-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(3): 197-203
doi:10.5923/j.ajmms.20211103.08
Received: Feb. 2, 2021; Accepted: Mar. 1, 2021; Published: Mar. 15, 2021

Surgical Tactic with Development of New Algorithm for Selecting an Elimination Method of the Anterior Tracheal Wall Defects
R. Ya. Khayaliev, Sh. N. Khudaibergenov, O. D. Eshonkhodjaev, R. A. Ibadov
Republican Specialized Scientific and Practical Medical Centre of Surgery, Named after Acad. V.Vakhidov, Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Aim of the study was to improve the treatment results of patients with persistent defects of the anterior wall of the trachea and soft tissues of the neck. Material and methods. 220 patients with cicatricial tracheal stenosis were treated at the Republican Specialized Scientific and Practical Medical Center for Surgery named after academician V. Vakhidov. 120 of them had defects in the anterior tracheal wall of various sizes. There were 89(74,2%) males and 31(25,8%) females. The patients' age ranged from 6 to 70 years (mean age was 30.19 ± 1.21 years). All patients were performed mandatory endoscopic and MSCT examinations. The patients were performed surgical treatment after a planned examination. Results and discussion. The literature data on reconstructive-plastic methods for eliminating open tracheal defects were summarized and analyzed in the article. The advantages and disadvantages of various plastic materials for closing extensive tracheal defects were given. Unresolved issues in the treatment of persistent extensive defects of the anterior tracheal wall, problems of terminology and clear distribution of defects were indicated. The authors presented an original classification of fenestrated tracheal defects and their own algorithm for choosing a method of closing a defect depending on its parameters up to complete restoration of the airway patency. Conclusion. The choice of the method for plastic elimination of the tracheal defect depends on the size, depth of the airway lumen and the condition of the donor skin in the area of operation.
Keywords: Laryngotracheostomy, Persistent extensive defects, Trachea, Classification, Algorithm
Cite this paper: R. Ya. Khayaliev, Sh. N. Khudaibergenov, O. D. Eshonkhodjaev, R. A. Ibadov, Surgical Tactic with Development of New Algorithm for Selecting an Elimination Method of the Anterior Tracheal Wall Defects, American Journal of Medicine and Medical Sciences, Vol. 11 No. 3, 2021, pp. 197-203. doi: 10.5923/j.ajmms.20211103.08.
1. Introduction
- Despite the detailed methods of preventing of the airway walls injuries during prolonged mechanical ventilation, the number of patients with iatrogenic postresuscitation cicatricial tracheal stenosis (CTS) is not decreased. Moreover, there has been a tendency towards an increase in the proportion of patients with extended and multifocal lesions [1-3].A complex of endoscopic, surgical measures, as well as methods of reconstructive and plastic surgery are used in the treatment of patients with CTS. When patients with critical and decompensated forms of CTS are admitted, the first stage is endoscopic methods of expanding and maintaining of the tracheal lumen in the narrowing area. In the case of plastic surgery of the tracheal lumen on a T-shaped stent after prolonged exposure, the question of how to eliminate an open defect arises in the future.A great progress has been made in the treatment of patients with chronic tracheal stenosis recently. But the issues of plastic surgery and closure of the defect are still controversial and it is confirmed by the literature data analysis [4-7].Circular tracheal resection (CTR) belongs to the category of complex reconstructive interventions, requires the coordinated work of thoracic surgeons, endoscopists and anesthesiologists-resuscitators and should be performed in specialized clinics. Simultaneous resection of the trachea with an end-to-end anastomosis and elimination of the tracheal anterior wall defect from the cervical approach can be performed only in the absence of evident neurological deficit, a non-extensive defect of the trachea with the presence of tracheomalacia, which does not allow to perform musculocutaneous plasty with local tissues. Plasty of extensive defects of the trachea cervical part involves the restoration of not only the soft tissue defect, but also the mucous lining and frame function of the trachea and it requires a sufficient supply of complete, hairless skin in the reconstruction zone [8-9]. The absence of such areas near the tracheal defect (sharp dystrophic or cicatricial changes) requires the use of tissues with skin taken from other areas of the patient's body (the formation of the Filatov’s flap, the movement of fascial skin flaps on the vascular pedicle, autotransplantation of complex flaps on microvascular anastomoses) [10-11].A large number of possible tissues and materials, as well as options for surgeries aimed at eliminating the defect of the cervical trachea have been proposed. The basic requirements for them are clearly formed: they must be of sufficient size, provide a frame function and the ability to evacuate secretions and also be resistant to infection [1,5,7,12-14]. Despite this, the problem is relevant and continues to be the subject of research and discussion of thoracic surgeons, plastic surgeons and otolaryngologists. The choice of a method for eliminating a tracheal defect depends on its size, the depth of the airway lumen and the state of the tissues surrounding the defect [8,11,14-15]. Aim of the study was to improve the treatment results of patients with persistent defects of the anterior wall of the trachea and soft tissues of the neck.
2. Material and Methods
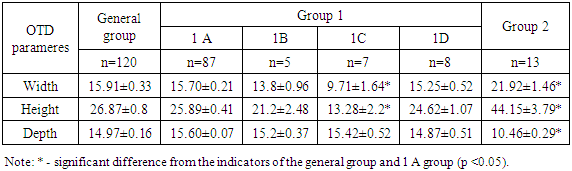
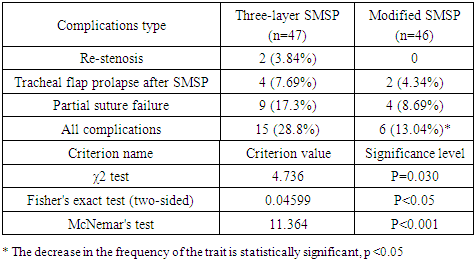
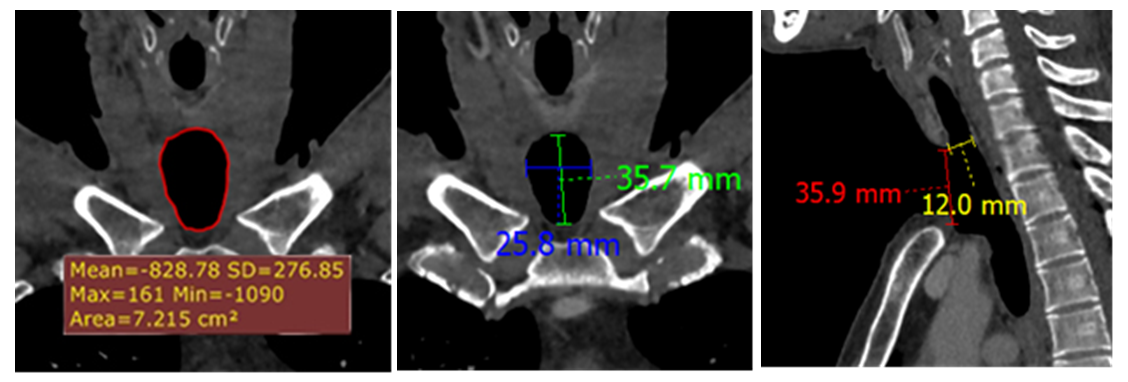
- 220 patients with cicatricial tracheal stenosis were treated at the Republican Specialized Scientific and Practical Medical Center for Surgery (RSSPMCS) named after academician V. Vakhidov from March 2008 to December 2020. 120 of them had defects in the anterior tracheal wall of various sizes. There were 89(74,2%) males and 31(25,8%) females. The patients' age ranged from 6 to 70 years (mean age was 30.19 ± 1.21 years). Goryainov D.A. (2014) referring to Grillo H.C., (2004) indicates that tracheal defects can be fenestrated and circular, small and large. Unfortunately, there are no other divisions of tracheal defects, especially the classification and clear definition of defects. In the absence of such, we took the liberty of developing our own working classification of tracheal defects.Classification of tracheal defects (RSSPMCS named after academician V. Vakhidov)I. By defect’s structureFenestrated tracheal defectsА - Small (up to 1.5 cm²)В - Large (from 1.5 cm² to 5.0 cm²)С - Extensive (over 5.0 cm²)II. By the duration of the defect persistence1. Persistent (are persisted after the tracheostomy removal for more than 2 months).2. Unstable (are closed independently after the tracheostomy removal within 2 months).III. By the appearence mechanism1. Post-traumatic2. Formed laryngotracheostomyIV. According to the condition of tracheal walls near the defect1) Morphologically restoration of multi-row epithelium with ciliated and goblet cells2) Tracheomalacia and overgrowth of coarse-fibrous connective tissue (chronic tracheocannulars)3) The presence of a tracheoesophageal fistulaV. By the height (depth) of the side walls of the defect1) Less 13 mm2) More 13 mm, but less 15 mm3) 15 mm and more All patients with an open tracheal defect (OTD) had tracheal stenosis of varying degrees before admission to the center. These patients had previously undergone plastic surgery of the tracheal lumen with the expansion of the stenotic area, removal of granulations and the installation of a T-shaped stent, commensurate with the location and length of the affected area. It should be noted that this is a difficult category of patients, each of whom has undergone a total of 3 to 11 operations. Before admission to our center 98 patients were performed tracheostomies. In 5 cases at intermediate stages of treatment, modified endotracheal tubes passed through the defect of the anterior tracheal wall, the so-called "clefts" were used. In 24 cases plastic surgery of the tracheal lumen was performed on a T-shaped stent, mainly by ENT doctors. 32 patients were referred from other hospitals of the country to close an existing OTD. 88 patients were hospitalized again for the final stage of a staged reconstructive plastic surgery (SRPS) - earlier in the Department of the lungs and mediastinum surgery they were performed stages of endoscopic coagulation, bougienage of tracheal stenosis followed by plastic surgery of the trachea with the formation of a lumen on the T-shaped stent. Therefore, when patients were admitted for OTD elimination they were of different sizes and depths. It was necessary to evaluate the parametric data of the defects of the anterior tracheal wall themselves to select the optimal tactics of surgical treatment for each specific patient. The high accuracy of measuring geometric relationships in comparison with bronchoscopy is an advantage of MSCT. MSCT allows to perform differential diagnostics between tracheomalacia and expiratory stenosis, external compression. It can be used as a criterion for the effectiveness of the surgical treatment of patients with tracheomalacia. The disadvantages of the method include radiation exposure, so its frequent repetition is not always justified. Three-dimensional models can be useful to improve the efficiency of X-ray diagnostic techniques and allow estimating the volume of surgical intervention when planning an operation (Fig. 1).
 | Figure 1. 3-D reconstruction of the tracheobronchial tree of a patient with OTD |
 | Figure 2. MSCT in frontal and lateral projections with measurement of the parameters of the OTD |
3. Results
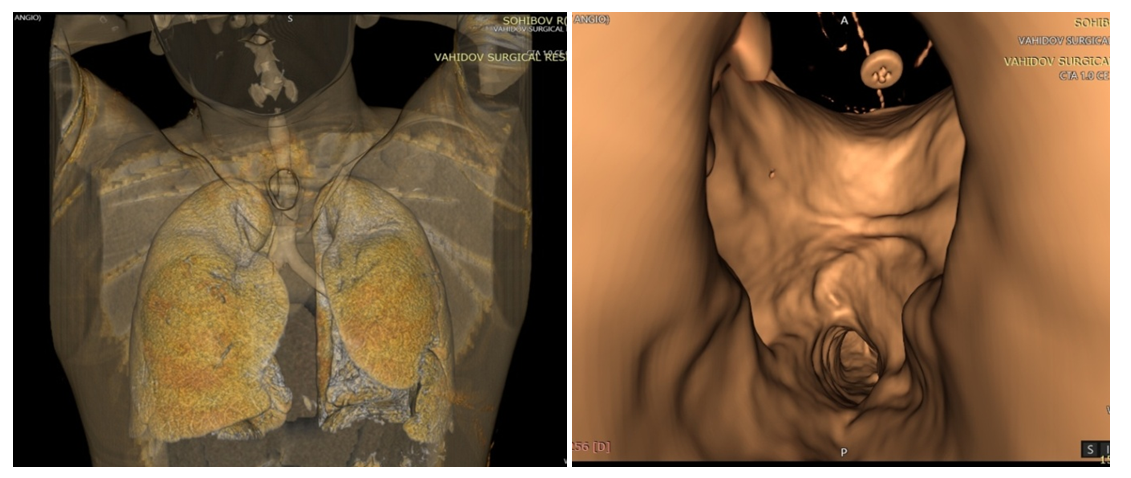
- Depending on the size and nature of the elimination of the anterior tracheal wall defect the patients were divided into two groups (Tab. 1).
|
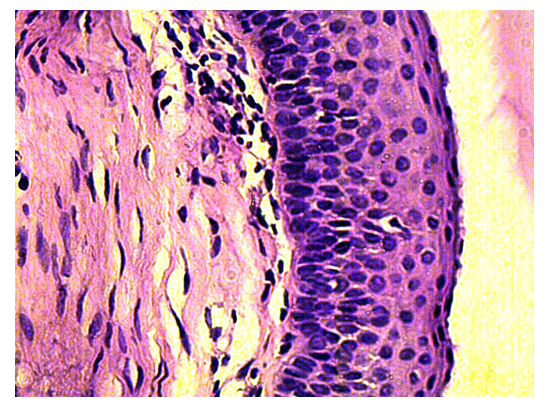 | Figure 3. Multi-row epithelial lining with accumulation of superficial prismatic cells, moderate perinuclear edema and mitotic figures in the basal parts. 7 months. OTD. G-E. 10х40 |
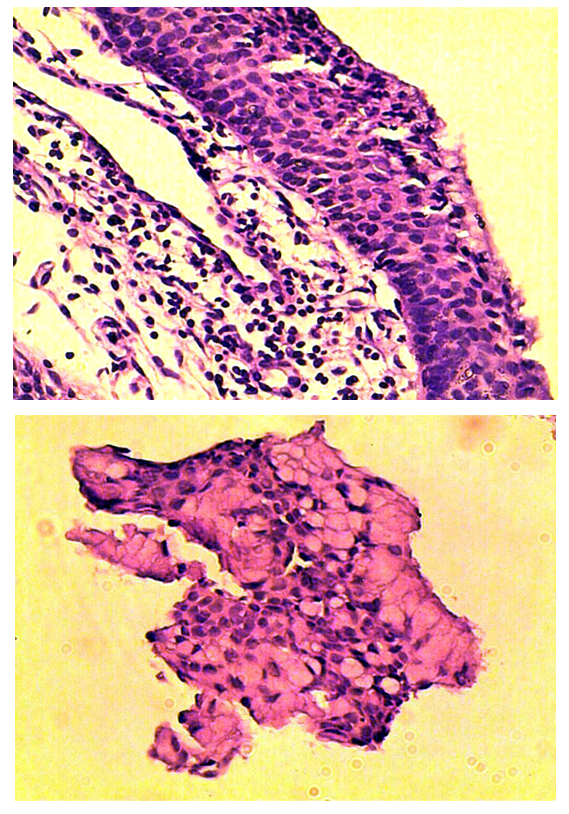 | Figure 4. A) The multi-row epithelial lining with an accumulation of superficial prismatic cells. 12 months. OTD. B) Goblet cells of the epithelial lining. 15 months. OTD. G-E. 10х40 |
4. Discussion
- We have developed our own algorithm for choosing a method for closing the defect depending on the size of the defect in the anterior tracheal wall. The application of this algorithm allows to use a differentiated choice of treatment tactics with the performance of a certain type of reconstructive plastic surgery for fully restoration of the airway patency. The choice of tracheal defect eliminating method depends on its size, the depth of the airway lumen and the state of the donor skin in the area of the defect. At small-sized defects skin-muscle-skin plasty (SMSP) according to Bokstein is performed in the modification of our clinics. CTR at OTD can be performed with limited stenosis without severe concomitant pathology, when there is tracheomalacia, restenosis, and the presence of a tracheo-esophageal fistula (TEF) in combination with cicatricial tracheal stenosis after ineffective attempts of elimination by endoscopic and surgical methods. A cartilaginous skin flap is used for large defect sizes which is prepared 1.5-2 months before the final operation. One of the main parameters in eliminating of a tracheal defect is the depth of the airway lumen - the distance from the anterior edge of the tracheostomy to the posterior wall of the trachea. When the depth of the lumen is less than 13 mm, the indications for plasty with autocostal cartilage are considered as a framework (Fig. 5).
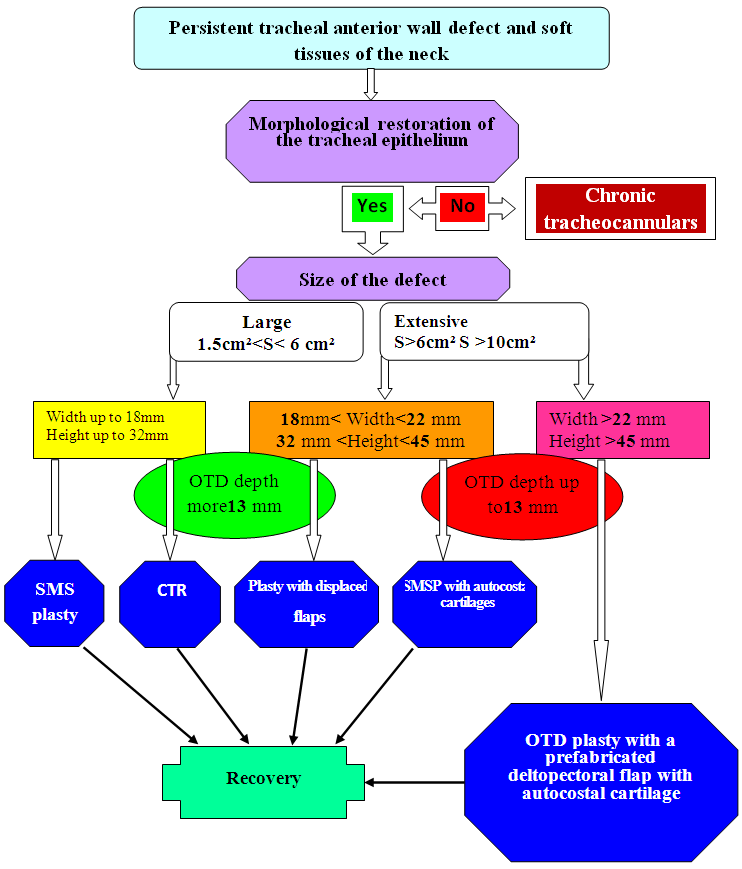 | Figure 5. Algorithm of choosing a method for closing a defect depending on the size of the OTD |
|
5. Conclusions
- When determining the strategy of eliminating defects of the trachea and soft tissues of the neck, there are no and cannot be absolutely established dogmas. In each specific case we have to choose one or another reconstruction option. Even fundamentally similar interventions in technical aspects can differ significantly from each other. The choice of the plastic elimination method of the tracheal defect depends on the size, depth of the airway lumen and the condition of the donor skin in the area of surgery. The timing of OTD elimination depends on the restoration of the stratified epithelium with highly specialized ciliated and goblet cells. If there is a significant proliferation of coarse-fibrous connective tissue in the tracheal walls adjacent to the defect, there is a high risk of restenosis during the first days after decannulation, which requires prolongation of T-shaped stenting.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML