-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(3): 175-181
doi:10.5923/j.ajmms.20211103.03
Received: Feb. 8, 2021; Accepted: Feb. 28, 2021; Published: Mar. 3, 2021

Comparative Analysis of the Short Term Results of Retroperitoneoscopic and Open Nephrectomies for Non-Oncological Kidney Diseases
Nazarov Dj. A., Mukhtarov Sh. T., Akilov F. A., Nasirov F. R., Ayubov B. A., Bakhadirkhanov M. M., Nuriddinov Kh. Z.
Republican Specialized Scientific-Practical Medical Center of Urology, Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

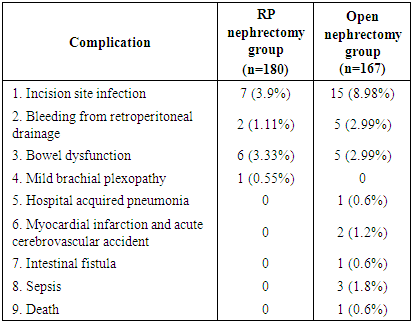
Background. With increasing acceptance of laparoscopic, retroperitoneoscopic and robotic procedures in urology over the last three decades, there is an ongoing discussion about the comparative outcomes of these procedures. Purpose: To report outcomes of retroperitoneoscopic nephrectomy (RPN) versus standard technique of open nephrectomy (ON) for various non oncological kidney diseases. Material and Methods: Clinical data of 347 patients who underwent nephrectomy from January 2019 to December 2019 were analyzed retrospectively. All patients were divided into 2 groups corresponding the surgical procedure. First group included 180 patients who underwent retroperitoneoscopic (RP) nephrectomy and second group consisted from 167 patients who underwent open nephrectomy. In both groups, the parameters of clinical outcome such as total blood loss, incision length, duration of surgical procedure, doses of nonsteroidal anti-inflammatory drugs used after surgery for pain relief and postoperative hospital stay are analyzed. We also assessed postoperative complications and classified. Results: The median amount of estimated blood loss was significantly lower (p < 0.001) in RP nephrectomy group 10 (10-400, IQR-40) mL in RPN group and 100 (25-400; IQR-100) mL in ON group). The median incision length was 60 mm (40-100 mm; IQR – 30) vs. 150 mm (100–230 mm: IQR – 30), and the median postoperative hospital stay was 2 days (1-12 days; IQR-1) vs. 5 days (2–14 days; IQR-2), and doses of analgesic medication requirement were 150 mg (0-375 mg; IQR-150) vs. 225 mg (0–1025 mg; IQR-225) for RPN and open nephrectomy respectively. The median operative time was 90 min (20-210 min; IQR - 45) for RPN and 80 min (60-180 min; IQR - 15) for ON, which didn’t significantly differ (p = 0.711). Complications. In ON group in 33 (19,76%) patients we observed postoperative complications. Among them 15 (8.98%) patients developed incision site infection, in 5 (2.99%) patients there was bleeding from retroperitoneal drainage, which required to increase in draining time. Postoperatively 5 (2.99%) patients had bowel dysfunction, in 1 (0.6%) patient developed hospital acquired pneumonia, in 2 (1.2%) patients - myocardial infarction and acute cerebrovascular accident, in 3 (1.8%) patients – sepsis, in 1 (0.6%) patient – intestinal fistula. 1 (0.6%) patient died due to sepsis syndrome and multiorganal failure. In RPN group in 16 (8.89%) we observed postoperative complications. Among them 7 (3.9%) patients developed incision site infection, in 2 (1.11%) patients there was bleeding from drainage, in 6 (3.33%) patients had bowel dysfunction. 1 (0.55%) patient developed mild brachial plexopathy, which treated by the administration of analgesia and muscle relaxers. Conclusions: Short-term results demonstrate that retroperitoneoscopic nephrectomy has the same success rates as open, - thoracolumbothomic approach, but morbidity and complication rate are significantly lover. These findings suggest that RPN has the potential to replace open surgery as the standard for treatment of majority of kidney cases.
Keywords: Retroperitoneoscopic, Nephrectomy, Morbidity
Cite this paper: Nazarov Dj. A., Mukhtarov Sh. T., Akilov F. A., Nasirov F. R., Ayubov B. A., Bakhadirkhanov M. M., Nuriddinov Kh. Z., Comparative Analysis of the Short Term Results of Retroperitoneoscopic and Open Nephrectomies for Non-Oncological Kidney Diseases, American Journal of Medicine and Medical Sciences, Vol. 11 No. 3, 2021, pp. 175-181. doi: 10.5923/j.ajmms.20211103.03.
1. Introduction
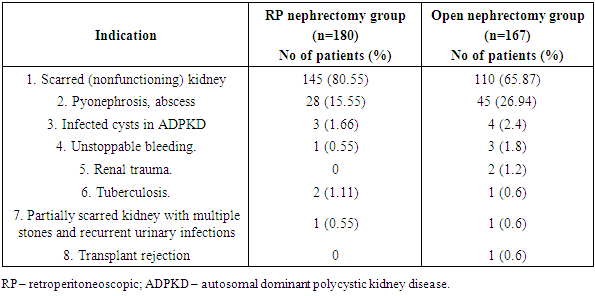
- The nephrectomy procedure was introduced to the practice of surgeons in XIX century. Based on this experience, the approaches, technical details, steps of the operation has been changed and modified and has become a standard all over the world for the treatment of different renal diseases [1,2].In 1990, Clayman et al. [3] performed the first laparoscopic nephrectomy and this method popularized worldwide. The technical difficulties of accessing the retroperitoneal space and the impossibility to create an effective and enough large pneumoretroperitoneum were overcome in 1992 by the introduction of the balloon dissection technique by Gaur [4]. This new approach then was modified and enabled the performance of different retroperitoneoscopic (RP) procedures [5,6]. But, despite the technical feasibility, current use of the retroperitoneal approach is not so much popular among urologists. In this study, we have comparatively evaluated our experience with the RP and with open nephrectomy (ON) performed in our clinic. These two groups have been balanced in terms of indications (table 1) and compared with respect to operative time, morbidity, blood loss, dose of analgesic use, postoperative mean visual analogue pain score (at third day) and postoperative hospital stay.
2. Material and Methods
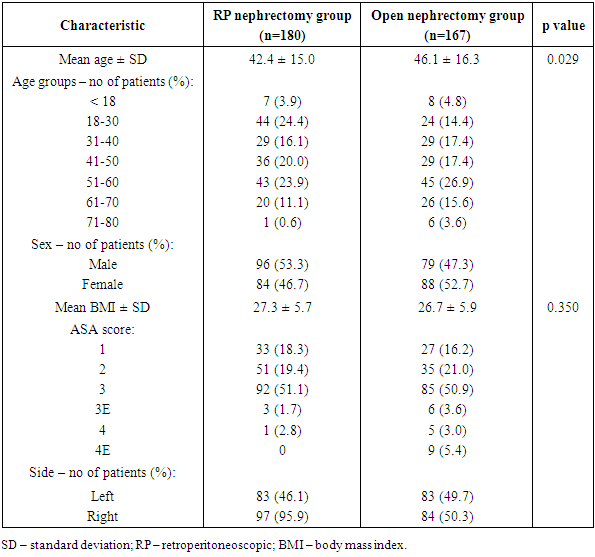
- Clinical data of 347 patients who underwent nephrectomy from January 2019 to December 2019 in Republican Specialized Scientific-practical Medical Center of Urology were analyzed retrospectively. The most common indication for both groups were scarred (nonfunctioning) kidney. Patient with suspected or confirmed malignancy were excluded from the analysis. Preoperative management included transabdominal ultrasound and urinalysis with culture, KUB film and intravenous urography or/and computed tomography (CT) urography, serum creatinine, complete blood count and basic metabolic panel. The American Society of Anesthesiologists (ASA) grading system was used to assess the patient’s physical condition and surgical risk. All patients were divided into 2 groups corresponding the surgical procedure. Patient selection was based upon referral, requesting either a laparoscopic or an open surgical approach, or depending on the previous surgical procedures and the complexity of the clinical case. First group included 180 patients who underwent retroperitoneoscopic (RP) nephrectomy and second group was control group and consisted from 167 patients who underwent open nephrectomy for various etiology kidney diseases. Basic characteristics of patients are shown in table 1.
|
|
3. Results
- The median amount of estimated blood loss was 10 (10-400, IQR-40) mL for RP nephrectomy group and 100 (25-400; IQR-100) mL for ON group, which reliably shows that RP nephrectomy is accompanied by less blood loss (p < 0.001).
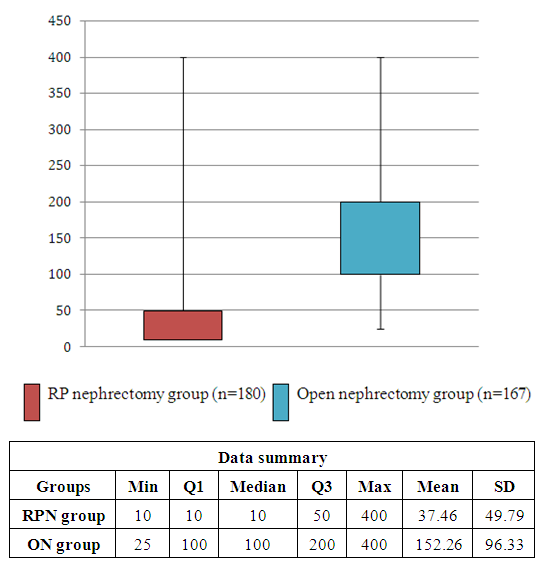 | Figure 1. Box plot chart for comparison of intraoperative blood loss in both groups in mL (p < 0.001). Note: outliers in this graph are not shown |
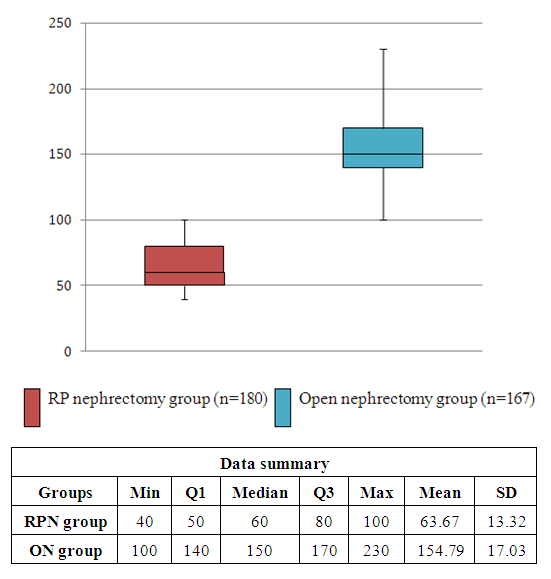 | Figure 2. Box plot chart for comparison of incision length in both groups in mm (p < 0.001) |
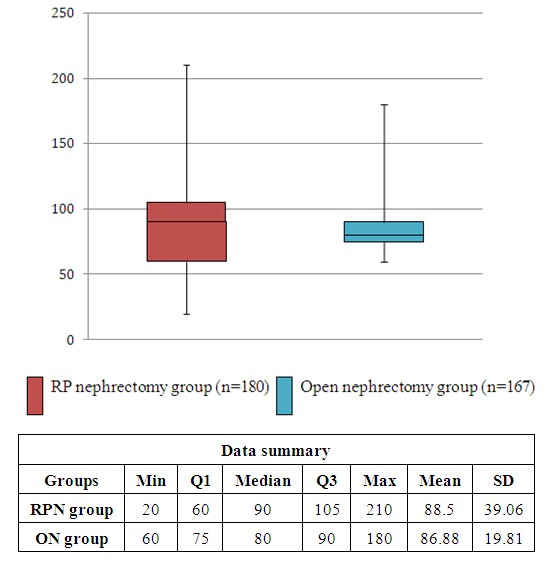 | Figure 3. Box plot chart for comparison of operative time in both groups in min (p = 0.711) |
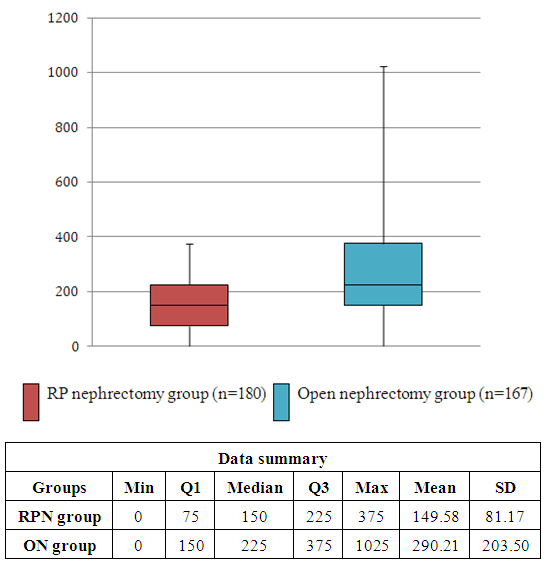 | Figure 4. Box plot chart for comparison of diclofenac doses for postoperative pain relief in both groups in mg (p < 0.001) |
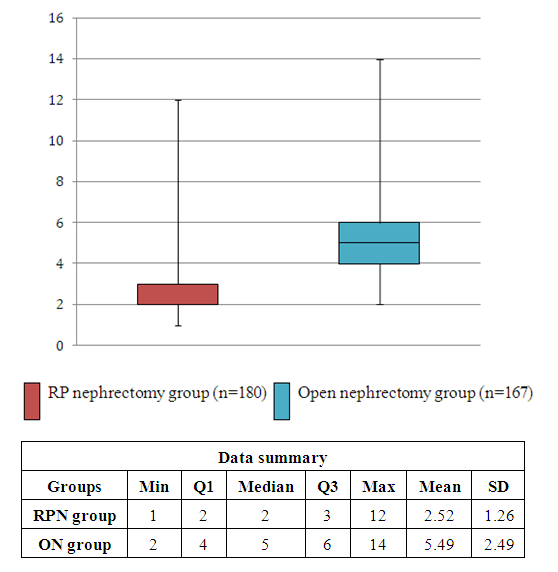 | Figure 5. Box plot chart for comparison of postoperative hospital stay time in both groups in days (p < 0.001) |
|
|
4. Discussion
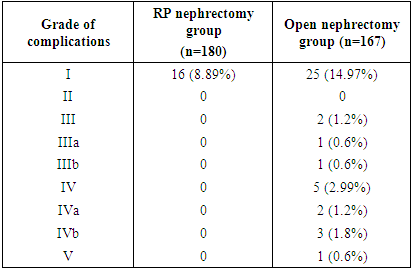
- Minimally invasive methods of simple or radical nephrectomy (laparoscopic, retroperitoneoscopic) are replacing the conventional open nephrectomy. The revealed benefits of retroperitoneoscopic approach are patient comfort, improved cosmetic result and shorter convalescence [8]. As originally described by Clayman et al. [3], the technique of laparoscopic nephrectomy included several steps: re-positioning of the patient from the supine to the lateral decubitus position after obtaining a pneumoperitoneum. Furthermore, dissection of the colon, which is performed in order to gain access to the retroperitoneum, could be the risky of injury to the liver or spleen. These disadvantages supported the search for standardizing a retroperitoneal approach which – as being similar to the open access [1] – could hopefully overcome these problems.In 1992, Gaur [4] introduced his revolutionized technique based on the insufflation of a special balloon catheter which allowed properly dissect the retroperitoneum and he has reported his experience with the first retroperitoneal laparoscopic nephrectomy [12]. In 1994, Rassweiler JJ et al. described their similar balloon dissection technique based on a hydraulic mechanism [13,14].There are some absolute contraindications for the transperitoneal laparoscopic approach, like a history of or active peritonitis, markedly distended bowel, extensive adhesions from prior surgery, uncorrected coagulopathy and hypovolemic shock [13,15,16]. However, in the case of retroperitoneal procedures, previous open abdominal surgery or history of peritonitis are not necessarily regarded as contraindications. But, severe perinephric adhesions due to previous lumbotomies, paranephritis, xanthogranulomatous pyelonephritis, renal tuberculosis, post-traumatic renal atrophy or post-embolization nephrectomies may make retroperitoneoscopic approach mostly impossible [14].It has noted that even among healthy patients for the open donor nephrectomy a 3.5% major complication rate and up to 30% minor complication rate were described. The operative time, although brief (90–140 min), is followed by a long hospital stay of 6.4–10.5 days [17,18]. Blohme et al. [19] have reported their series of 490 living open donor nephrectomies with a major complication rate of 1.4% and a minor complication rate of 13.6%. Often the major criticism towards laparoscopic approach has focused on the complications that were supposed to be more frequent than in open nephrectomy. Kavoussi et al. [16] classified the possible complications into needle and trocar injuries, insufflation, dissection and closure injuries, and Gill et al. [15] presented the USA experience and complications rate for laparoscopic nephrectomy. Vascular injuries were the most common lesions and occurred during dissection of the renal hilum or accessory vessels. Complications according to insufflation can lead to cardiopulmonary problems, hypercarbia with associated acidosis and eventually pulmonary gas embolism. Postoperative incisional hernias have been described in trocar sites larger than 10 mm [20,21].The complications of surgery can be uniformly compared according to the modified classification described Clavien-Dindo [7] (Table 2). We also have found similar overall complication rates for each group (Table 3). It is also notable that the majority of complications in both groups was minor and was similar with other series of open or RPN [15-19,22,23].
5. Conclusions
- Currently in the last 10 years, there have been performed more than 1200 cases of retroperitoneoscopic nephrectomies. Based on the results of our study we conclude that RPN should be currently recognized as the method of choice for most kidney diseases requiring nephrectomy. The main “disadvantage” in terms of operation time can be widely compensated by the advantages of less analgesia, reduced hospital stay and cosmetic advantages. The cosmetic appearance and shorter convalescence after such procedures is more attractive to the patient who is quite satisfied with the overall result. In our experience the durability of operating time mainly depended on learning curve, the individual pathology, i.e. size of the kidney, number of renal arteries, and peri-renal adhesions.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML