-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(2): 79-83
doi:10.5923/j.ajmms.20211102.01
Received: Jan. 8, 2021; Accepted: Jan. 23, 2021; Published: Jan. 25, 2021

Improving the Effectiveness of Surgical Treatment of Patients with Odontogenic Cysts of the Jaw
Zaynutdinov M. O.1, Makhkamov M. E.2, Yusupalikhodjaeva S. Kh.3, Patkhiddinova M. Sh.3
1Tashkent State Dental Institute, Department of Oral and Maxillofacial Diseases and Traumatology, Tashkent, Uzbekistan
2Medical Institut of Karakalpakstan, Department of Dentistry, Tashkent, Uzbekistan
3Tashkent State Dental Institute, Tashkent, Uzbekistan
Correspondence to: Zaynutdinov M. O., Tashkent State Dental Institute, Department of Oral and Maxillofacial Diseases and Traumatology, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Clinical studies were carried out in 50 patients with radicular cysts of the upper and lower jaw. The aim of the study is to increase the efficiency of surgical treatment of patients with odontogenic cysts of the jaws with a rationale for the choice of osteoplastic drugs. Filling of the cystic cavity with osteoplastic material with the addition of an antibiotic provides good immediate and long-term results of surgical interventions. The processes of formation of newly formed bone tissue are more active. The use of bone replacement materials allows you to completely close a large cavity, while the degree of reparative osteogenesis does not decrease.
Keywords: Osteogenesis, Biomembrane, Bone grafting, Bioceramics, Bioglass, Osteoplasty
Cite this paper: Zaynutdinov M. O., Makhkamov M. E., Yusupalikhodjaeva S. Kh., Patkhiddinova M. Sh., Improving the Effectiveness of Surgical Treatment of Patients with Odontogenic Cysts of the Jaw, American Journal of Medicine and Medical Sciences, Vol. 11 No. 2, 2021, pp. 79-83. doi: 10.5923/j.ajmms.20211102.01.
1. Introduction
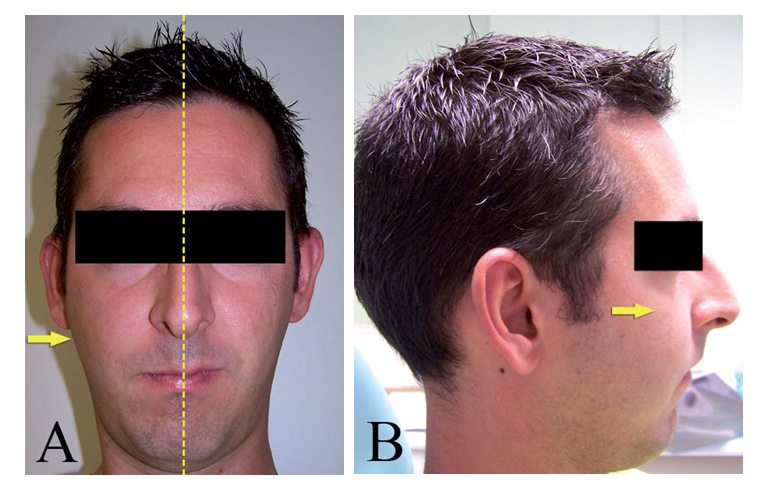
- Odontogenic cysts (OC) are the most frequent lesions of the upper jaw and the presence of a web is composed of epithelial tissue of odontogenic origin [1,8].The etiology of OCs is explained by the presence of odontogenic cells remaining enclosed in the bone tissue or gingival tissue covering the upper or lower jaw, such as epithelial Malassez residues, dental plate or enamel organ (OC development). However, in other cases cysts are formed by inflammatory processes. In most cases, the lesions are true cysts with a complete and sealed epithelial lining [1,3]. Most of the latest World Health Organization (WHO) classification of redistributed keratocysts (keratinized primordial cysts) in the classification of tumours of the upper jaw under the term "kerato-cystic odontogenic tumour" (CAT) [4,9]. Its slow, extensive and non-penetrating growth provides clear evidence of its harmlessness - a situation that can facilitate late diagnosis. The appearance of signs such as cortical enlargement (Figure 1), dental dislocation or the appearance of pain or infectious symptoms should alert the doctor to the possible presence of a pathological cyst. Routine radiological examination based on panoramic radiographs reveals the presence of characteristic masses (Figure 2) [1,2,3,5].
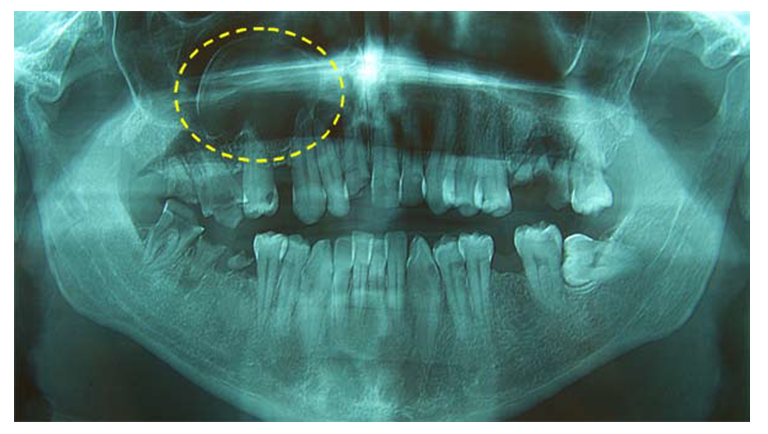 | Figure 2. Residual cyst in the first quadrant, displacing the sinus wall |
2. Patients and Methods
- Own clinical trials were conducted in 50 patients with upper and lower jaw radicular cysts. We used autogenic blood plasma (a blood fraction consisting of leukocytes and fibrin proteins in addition to platelets) as a means of stimulating osteogenesis. The basis of plastic material was bioactive glass with antibiotic. Surgical treatment included dissection of a radicular cyst of the jaw - cystectomy, with resection of the tooth root tip and plastic closure of the defect by bioactive glass with antibiotic on the "pillow" of autogenous blood plasma. The study was carried out in 50 patients aged 19 to 45 years, while in 30 patients - bone cavity diameter was from 0,5 to 1 sm, in 20 patients - more than 1 sm. Clinical examination was conducted according to the generally accepted standard scheme. Anamnesis data were read out, including complaints, development of the present disease, presence and absence of concomitant pathology. All patients were divided into 3 groups according to the osteoplastic material used to fill the postoperative bone defect after cystectomy (Table 1): 1 - comparison group - 12 patients in whom the postoperative bone cavity healed by transformation of the blood clot.2 - main group - 21 patients, the course of operation as in classical cystectomy, postoperative bone cavity (bone cavity diameter from 0,5 to 1 sm) was filled with bioactive glass with antibiotic. 3 - main group - 17 patients in whom the postoperative bone cavity from 1 to 2 sm was filled with microgranular osteoplastic material - bioactive glass on the "pillow" of autogenous plasma. Dynamic control of reparative osteo-regeneration processes was performed by X-ray examination for 1-2 days after the operation and further in 3, 6, 9, 12 months.
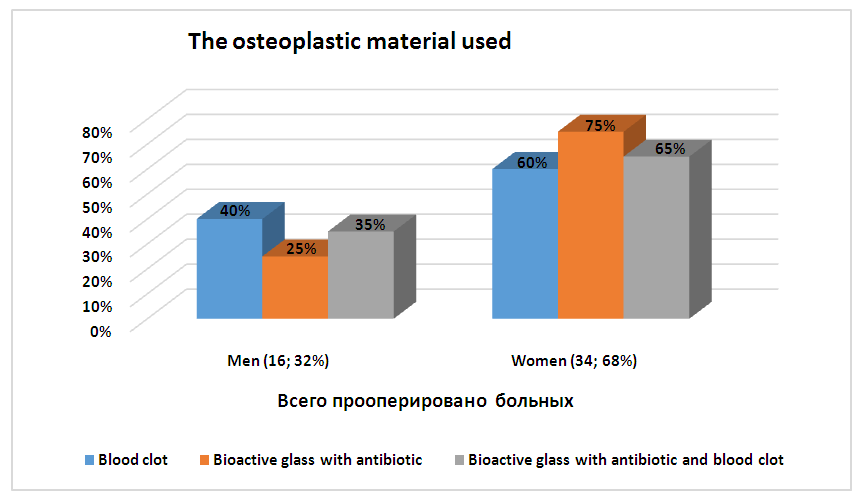 | Figure 3. Distribution of patients according to the type of osteoplastic material used |
3. Results and Discussion
- 1 group of investigated - 12 patients were operated on: men - 5 and women - 7, aged 19 to 55 years. 8 operations were performed on the upper jaw and 4 on the lower jaw. In total, 10 pericorneal and 2 follicular cysts were removed. Of them small cysts up to 1 cm in diameter were removed in 8 patients, and 4 patients over 1 sm in diameter. There were 11 resections of the tops of the roots. Postoperative wound healed by primary tension in 10 (83%) patients. The sutures were removed on 7-8 days after the operation. Spacing of the sutures with subsequent suppuration of the postoperative wound in patients with cysts up to 1 sm was noted in 1 (8%) people, in patients with a cyst diameter greater than 1 sm - in 1 (8%) cases. In total, complications in traditional treatment of cysts - 16%.Patients with postoperative complications were prescribed antibiotics, daily wound irrigation with antiseptic solutions and enzymes, physiotherapeutic procedures were performed. As a result of intensive complex treatment, wounds healed in all patients with secondary tension. Patients did not complain during the control examination, the postoperative scars were inconspicuous and painless. X-ray inspection was carried out in 1, 3, 6 and 12 months, according to the results it was found that bone regeneration in the postoperative cavities is intense, the defect contours become blurred. In 6 months the newly formed bone in postoperative defects in cysts up to 1 sm in size approaches the normal surrounding bone tissue in its structure. If the defects are more than 1.0 sm in X-ray images of the newly formed bone areas, the increased spongyness with air areas is determined, centers of darkening are preserved, the structure of the bone has a fine-shaped pattern, after 12 months - a significant reduction in air areas is noted, but complete replacement of the cavity is not observed. with defects up to 1 sm.On the basis of the treatment results of the control group cysts, in which healing of the bone cavity occurs under the blood clot, quite satisfactory not only for cysts up to 1 sm in diameter, but also more than 1 sm. At the same time, it should be noted a significant number of complications (16%), as well as delayed and imperfect regeneration of postoperative bone defects.The second group of the study includes 21 patients: men - 5 and women - 16, aged 19 to 59 years. The operation was performed using the traditional method, after which the postoperative bone defect of 0,5 to 1 sm was filled with bioactive glass with antibiotic. There were performed 16 operations on the upper jaw and 5 operations on the lower jaw. In total, 20 near root and 1 follicular cyst were removed. Twenty-one resections of the tops of the roots were performed. In the postoperative period the patients were prescribed symptomatic treatment, physiotherapy and rinsing with antiseptic agents.The postoperative wound in all operated patients healed by primary tension. The sutures were removed on the 7-8th day after the operation. Spacing of the sutures with subsequent suppuration of the postoperative wound occurred in 1 patient. Patients with postoperative complications were prescribed antibiotics, daily wound irrigation with antiseptics, enzymes, physiotherapy treatment was carried out. As a result of intensive, complex treatment, the wound healed by secondary tension. Patients did not complain during the control examination, postoperative scars were inconspicuous and painless. The results of treatment were traced in 18 patients within the period from 1 month to 2 years. Dense bone tissue was determined at the defect site. The teeth within the defect are stable. X-ray examination found that the active regeneration of bone tissue at the site of the former defect begins in the second month and after 3-6 months, the contours of small defects to 0,5 sm become inconspicuous. In 6 months after the operation, the local status without any special features, dense bone tissue is palpated. On the X-ray the postoperative cystic cavity is filled with newly formed bone. With defects of more than 1.0 sm - there is a thinning of the area of the implant inserted along the edges, in some places, the incomplete merging with the border of the actual bone fragments of the jaw in terms of 12 months, 24 months later the picture remains unchanged - in this case, the visual defect is not visualized incompletely filled, but such a state of bone on the X-ray does not allow for dental implantation at the defect site.Thus, cystic cavity filling provides good immediate and distant results of surgical interventions. The processes of forming newly formed bone tissue are more active. However, the full recovery of cystic defect in cysts over 1 sm in diameter does not occur even within a year after surgery.The third group of patients undergoing cystectomy with simultaneous filling of the postoperative bone cavity with bioactive glass on the "pillow" of autogenic plasma was performed in 17 patients: 6 men and 11 women aged 20 to 56 years. A cyst up to 2 sm in size was made in 13 patients, more than 2 sm - in 4 patients, 1 patient had a "causal" tooth removed. Due to the large diameter of the cyst, the tooth located in the cavity of the cyst is mobile and cannot be cut, its removal is performed. The nearest results of the operation in all patients were satisfactory. The sutures were removed on day 7-8. In terms of 1 month to 2 years, the results of treatment are traced in all patients.At examination after 1 month patients did not complain. Blurred contours of the bone defect are determined on R-grams. In 3 months after the cysts were removed, the defect decreased by 1/3. Defect contours are blurred. Newly formed bone tissue is clearly defined at the defect periphery.In 6-9 months the average bone cavity of the defect is filled by 2/3. The newly formed bone intensively develops towards the root tip of the adjacent teeth and to the center of the cavity. By the 9-10th month, most of the medium size cysts had a complete recovery of bone defects. Final recovery of bone defects with small areas of thinning in patients of this group was noted in 1 year after the operation, in 24 months - in the area of defects - is determined by the dense tissue of the bone structure without air areas of sufficient density for X-rays transmission, At the same time, the newly formed bone tissue with coarse trabecular pattern, the boundaries of the alveolar ridge are smooth and clear, its overall height is not reduced, the structure of bone tissue coarse throughout.Based on the results of this study, the use of enriched autogenic plasma and bioactive glass allows to completely close the large cavity, while the degree of reparative osteogenesis is not reduced. Two patients (11,7 %) had incomplete bone cavity recovery (cyst size more than 2 sm) during control examination in 1,5 years. In 1 (5,8 %) patients the development of inflammatory complications of the postoperative wound at control after 6 months was noted.Comparison of bone tissue regeneration terms in the defect area allowed to establish the osseointegration level after each drug use, severity of the postoperative period. Use of stimulating bioactive material allowed to optimize the healing process of bone wounds, identify new opportunities to increase their regenerative capacity and tissue recovery.
4. Conclusions
- The use of biocomposite material of bioactive glass promotes the more active flow of regeneration processes in bone defects, causing the energy formation of connective tissue in them and on its basis - bone structures. Filling the postoperative defect with composite material has a positive effect on the course of the postoperative period, which is expressed in a significant reduction of postoperative soft tissue edema, the absence of pain syndrome, lower temperature reaction. Large bone cavity, bone defects can not be replaced by a conservative treatment or simple surgery, so to restore lost bone tissue should use a combination of synthetic materials that can replace the lost bone or have an inducing effect on the regeneration processes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML