-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(3): 170-174
doi:10.5923/j.ajmms.20211103.02
Received: Feb. 5, 2021; Accepted: Feb. 28, 2021; Published: Mar. 3, 2021

Clinical and Laboratory Features of Coronary Heart Disease in Patients with Aspirin Resistance
Khodjanova Shakhnoza Iskandarovna, Alyavi Anis Lutfullayevich
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

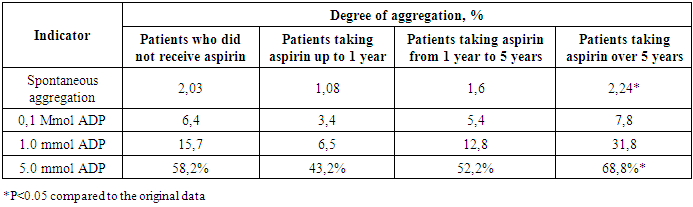
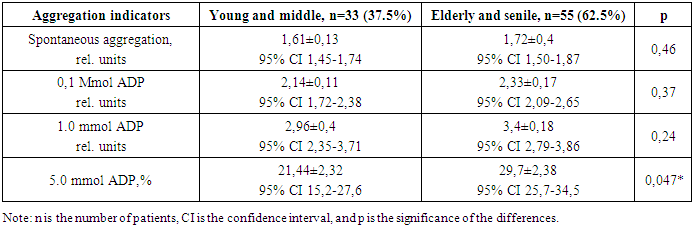
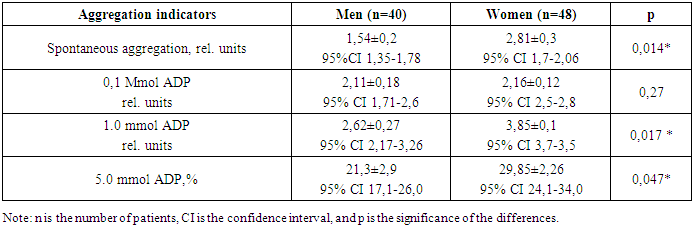
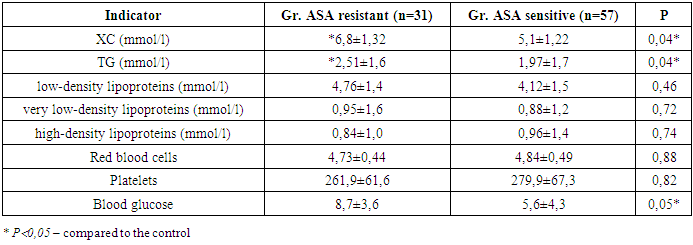
Purpose. To determine the frequency of aspirin resistance in patients with coronary heart disease and evaluate the risk factors for the developement aspirin resistence in patients with coronary heart disease. Material and methods. 88 patients were enrolled in the study with stable forms of coronary heart disease, who received a standard dose of aspirin 75 mg/day for a long time. Platelet aggregation was measured using a laser analyzer, and adenosine diphosphate was used as an inducer. All statistical analysis were performed SPSS software. Results. 35.2% of patients who took aspirin at a standard dose of 75 mg / day were resistant to aspirin. The average degree of platelet aggregation with 5.0 mmol of ADP was 79.4% in patients with resistant to aspirin. Patients with aspirin resistance were significantly more likely to have a history of myocardial infarction than aspirin-sensitive individuals. There were a correlation between lipid disorders and the functional state of platelets. The most significant negative correlation of the platelet aggregation index was determined in relation to the level of cholesterol (r = -0.41) and triglycerides (r = -0.43). Possible risk factors for the development of ASA resistance were: female gender, old age, obesity, hypercholesterolemia and hyperglycemia, since patients with aspirin resistance tended to have higher cholesterol and glucose levels (p<0.05). Conclusion. Aspirin resistance was more common in patients with coronary heart disease taking aspirin over 5 years, the elderly and in women. Possible risk factors for developing ASA resistance are old age, female gender, obesity, and hypercholesterolemia.
Keywords: Aspirin, Aspirin resistance, Coronary heart disease, Platelet aggregation
Cite this paper: Khodjanova Shakhnoza Iskandarovna, Alyavi Anis Lutfullayevich, Clinical and Laboratory Features of Coronary Heart Disease in Patients with Aspirin Resistance, American Journal of Medicine and Medical Sciences, Vol. 11 No. 3, 2021, pp. 170-174. doi: 10.5923/j.ajmms.20211103.02.
1. Introduction
- Currently, it is proved that the appointment of antiplatelet drugs for the primary and secondary prevention of acute cardiovascular events is a mandatory component of the pharmacotherapy of CHD and is included in the clinical recommendations of different levels [2,6,7,9]. Acetylsalicylic acid (aspirin) is considered to be the only disaggregate whose clinical efficacy has been proven by numerous clinical studies [7,8,9].In recent years, it has been noted that in a number of patients, aspirin has less pronounced antiplatelet activity. This phenomenon is known as aspirin resistance. According to different authors, the frequency of determining aspirin resistance varies significantly – from 5.2% to 57% [1]. These patients appear to have a poorer prognosis than patients with clear, ASA-dependent inhibition of platelet function [3]. An analysis conducted in Cleveland clinic's revealed a correlation between aspirin resistance and clinical outcomes, and also revealed that patients with aspirin resistance, which was studied using an express platelet functional state analyzer, are more than three times more likely to develop ischemic complications in the future (death, stroke or myocardial infarction) [5].Resistance to aspirin is defined as: the inability of aspirin to protect the patient from thrombotic complications; to prolong the bleeding time; to suppress the biosynthesis of THA2; to suppress platelet function in one or more in vitro tests. The problem of resistance to antiplatelet drugs is fundamental in its significance, since it creates prerequisites for the individualization of preventive therapy and the formation of more effective methods for preventing the disease. [4].The prevalence of aspirin resistance and its clinical significance are poorly understood. Patients with chronic coronary heart disease take aspirin for years, but do not know the effectiveness of this drug, and it is not always possible to determine the effectiveness of antiplatelet agents using laboratory tests.The purpose of this study was to study the prevalence of aspirin resistance and the factors influencing aspirin resistance in patients with coronary heart disease who take aspirin for a long time.
2. Materials and Methods
- The study included 88 patients aged > 18 years with a diagnosis of CHD stable angina pectoris (SAP) of functional classes II-III (FC). The patients were treated in the cardiology department of the Republican Specialized Scientific and Practical Medical Center for Therapy and Medical Rehabilitation. The diagnosis of CHD in the form of a clinical form of SAP II-III FC, established according to European recommendations [2].All patients received standard therapy: antithrombotic, antihypertensive, antianginal drugs, statins. As an antiplatelet agent, ASA (tablets coated with an intestinal-soluble coating) was prescribed at a dose of 75 mg. All patients underwent physical examination, clinical and laboratory methods of investigation (general blood analysis, biochemical blood analysis, blood lipid spectrum and coagulogram), platelet aggregation and functional diagnostics (ECG, EchoCG).The study of platelet aggregation in platelet-rich citrate plasma by the Born and O'Brien method was performed on a two-channel laser analyzer of platelet aggregation Alat-2 Biol, with computer processing according to the AGGR program. Solutions of adenosine diphosphate (ADP) with final concentrations of 0.1, 1.0, and 5 µg/ml were used as aggregation inducers. The normal limits of the activity of the platelet aggregation process with the addition of 5.0 mmol of ADP are 25-72%. Statistical processing of the study data was carried out using the SPSS 18.0 software.
3. Results
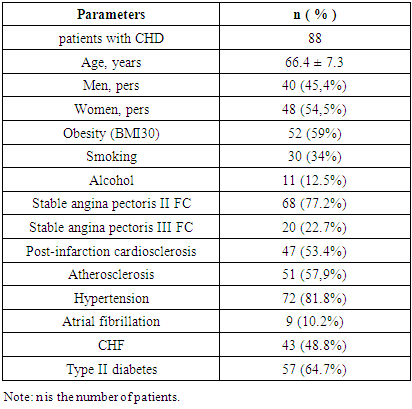
- The study included 88 patients (40 men and 48 women), the average age was 66.4 (45.3—78.4) years. Table 1 shows the characteristics of patients with CHD.
|
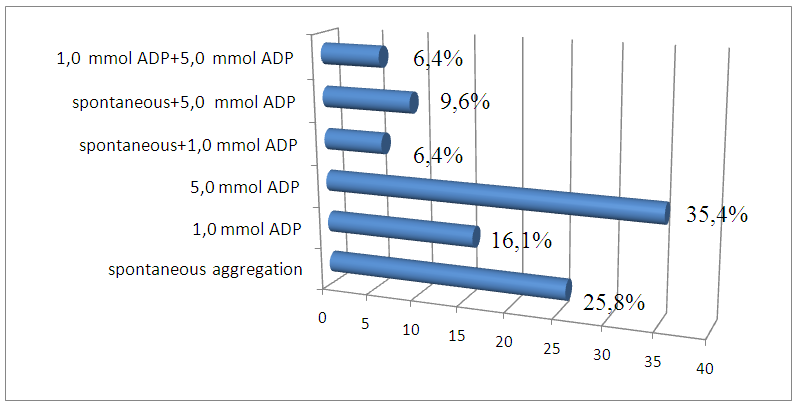 | Figure 1. Distribution of the increased aggregation response depending on the concentration of the inducer in patients with CHD receiving ASA preparations |
|
|
|
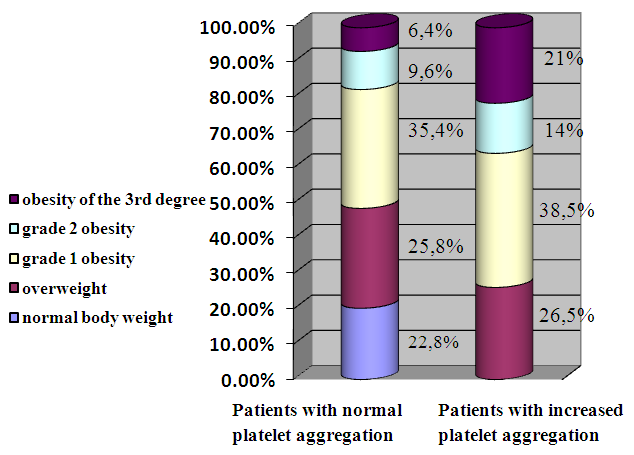 | Figure 2. Distribution of patients with normal and increased platelet aggregation depending on body weight |
|
4. Conclusions
- 1. Aggregation aspirin resistance was observed in 1/3 of patients with ischemic heart disease who took aspirin for a long time.2. Patients with ASA resistance were significantly more likely to have a history of myocardial infarction than aspirin-sensitive individuals.3. Possible risk factors for the development of resistance to ASA are: old age, female gender, obesity and hypercholesterolemia.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML