-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(2): 106-112
doi:10.5923/j.ajmms.20211102.08
Received: Jan. 17, 2021; Accepted: Feb. 1, 2021; Published: Feb. 6, 2021

Dynamics of Cytological Parameters During the Treatment of Long-Term Non-Healing Soft Tissue Wounds
B. R. Abdullajanov, K. A. Yusupov, A. Kh. Babadjanov, R. A. Sadykov, J. K. Yusupov
Andijan State Medical Institute, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Aim of the research is to study the dynamics of cytological parameters in the treatment of chronic non-healing purulent wounds of soft tissues. Material and methods. The study was based on the treatment results of 132 patients with chronic non-healing purulent wounds of soft tissues who were treated in the clinic of the Andijan State Medical Institute from 2016 to 2020. Retro- and prospective studies were carried out with the distribution of patients into 3 groups. 54 patients with traditional treatment (retrospective analysis) were included in Comparison group № 1. Comparison group №. 2 was consisted of 40 patients whose treatment was carried out only with the use of the FarGALS drug. The main group included 38 patients, whose treatment was carried out according to the proposed method of chemo-photodynamic therapy with local use of the FarGALS domestic drug and laser irradiation of the wound. The results of cytological samples of exudate isolated from wounds were analyzed in a comparative aspect. The reliability of the results obtained is testified by statistical methods. Results. Analysis of the cytograms types from wounds in the dynamics of treatment showed that in the main group of patients, the acceleration of the transition of the inflammatory phase to the regenerative phase was noted by the 14th day in 71.1% of patients (versus 31.5% in group № 1, χ2 = 17.073; df = 3; p <0.001 and 47.5% in group № 2), and on 21st day in 94.7% of patients (versus 53.7% in group № 1, χ2 = 18.188; df = 2; p <0.001 and 77.5% in group № 2, χ2 = 4.780; df = 1; p = 0.029). Conclusion. The introduction of a new method of combined local chemo-photodynamic therapy of long-term non-healing purulent wounds of soft tissues, aimed at the induction of anti-inflammatory and reparative action, allowed to accelerate the transition of the inflammatory phase to the regenerative phase in a relatively short period of treatment.
Keywords: Surgery, Long-term non-healing purulent wound of soft tissues, Method of chemo-photodynamic therapy, Dynamics of cytological parameters
Cite this paper: B. R. Abdullajanov, K. A. Yusupov, A. Kh. Babadjanov, R. A. Sadykov, J. K. Yusupov, Dynamics of Cytological Parameters During the Treatment of Long-Term Non-Healing Soft Tissue Wounds, American Journal of Medicine and Medical Sciences, Vol. 11 No. 2, 2021, pp. 106-112. doi: 10.5923/j.ajmms.20211102.08.
1. Introduction
- The issues of improving the tactical and technical aspects of the treatment of chronic non-healing purulent wounds (CNPW) of soft tissues are one of the topical, actively discussed in the literature and still unsolved problems of surgery. [1-3]. In this aspect, the most pressing issues are the development of new dressings, wound healing chemical agents and tactical approaches to their combined use with physical factors designed to enhance the activity of cleaning and epithelialization of the wound surface, accelerate the time of complete regeneration with restoration of anatomical and functional structures and reduce the risk of early relapse [2-3]. According to the Global Burden of Disease Study (2016), "the morbidity of the skin diseases and subcutaneous tissue of various etiologies is 8.24%, while the prevalence of chronic non-healing purulent wounds (CNPW) in soft tissues is 2.21 per 1000 population." [2,4]. At the same time, "the frequency of purulent-necrotic inflammation reaches 45% of the total number of surgical skin wounds, leading to disability and mortality up to 25% -50%" [5-7]. Soft tissue CNPW is known to lead to chronic pain, loss of activity, increased stress and social isolation, depression and anxiety, prolonged hospitalization, and significant increases in treatment costs [8-10]. Also, as a result of the active development of surgical technologies, the first place is the problem of safety and biocompatibility of the currently used dressings, local drugs and methods of physiotherapy, reduction of the rehabilitation period, the frequency of infectious complications and the achievement of accelerated wound healing [3,7,9]. Thus, the lack of unity of views and debate on some issues of treatment tactics for this difficult contingent of patients dictates the need for a more detailed study of this problem. Special attention is required to continue studying the issues of clinical application of various options for combined chemical and physiotherapeutic effects and their optimization. These circumstances have stipulated the growing interest in photodynamic therapy (PDT), as a serious alternative to the traditional standard approaches to surgical treatment of wounds, medical methods of debridement and dressings.Aim of the research is to study the dynamics of cytological parameters in the treatment of long-term non-healing purulent wounds of soft tissues.
2. Material and Methods
- The study was based on the treatment results of 132 patients with chronic non-healing purulent wounds of soft tissues who were treated in the clinic of the Andijan State Medical Institute from 2016 to 2020. In all patients, purulent wounds were formed at least 14 days before admission, and the average duration of the presence of a wound was 22.6 ± 1.9 days. The study included only those patients whose LNPW treatment implied only local exposure; patients with wounds of soft or deep-lying tissues were excluded, for whom various methods of surgical treatment were performed (traditional and minimally invasive interventions on vessels, amputations, etc.). All patients were divided into three groups according to the CNPW treatment method. Two comparison groups were formed. Comparison group № 1 was consisted of 54 patients in whom the analysis of the results for the comparative study was carried out retrospectively. A prerequisite for inclusion in this group was the correspondence of the clinical course of CNPW, as well as other indicators (age, sex, comorbidity, causes of wound formation, etc.) to patients in other groups, as well as the availability of all the necessary data for comparative analysis. CNPW treatment in this group was carried out according to the traditional method. The main group included 38 patients who were treated according to the proposed method. The domestic drug "FarGALS" was used as an antiseptic and wound-healing agent, as well as a photosensitizer for PDT. We used the “Matrix” laser device as a source of radiation for PDT. A semiconductor emitter with a radiation power of 3 mW, spectrum - 337 nm was used in it. Radiation is pulsed with a frequency of 100 Hz. The device is equipped with a light guide with a diameter of 500 µm, a power meter and a timer with discrete time values from 10 sec to 3 min.The absorption spectrum of "FarGALS" completely coincides with the radiation of the laser apparatus "Matrix". The domestic highly effective antimicrobial drug showed an absorption spectrum in the 350-550 nm mode, with a second slight rise of the curve in the 800 nm spectrum.Comparison group № 2 included 40 patients. In this group the treatment of patients was carried out only with the use of the drug "FarGALS" for an objective picture in evaluation of the results. The age of the patients included in the study ranged from 25 to 75 years. Most of the patients corresponded to the age group from 45 to 60 years. There were 25 (46.3%) females and 29 (53.7%) males in comparison group № 1. There were 19 (47.5%) females and 21 (52.5%) males in comparison group № 2. There were 20 (52.6%) females and 18 (47.4%) males in the main group. According to the classification of surgical soft tissue infections proposed by Ahrenholz D.H. in 1991, all patients included in the study were assigned to the second level with lesions of the subcutaneous tissue (abscess, phlegmon, etc.) and to the third level with lesions of the superficial fascia (necrotizing fasciitis). The distribution of patients according to the recommendations of the Russian Association of Specialists in Surgical Infections showed that all cases were attributed to secondary infections with a complicated course, the causes of which were: bites with an outcome in infected wounds, infection of the surgical site, infected trophic ulcers, bedsores and infected burn wounds.According to the localization of wounds, the patients were distributed as follows: wounds of the medial malleolus made up the majority of cases both in the main (44.7%) and in comparison groups № 1 and № 2 (48.1% and 45.0%). Next in frequency of occurrence were wounds of the soft tissues of the lower leg, sacrum region, buttocks, feet and forearm.According to the presence of combined pathology in patients, there were no significant differences between the main and comparison groups № 1 and № 2. Most often, both in the main (34.2%; 13 from 38 patients) and in comparison groups № 1 (27.8%; 15 from 54) and № 2 (27.5%; 11 from 40) arterial hypertension was observed. Concomitant pathology of the gastrointestinal tract was observed in 4 (10.5%) patients in the main group, in 5 (9.3%) cases of comparison group № 1 and in 5 (12.5%) patients of group № 2. The diagnosis of concomitant diabetes mellitus was defined with a frequency of 10.5% (4 from 38), 5.6% (3 from 54) and 7.5% (3 from 40) in the main and comparison groups № 1 and № 2, respectively. Various forms of coronary heart disease as a concomitant pathology were detected in 13.2%, 11.1% and 10.0% of cases in the main and comparison groups № 1 and №2, respectively. Concomitant pathologies of the kidneys and lungs were detected with a relatively lower frequency.In patients of the study groups after primary surgical treatment wounds with an area from 401 to 600 mm2 were most often observed: 48.1% in comparison group № 1, 50% in group № 2 and 55.3% in the main group. According to the frequency of detection, wounds with an area of 201-400 mm2 were noted in 28.9%, 37.0% and 35.0% cases of the main, comparison groups № 1 and № 2, respectively. Extensive wounds with an area of more than 600 mm2 were detected in only 4 (10.5%) patients of the main group, in 6 (11.1%) cases of group № 1 and in 4 (10%) patients of comparison group № 2.
3. Results
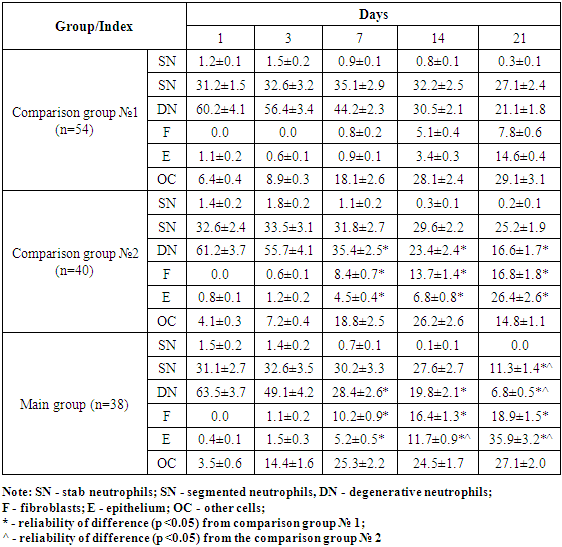
- Degenerative neutrophils predominated in the wounds of patients of all three groups, fibroblasts and epithelial cells were practically absent at the initial stage of treatment. In dynamics, we could observe a gradual improvement of the inflammatory process in wounds. So, the number of degenerative neutrophils (per 100 cells) by the 21st day of treatment decreased from 63.5 ± 3.7 to 6.8 ± 0.5 in the main group of patients; from 60.2 ± 4.1 to 21.1 ± 1.8 - in comparison group № 1 and from 61.2 ± 3.7 to 16.6 ± 1.7 in group № 2. At the same time, there was a significant difference in this indicator in favor of the main group of patients (p <0.05). A gradual increase in the number of fibroblasts was cytologically revealed (in the main - up to 18.9 ± 1.5; in group № 1 - up to 7.8 ± 0.6; in group № 2 - up to 16.8 ± 1.8) and epithelial cells (in the main - up to 35.9 ± 3.2; in group № 1 - up to 14.6 ± 0.4; in group №2 - up to 26.4 ± 2.6) in a wound with a significant difference (p <0. 05) from comparison group №1 (Tab. 1).
|
|
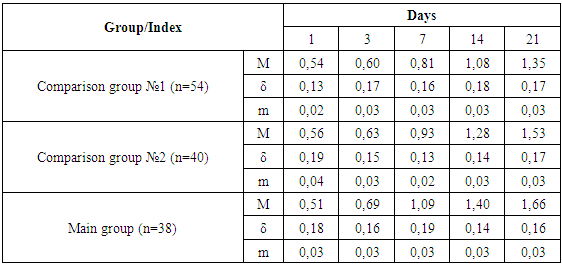
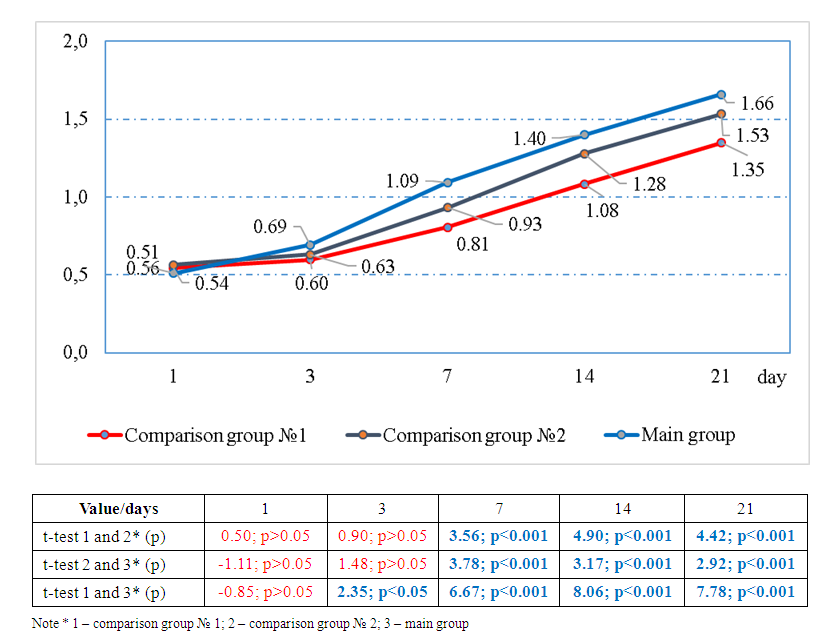 | Figure 1. The dynamics of the growth rate of the regenerative-degenerative index during treatment |
|
4. Discussion
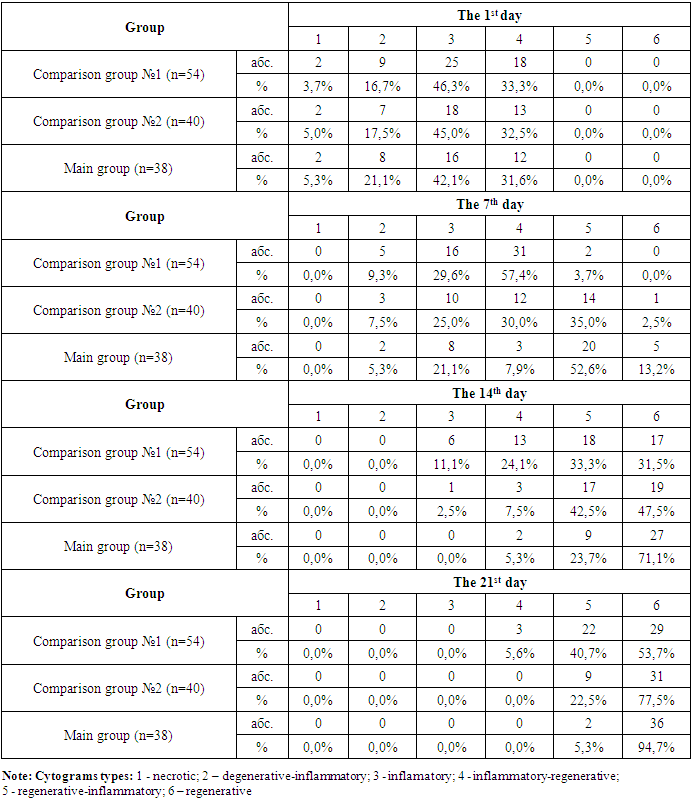
- In the course of treatment we studied and monitored the ratio of cytograms types in the investigated groups (Table 3 and Fig. 2). Thus, at the initial stage of treatment, the following types of cytograms were identified in all groups: necrotic, degenerative-inflammatory, inflammatory and inflammatory-regenerative. The highest frequency of occurrence was found in the inflammatory type - 46.3% (25 from 54), 45.0% (18 from 40) and 42.1% (16 from 38) in groups № 1, № 2 and in the main group, respectively. Later, on the 7th day of treatment, more than half of the patients (52.6%; 20 from 38) of the main group had a regenerative-inflammatory type of cytograms. In comparison group № 2 this indicator was 35.0% (14 out of 40), and in comparison group № 1 - only 3.7% (2 out of 54). Also in the main group of patients at this stage of treatment, 5 (13.2%) cases with a regenerative type of cytograms were noted. It did not take place in comparison group № 1 and in group № 2 it was revealed only in 1 (2.5%) case. A statistically significant intergroup difference in the distribution of cytogram types had been already noted by 7th day after the start of treatment (Fig. 2).
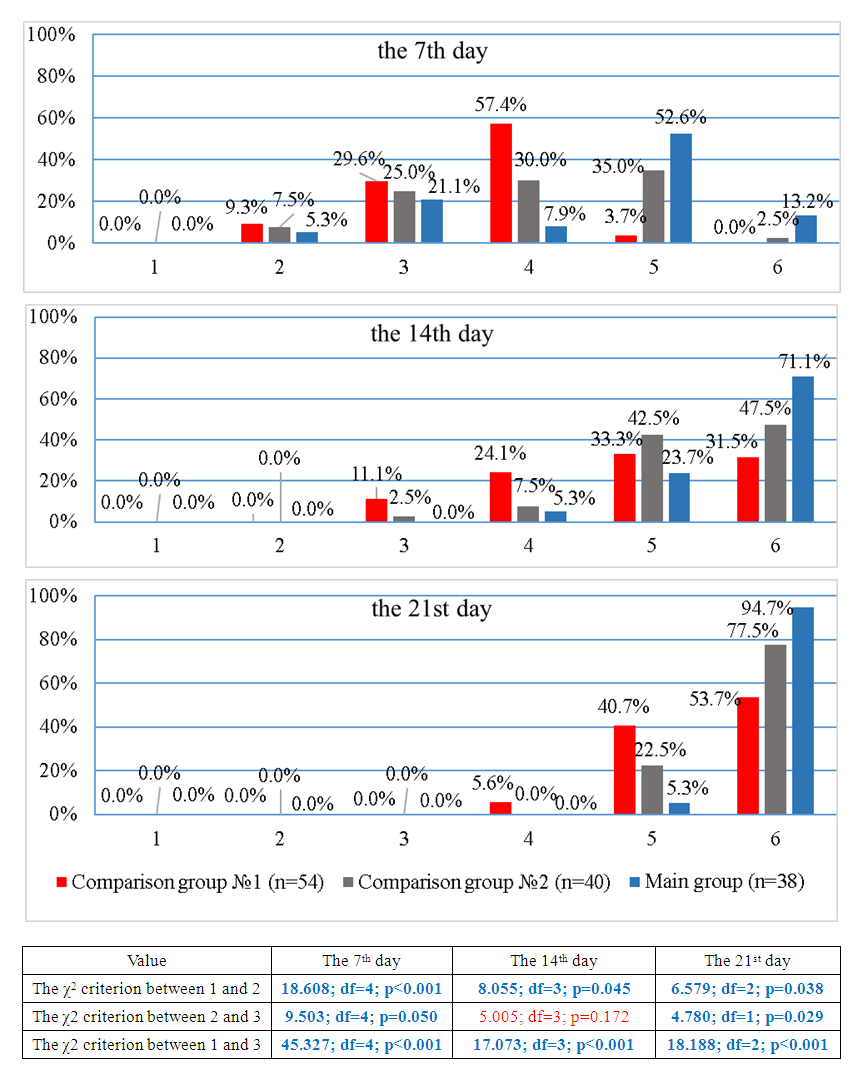 | Figure 2. Correlation of cytograms types during treatment |
5. Conclusions
- The introduction of a new method of combined local chemo-photodynamic therapy of long-term non-healing purulent wounds of soft tissues, aimed to the induction of anti-inflammatory and reparative action, allows to accelerate the transition of the inflammatory phase to the regenerative one by the 14th day in 71.1% of patients (versus 31.5% in group № 1, χ2 = 17.073; df = 3; p <0.001 and 47.5% in group № 2), and on the 21st day - in 94.7% of patients (versus 53.7% in group №1, χ2 = 18.188; df = 2; p <0.001 and 77.5% in group №2, χ2 = 4.780; df = 1; p = 0.029).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML