-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(2): 99-102
doi:10.5923/j.ajmms.20211102.06
Received: Dec. 5, 2020; Accepted: Jan. 11, 2021; Published: Feb. 6, 2021

Modern Approaches in the Treatment of Herpetic Stomatitis
Kamilov Kh. P., Ibragimova M. Kh., Kadyrbaeva A. A., Shokirova F. A.
Department of Hospital Therapeutic Stomatology, Tashkent State Dental Institute, Tashkent, Uzbekistan
Correspondence to: Kamilov Kh. P., Department of Hospital Therapeutic Stomatology, Tashkent State Dental Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Herpes viral infection (HVI) occupies one of the leading places among viral diseases in humans due to the widespread prevalence of the virus and the ability to be persistent perpetually in humans after a primary infection. According to the WHO, from 90 to 100% of the world's population are infected with herpes simplex viruses (HSV) of the 1st and 2nd types. Based on the results of the analysis of scientific research and scientific literature data, one can come to the conclusion that there is a need for large-scale research on this problem in Uzbekistan. The aim of research was to study of the effectiveness of applying biological active additive Reptin-plant within the complex treatment of herpetic stomatitis patients and therapeutic effect of photodynamic therapy with the PDU device in patients with HSV. Under our supervision, there were 85 patients diagnosed with HSV at the age of 18 to 40 years, divided into three groups, depending on the therapy. All patients were mainly treated on an outpatient basis. Analysis of the data obtained from the treatment results showed that the group of patients with HSV received complex treatment (traditional treatment + Reptin-plant + PDU) was more effective than traditional therapy alone.
Keywords: Herpes viral infection, Adhesion, PDU, Oral mucosa
Cite this paper: Kamilov Kh. P., Ibragimova M. Kh., Kadyrbaeva A. A., Shokirova F. A., Modern Approaches in the Treatment of Herpetic Stomatitis, American Journal of Medicine and Medical Sciences, Vol. 11 No. 2, 2021, pp. 99-102. doi: 10.5923/j.ajmms.20211102.06.
Article Outline
1. Relevance
- The problem of treating oral mucosa (OM) diseases is one of the topical tasks of practical dentistry. Despite the achievements of modern science, the effectiveness of most drugs and methods for treating OM remains at an insufficient level. It is important to take into account the fact that if a sufficiently effective drug is available, it is very important to select the optimal dosage for each patient individually, as well as to assess the pharmacodynamic properties of the drug during treatment, since at this time it is sometimes possible to activate or inhibit the adaptive mechanisms of the body. It should also be noted that the emergence of bacterial resistance to drugs is a constant obstacle on the path of effective therapy of OM diseases [4,11,14,15]. Along with the procedures mentioned above, the attempts to use photodynamic therapy in the field of medicine have arisen. A special place in among them is PDU, in which the therapeutic effect is achieved due to the simultaneous influence of several radiations [3,8,9,12].Herpes viral infection (HVI) occupies one of the leading places among viral diseases in humans due to the widespread prevalence of the virus and the ability to be persistent perpetually in humans after a primary infection. [5,13].According to the WHO, from 90 to 100% of the world's population are infected with herpes simplex viruses (HSV) of the 1st and 2nd types. This is mainly due to the introduction of new medical technologies and a significant increase in the number of patients with immunodeficiency, manifested in children by the development of a dysbiotic state of the oral cavity [1,2].In herpetic stomatitis, there is a mutual action of herpes viruses and immune complexes of the human body, as a result of which it is possible to activate the inflammatory process, which occurs in a chronic form. Based on this, the treatment of a chronic inflammatory process with antiviral agents alone is clearly not enough. [5,10,13].Modern antiviral drugs can affect HSV either at the stage of adhesion to the cell membrane, or at the stage of penetration into the cell, or on the replication of viral particles, but they do not affect the virus that is in a latent state and cannot prevent the onset of its activation, i.e. relapse of the disease. [6,7,10].Despite numerous works devoted to the study of herpetic lesions of the oral cavity in patients, their diagnosis, prevention and treatment methods, the trend towards an increase in this pathology persists, and therefore it remains relevant to develop a regimen of complex treatment of the herpetic stomatitis based on the identified pathogenetic mechanisms. Based on the results of the analysis of scientific research and scientific literature data, one can come to the conclusion that there is a need for large-scale research on this problem in the Republic.
2. The Purpose of the Study
- The study of the effectiveness of applying biological active additive Reptin-plant within the complex treatment of herpetic stomatitis patients and therapeutic effect of photodynamic therapy with the PDU device in patients with HSV.
3. Materials and Methods
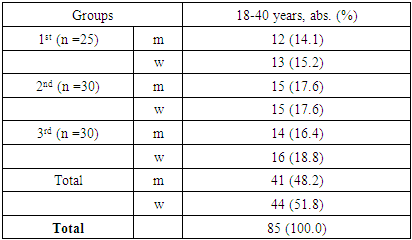
- Under our supervision, there were 85 patients with HSV, at the age of 18 to 40 years, they were divided into three groups, depending on the therapy, 25 (29.4%) patients were treated in the traditional way, traditional therapy (TT) (1st group). 30 (35.3%) patients - group 2, along with TT, additionally received a biologically active food supplement based on a lipid concentrate from the biomass of snakes of the genus ERYX - Reptin-plant (made in Uzbekistan). 30 (35.3%) patients - group 3, along with TT and a biological active food supplement based on a lipid concentrate from the biomass of snakes of the genus ERYX – Reptin-plant, additionally received photodynamic therapy (PDT). All patients were mainly treated on an outpatient basis.All subjects were diagnosed with HSV based on clinical symptoms. The severity of the disease was assessed by the severity of toxicosis and the area of lesion of the mucous membrane. Acute and chronic respiratory diseases noted in the anamnesis of patients in both groups, including influenza, tonsillitis, sinusitis, chronic pathologies of the gastrointestinal tract, hepatobiliary system, etc.We found out the presence of complaints of headache, nausea. The skin, which could be pale, was examined. Body temperature could rise to 38°. At the peak of the rise in temperature, increased hyperemia and pronounced edema of the oral mucosa, elements of the lesion were detected. We counted the number of lesion elements and found out the number of relapses per year. The presence of increased salivation, the consistency of saliva (viscous, stringy) was determined. The presence of inflammation and bleeding of the gums was found out. The possibility of repeated rashes was ascertained (during the examination, attention was paid to the elements of the lesion at different stages of clinical and cytological development). Examination on edematous and hyperemic OM revealed multiple, often grouped and merging into each other, sharply painful aphthae, covered with a yellowish-white fibrinous coating. In some patients, in parallel with the above, there was a rash of groups of small bubbles on the red border of the lips and the adjacent skin of the perioral area. All identified symptoms were recorded in the patient's medical history.In the treatment of the 1st group, the traditional scheme of therapy was used: Local therapy included painkillers before and after eating food, irrigation of the oral cavity with chlorhexidine solution (1: 1 with distilled water up to 3 times a day), as well as application of 0.25% oxolinic acid ointment (3-4 times a day for 7-10 days). We applied these ointments to the tip of the tongue and then spread them on the surface of the OM and the red border of the lips.In the 2nd group, the treatment was distinguished by the fact that, along with the generally accepted traditional therapy, we added the biological active additive Reptin-plant before meals, 1-2 capsules 3-4 times a day for 30 to 60 days.It stimulates the immune system, has a general strengthening and tonic effect.Patients of the 3rd group (n = 30 of the third), along with traditional and general treatment, additionally received a biological active supplement Reptin-plant - before meals, 1-2 capsules 3-4 times a day, also were irradiated with an PDU device with a wavelength of 620-650 nm with a density-power of 200 mW/cm2 using a mirror-lens light guide). The distance from the end of the radiator to the wound surface is 2-3 cm, the exposure time is 15-20 minutes. Depending on the area of the wound surface, the frequency of the procedure was 3-6 sessions. Local irradiation was performed when localized on the red border of the lips, on the border with the skin, as well as when localized in the oral cavity (cheeks, tongue, traumatic areas of the oral mucosa).
4. Results and Discussion
- All patients after a set of diagnostic measures in accordance with the clinical classification (Maksimovskiy Y.M., Maksimovskaya L.N., Orekhova L.Y., 2002) and with ICD-10 (1997), the diagnosis “Herpetic stomatitis caused by the herpes simplex virus [herpes simplex virus I (HSVI)] (B00.2X, K12.02)" was made.Drug-free, anti-relapse method of treatment of herpes lesions of the oral cavity in patients with HSV is the - PDU device, taking into account the difficulties of drug treatment of the oral cavity, the formation of resistance of pathogens to drugs, the wide spread of drug allergies, the widespread increase in the number of allergic diseases, including those induced by viral invasion, the increase in the severity of their course and manifestation at an earlier age.Photodynamic therapy (PDT) is a method of local activation by light of a photosensitizer accumulated in a tumor, which in the presence of tissue oxygen leads to the development of a photochemical reaction that destroys tumor cells. The mechanism of PDT action is represented as follows: a photosensitizer molecule, having absorbed a quantum of light, passes into an excited triplet state and enters into two types of photochemical reactions. In the first type of reactions, interaction occurs directly with the molecules of the biological substrate, which ultimately leads to the formation of free radicals. In the second type of reactions, an excited photosensitizer interacts with an oxygen molecule to form singlet oxygen, which is cytotoxic for living cells, due to its property of a strong oxidizing agent for biomolecules. A 0.05% methylene blue buffer solution was used as a photosensitizer with a 30 min exposure. Then, after washing off the photosensitizer from the wound surface, the wound surface was irradiated with the PDU-1 device. Wavelength is 620-650 nm with a power density of 200 mW/cm². The distance from the end of the radiator to the wound surface was 2-3 cm with the absence of thermal discomfort to the patient. The duration of treatment was 15-30 minutes, depending on the area of the wound surface. After radiation of the wound surface, the photosensitizer becomes discolored, since a photodynamic reaction has started. The frequency of the procedure was 3-6 sessions, depending on the clinical diagnosis.
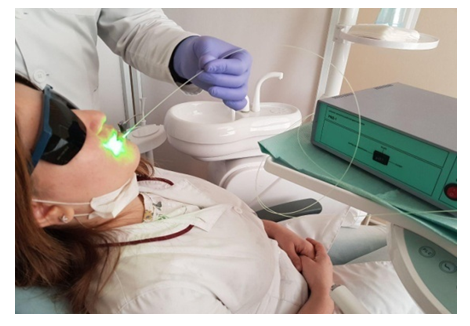 | Figure 1. Radiation of the oral cavity with the device PDU |
|
|
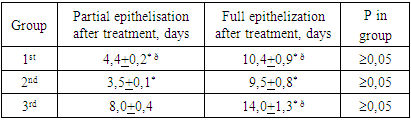
5. Conclusions
- Complex treatment of children with HSV was more effective, as evidenced by the results of the 3rd group. When using PDU, traditional therapy and a biologically active food supplement based on a lipid concentrate from the biomass of snakes of the ERYX genus - Reptin-plant (made in Uzbekistan), patients of the 3rd group observed earlier disappearance of symptoms of HVI intoxication and pain in the oral mucosa, enhanced result of complete epitilization, a decrease in the frequency and severity of relapses, as well as an increase in the duration of remission.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML