-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(2): 95-98
doi:10.5923/j.ajmms.20211102.05
Received: Dec. 3, 2020; Accepted: Jan. 8, 2021; Published: Feb. 6, 2021

Methods of Rehabilitation Treatment and Orthopedic Prosthetics of Oncological Patients with Postoperative Defects in Maxillofacial Area
Ubaydullayev K. A.1, Gafur-Akhunov M. A.2, Gafforov S. A.3
1Member of Association of Oncologists and Dentists of Russia and Republic of Uzbekistan, Tashkent Institute of Postgraduate Education for Doctors, Tashkent, Uzbekistan
2Head of Oncology Department at Tashkent Institute of Postgraduate Medical Education, Republican Research Oncological Center, Tashkent, Uzbekistan
3Head of Stomatology, Pediatric Dentistry and Orthodontics Department, Chair of Stomatology, DM. Tashkent Institute of Postgraduate Medical Education, Tashkent, Uzbekistan
Correspondence to: Ubaydullayev K. A., Member of Association of Oncologists and Dentists of Russia and Republic of Uzbekistan, Tashkent Institute of Postgraduate Education for Doctors, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: This study aimed to demonstrate the usefulness of our rehabilitation program after extensive surgeries inpatients with maxillofacial area (MFA) and neck tumors. Methods: Data from patients who underwent surgery in the clinics of the Republican Oncological Research Center and theTashkent Institute of Postgraduate Medical Education for MFA and neck tumors were retrospectively analyzed. The patients were enrolled to our rehabilitation program, which consisted of a three -staged technique involving a complex prosthesis, and several physical therapies for damaged functions, such as chewing, swallowing, and breathing. Results: A total of 107 oncological patients with postsurgical defects were fitted with various types of prosthesis. Theintroduction of our rehabilitation program was performed at an interval between initial surgery and prosthesis formation of 10-15 days, and between initial surgery and preparation of the final prosthesis of 26–30 days. A restoration of the Karnofsky performance status to 80%–85% was observed. Conclusion: The present study demonstrates that our rehabilitation program is useful for shortening the postoperative con-valescent period and improving the quality of life of patients with defects of the MFA and neck.
Keywords: Maxillofacial tumor, Prosthesis, Defect, Plasty, Rehabilitation
Cite this paper: Ubaydullayev K. A., Gafur-Akhunov M. A., Gafforov S. A., Methods of Rehabilitation Treatment and Orthopedic Prosthetics of Oncological Patients with Postoperative Defects in Maxillofacial Area, American Journal of Medicine and Medical Sciences, Vol. 11 No. 2, 2021, pp. 95-98. doi: 10.5923/j.ajmms.20211102.05.
1. Introduction
- Tumors of the maxillofacial area (MFA) and neck are one of the most important health problems worldwide [1,2,3]. In our country (Uzbekistan), approximately 82% of patients with MFA and neck tumors are referred to otorhinolaryngologists, 10%–11% to stomatologists, and 7%–8% to oncologists. After referral from physicians, these specialists appropriately diagnose and evaluate the extent of the disease. However, doctors in the emergency room setting may not pay much attention to the related symptoms, and the complexity of the differential diagnosis may result in delayed diagnosis of head and neck tumors [4,5]. The best results, in terms of survival, are obtained through a combination of chemotherapy, radiation and surgical treatment. However, surgery on the MFA is often accompanied by complex and serious defects, which can result in disturbance of the functions of chewing, swallowing, respiration, and speech [6,7,8]. Furthermore, cosmetic changes to the face may have a negative influence on the patients’ mental state, and their return to society is another major problem of MFA and neck tumors.An effective method of early rehabilitation is correction of the defects with a prosthesis. In addition, orthopedic treatment is used along with reconstructive surgeries to adjust the prosthesis so that several related problems such as infection, immunity attenuation and/or unfitted braces can be prevented. Early intervention to address the defects is important because the early preparation of a prosthesis allows restoration of the lost functions and even improves the patient’s psychological condition [9,10].In our institutes, early rehabilitation consists of a three-step reconstruction process, improvement in complex exercises, articulating gymnastics, mechanotherapy directed at the accurate alignment of the lower jaw, and restoration of the damaged functions of chewing, swallowing, and breathing. This program has been utilized to improve the quality of life (QOL) of patients with MFA and neck tumors. In the present study, we will demonstrate the results of our rehabilitation program.
2. Material and Methods
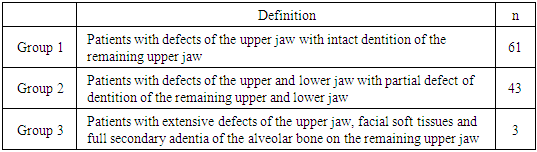
- In all, 107 patients from the clinics of the Republican Oncological Research Center and the Tashkent Institute of Postgraduate Medical Education, who had postoperative defects of the MFA due to tumors, were included in the present study. Traditional methods of clinical examination, surgical interventions, radiation therapy, chemotherapy, immunological reactivity and psycho-neurological body resistance, as well as methods of study of complex jaw prostheses were applied during the research.These 107 patients were divided into three groups ac-cording to the locations of their defects: Group 1, patients with defects of the upper jaw with intact dentition of the remaining upper jaw; Group 2, patients with defects of the upper and lower jaw with a partial defect of dentition of the remaining upper and lower jaw; and Group 3, patients with extensive defects of the upper jaw, facial soft tissues and full secondary adentia of the alveolar bone on the remaining upper jaw. This categorization allows us to plan the appropriate rehabilitation program for each patient.
3. Results
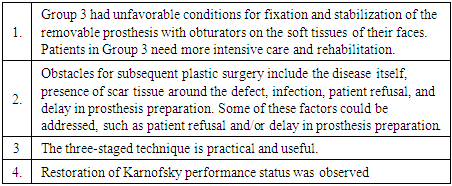
- 107 oncological patients with postoperative defects of the MFA were fitted with various types of prosthesis. Patients were both men and women, aged between 20 and 70 years of age, with the majority having Stage III or IV disease, while a small percentage had Stage I or II disease. The pathological diagnoses included cancer, sarcoma, melanoma, and other malignant tumors of the MFA and neck. The author Ubaydullaev received two patents for endo-prosthesis and exo-prosthesis (Certificate #000875, #000876 – 09.09.2018). Thirteen patients had extensive defects of the up-per jaw, facial soft tissues and full secondary adentia of the alveolar bone on the remaining upper jaw (Table 1). Consequently, these patients had defects of the right and left parts of the maxilla, large defects of the eye and soft tissues of the face, defects of the alveolar process of the mandible, and/or defects of the nose and ear skin. We found that the patients in Group 1 and 2 had the most favorable conditions for fixation of the removable pros-thesis with obturators, while patients in Group 3 had un-favorable conditions for fixation and stabilization of the removable prosthesis with obturators on the soft tissues of their faces.
|
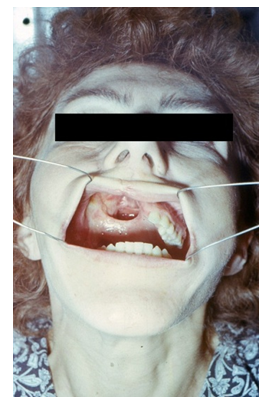 | Picture 1. Before surgery |
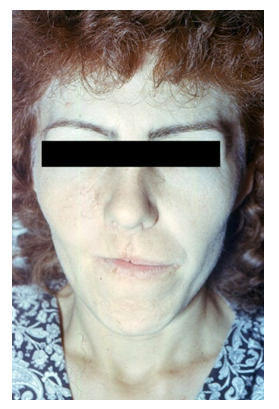 | Picture 2. Before rehabilitation |
 | Picture 3. After rehabilitation |
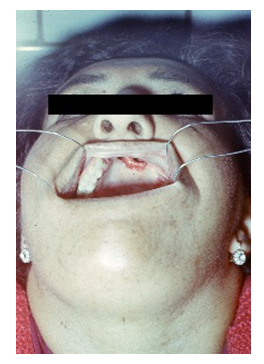 | Picture 4. Before surgery |
 | Picture 5. Before rehabilitation |
 | Picture 6. After rehabilitation |
4. Conclusions
- In the present study, we have found several important results (Table 2). First, Group 3 had unfavorable conditions for fixation and stabilization of the removable prosthesis. Because the patients in Group 3 had severe defects of the MFA, there is no argument that preparing prostheses for these patients is much more difficult than for other patients. However, confirming this result is quite important, because the patient categorization used in the present study is useful for identifying patients needing closer attention.
|
ACKNOWLEDGEMENTS
- This work is supported, in part, by the non-profit organization Epidemiological & Clinical Research Information Network (ECRIN).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML