.
Keywords: Precancerous diseases, Oral mucosa, Leukoplakia, Lichen planus, Autofluorescent stomatoscopy
Cite this paper: Kamilov Kh. P., Kadirbaeva A. A., Aripova D. U., Diagnostics of Precancerous Diseases of Oral Mucosa, American Journal of Medicine and Medical Sciences, Vol. 11 No. 3, 2021, pp. 211-215. doi: 10.5923/j.ajmms.20211103.10.
Article Outline
1. Relevance
- Analysis of the recent literature indicates that one of the common diseases of oral mucosa and the lip border are the diseases accompanied by hyper- and dyskeratosis, such as lichen planus, leukoplakia, various forms of cheilitis. As you know, these conditions belong to facultative precancers, with a malignancy rate of up to 19%. At the same time, abrasive precancerous cheilitis of Manganotti is referred to as obligate forms of precancer with high potential malignancy (from 9 to 42%). From a clinical and pathomorphological point of view, precancerous conditions include any chronic diseases accompanied by the formation of foci of excessive cell proliferation in the tissues, against which cancer can develop [1].The annual incidence of squamous cell carcinoma in the United States is approximately 40,000 cases, in Europe - 60,000 cases, in Russia - 60,000 [2]. The highest incidence of cancer of the oral mucosa is observed in India - 70%. In the Republic of Belarus, newly diagnosed cases of oral mucosa cancer were registered in 2006 - 717, and in 2007 - 707 patients, in 2008 - 735. Cancer of the oral mucosa ranks 6-9 in terms of prevalence among malignant tumors in the world [3-5].Primarily oncology alertness, diagnostic accuracy, clinical knowledge of diseases, the organization of oncological aid to the population, the strategy and tactics of this category of patients are required from dentists [6-8].In recent years, the method of autofluorescence diagnosis (AFD), based on differences in the intensity and spectral composition of autofluorescent radiation of normal and pathological tissue, has shown high sensitivity in detecting predictor changes and early forms of cancer of the mucous membranes of hollow organs [9-10]. The physical principle of the method is based on the excitation of intrinsic fluorescence (autofluorescence) of the mucous membrane by means of light from the blue zone of the optical spectrum (375-440 nm). It is known that autofluorescence of healthy tissues is observed in the green part of the spectrum in the range from 470 to 800 nm, the difference in wavelength between the excitation light (blue) and the emitted light makes it possible to detect fluorescence [11-12].According to clinical studies of recent years, a sharp decrease in the radiation intensity against the background of the surrounding healthy tissue is observed at the site of epithelial degeneration. This effect is called "dark spot", since the epithelium of precancerous and malignant formations emits a luminescence of lower intensity than the epithelium of the normal mucous membrane. The difference between the autofluorescence of neoplasms and normal epithelium is caused by changes in the physical structure of the tissue, changes in the volume of circulating blood, the content of fluorescent substances in the tissue [13-15].The question of the choice of methods for diagnosing early forms of cancer of the oral cavity and oropharynx remains open. An increase in morbidity, damage to people of working age, and a high percentage of relapses indicate numerous problems in the diagnosis and treatment of these diseases [16]. The presence of a large number of publications considering the histogenesis of precancerous lesions of the oral mucosa and lips introduces terminological confusion and creates problems in the classification of these pathological processes.Early diagnosis using screening methods for the active detection of precancerous diseases of the oral mucosa and early stages of asymptomatic cancer is relevant.
2. The Purpose of the Study
- The purpose of the study was to improve diagnostics of precancerous processes of oral mucosa cancer using minimally invasive methods of examination.
3. Materials and Methods
- On the base of the Department of Hospital Therapeutic Dentistry of the Tashkent State Dental Institute for 2017 -2020 years, 50 patients with precancerous diseases of oral mucosa at the age of 25 -80 years were examined. Among them, various forms of precancerous pathology of oral mucosa and lip red border were revealed: erosive and ulcerative form of lichen planus (LP) was in 27 patients (54%), erosive form of leukoplakia was in 12 patients (24%), verrucous leukoplakia was in 8 patients (16%); decubital ulcer was in 2 patients (4%), Manganotti cheilitis was in 1 patient (2%).All the patients included in research had the pathology of oral mucosa with the increased risk of malignancy development (such as smoking during 5-10 years, smoking NAS etc.)Examination of patients included traditional methods, such as interrogation, anamnesis, visual examination, palpation of regional lymph nodes, examination of the dentition, and also we carried out the autofluorescent stomatoscopy, determination of dispersed luminous particles (A-K method), PAP-test. The area of a single ulcer, erosion (Fig. 1) was calculated using the formula S = a×b, in the presence of several pathological elements, the total area of the affected surface was calculated using the formula S = S1 + S2 + S3 + n.
 | Figure 1. Patient K., 48 Diagnosis: lichen planus of the oral mucosa, erosive and ulcerative form. Visual inspection |
4. Results and Discussion
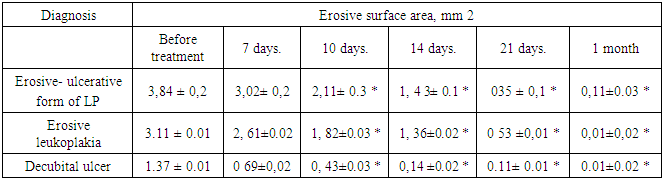
- Most of the examined patients complained of pain when eating, brushing teeth, permanent presence of erosions and mouth ulcers, impaired taste and sensitivity, increased or, conversely, decreased salivation. The beginning of the disease 3 5% of patients associated with unsuccessful prosthesis or with the removal of teeth, in other cases the trigger was a lot of stress. According to history it was found that 3 of 6% of patients previously treated for dental care, but the treatment did not bring the desired results. During the survey, it was found that when making a diagnosis, practitioners of other medical institutions in 97.9% performed only a visual examination16. Additional research methods, such as stomatoscopy, fluorescence diagnostics, have not been used previously. In 12 (12.5%) patients were previously examined for fungi of the genus Candida, morphological examination with a disease duration from several months to several years was carried out only in 2 (2.1%) patients.When analyzing concomitant pathology in patients with facultative precancerous lesions of organs and tissues of the oral cavity, the following results were obtained: diseases of the gastrointestinal tract occurred in 1 8 people (36%), diabetes mellitus in 1 person a (2%), blood diseases were in 2 people (4%). At the same time, 44 patients (8 9.3%) were found to have comorbid pathology, that is, a combination of two or more diseases of internal organs, most often of the cardiovascular and digestive systems.On an objective examination, 4 0 patients with dyskeratosis had partial loss of teeth, the mean values of the KPU index were 18.4 ± 0.02. Of these, 1 9 patients (38%) had low-quality orthopedic structures: 20 people had stamped-brazed stainless steel without spraying, 10 had the same sputtered structures, and 29 patients had metal - ceramic crowns and bridges. The revealed violations were eliminated by an orthopedic dentist and included removal of constructions, temporary and permanent prosthetics, as well as dynamic observation joint with the dentist m- therapist.Periodontal diseases such as chronic gingivitis and periodontitis are found in 100% of cases.As a result of the AFS study, one third of the applicants revealed a violation of the autofluorescence of the soft tissues of the oral cavity in the form of an increase or, conversely, a decrease in its intensity. So, 16 people (31.3%) endogenous fluorescent glow different from the glow of healthy mucosa. Of these, 42 patients (84%) with erosive and ulcerative diseases of oral mucosa revealed fluorescence quenching, which rendered as dark areas with no visible glow. In the foci of hyperkeratosis, on the contrary, an increase in fluorescence in the form of a bright white glow was noted. According to the results onco-screening in 3 patients showed inhomogeneous bright red or brown glow pathological elements subsequently have been verified morphologically squamous cancer of oral mucosa. At the stages of complex treatment, repeated AFS diagnostics and measurement of the area of pathological elements were carried out on days 7, 10, 14, 21, which made it possible to visualize the dynamics of epithelialization of pathological elements and evaluate the effectiveness of complex therapy (Table 1).
|
5. Conclusions
- The use of autofluorescent diagnostics at the primary admission in dentistry allows you to detect differences in the glow of healthy and pathologically altered tissue, and also it allows to improve visualization and to objectively determine the area of the affected surface. In addition, the "AFS-D" device can be recommended for evaluating the efficiency of treatment results and dynamic monitoring of patients with dyskeratosis of the oral mucosa. At the same time, the complex treatment of this category of patients should include sanitation of the oral cavity, elimination of traumatic factors, structures made of dissimilar metal alloys, optimal drug therapy and a rational approach to prosthodontic treatment.The express method for determining the DLP allows the detection of precancerous pathology of the oral mucosa without the use of expensive chemical dyes.Early detection of potential precancerous processes allows avoiding interventional diagnostic methods, as well as reducing the risk of developing cancer of the oral mucosa.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML