-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(1): 46-52
doi:10.5923/j.ajmms.20211101.12
Received: Dec. 7, 2020; Accepted: Jan. 15, 2021; Published: Jan. 25, 2021

Studying of the Remote Results in the Application of Intrauterine Contraception after Cesarean Section
Nasirova Zebiniso Azizovna
Samarkand State Medical Institute, Uzbekistan
Correspondence to: Nasirova Zebiniso Azizovna, Samarkand State Medical Institute, Uzbekistan.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Contraception for women in the postpartum period must be highly effective, safe (allowed for use in the postpartum period, do not contain estrogens) and acceptable (prolonged). The method of long – term reversible contraception-intrauterine contraception (IU) – is a safe method that is suitable for most women. To study the effect of intrauterine contraception on the state of the reproductive system, ultrasound examination of the pelvic organs in dynamics in the postoperative period for 12 months in patients with IUD was performed. When using IUD intraoperatively and at intervals throughout the year, the echographic picture of the reproductive system does not differ significantly from those of women who did not use contraception. It was found that the localization of the IUD inside the uterus may change during the first three to six months after administration. This may be due to bleeding, pain, and expulsions.
Keywords: Cesarean section, Intraoperative, IUD, Echographic parameters, Contraception, Expulsion
Cite this paper: Nasirova Zebiniso Azizovna, Studying of the Remote Results in the Application of Intrauterine Contraception after Cesarean Section, American Journal of Medicine and Medical Sciences, Vol. 11 No. 1, 2021, pp. 46-52. doi: 10.5923/j.ajmms.20211101.12.
1. Introduction
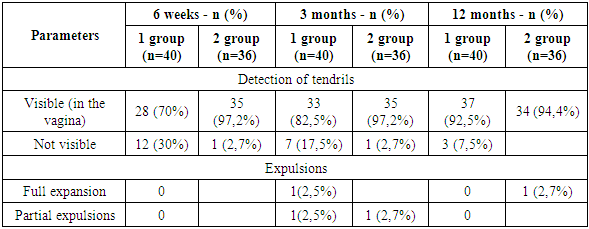
- High frequency of abdominal delivery is a distinctive feature of modern obstetrics. Currently, the frequency of this operation is steadily increasing. In Uzbekistan, over the past 10-15 years, its frequency has more than doubled, and according to the statistical Department of the RSNPMC A and G and the ROC in 2017, it was 18%, reaching up to 35-40% in some institutions [21].The increase in the frequency of operative delivery creates a new problem - an individual approach to choosing the optimal method of contraception in women with a uterine scar after cesarean section in order to best observe the interval between deliveries.The most important factor in maintaining the reproductive health of women who have undergone cesarean section is to solve the problem of unwanted pregnancy and to observe the intergenetic interval. Artificial abortion is a severe physical, psychological and hormonal stress that leads to functional and organic disorders in the reproductive system [18]. In this regard, the use of contraception is considered as one of the most important areas in the rehabilitation of women after operative delivery.An essential element of preserving women's reproductive potential after CS surgery is ensuring an adequate interval between pregnancies and childbirth. The most optimal interval between childbirth is from 3 to 5 years. Pregnancy earlier than 2 years, even after natural birth, is associated with a high risk of complications: miscarriage, bleeding, postpartum and inflammatory diseases, uterine ruptures, and maternal mortality [11,20]. However, ensuring an adequate interval between pregnancy and delivery is especially important for women with uterine scarring due to the increased risk of pregnancy and delivery complications. This becomes possible only with the use of effective planned contraception. Contraception for women in the postpartum period must be highly effective, safe (allowed for use in the postpartum period, do not contain estrogens) and acceptable (prolonged). The method of long – term reversible contraception-intrauterine devices (IUDs)– is a safe method that is suitable for most women.The main advantage of long-term reversible contraception methods is that they do not require constant effort on the part of the user. In addition, after removal of the contraceptive, fertility is rapidly restored [21,26].The period immediately after delivery is particularly well suited for the introduction of an IUD. Women who have just given birth to a child are usually highly motivated to use contraception; it is safe to rule out pregnancy, and the introduction of a contraceptive during a hospital stay is convenient for both patients and medical professionals. In addition, there is a risk of unwanted pregnancy in the period immediately after delivery [17].It is the postpartum period that is an important time to start using an effective method of contraception in order to increase the interval between pregnancies. This is especially important for women after CS surgery.Thus, the postpartum period is an important time to start using an effective method of contraception in order to increase the interval between pregnancies, which is especially important for women after CS surgery. One of the most suitable solutions is the use of prolonged reversible contraception-IUD-highly effective and long-acting contraceptives. The use of these methods of contraception allows you to ensure an adequate interval between pregnancies and childbirth and thereby preserve the reproductive potential of women after CS surgery.All of the above determines the need to study the reproductive behavior of women after cesarean section and optimize the use of highly effective methods of contraception in women with a scar on the uterus.The location of the IUD inside the uterus may change during the first three to six months after administration. This may be due to bleeding, pain, and expulsions. Some authors have found that after 6 weeks, the distance from the upper edge of the IUD to the bottom of the uterus of more than 10 mm will lead to expulsions after 24 weeks with interval IUD administration [9,12]. Among women with interval IUDs, expulsions occurred at a lower position inside the uterus, while women did not have the desire to remove the IUDs due to side effects. An IUD administered post-placentally will have a different localization inside the uterus compared to an interval injection [10,16].The main goal of the study was to study the long-term results of using IUDs post-placentally and at intervals (after 6 weeks) in women who underwent cesarean section.
2. Method of Research
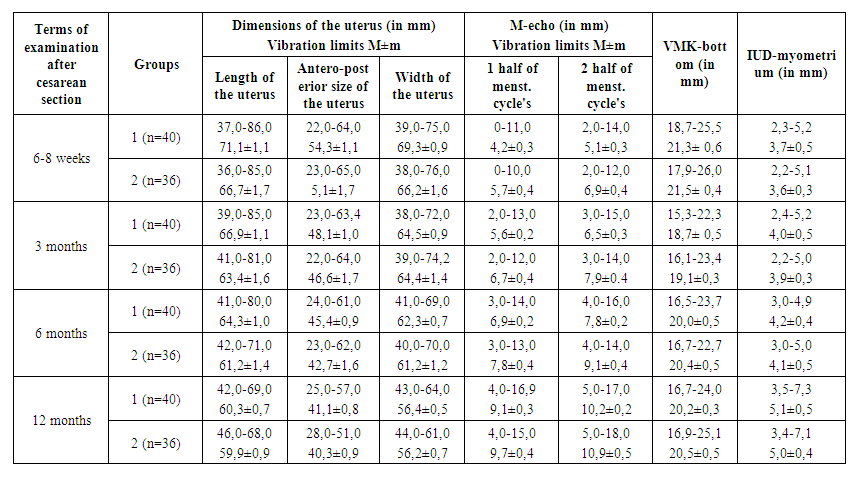
- A prospective study was conducted in the city Maternity hospital No. 2 in Samarkand to assess the long-term results of post-placental and interval administration of CU T 380 A IUD in women who underwent cesarean section. The study included 76 women who were delivered by caesarean section and wanted to use the CU T 380 A IUD, who met the who standard medical criteria for IUD administration and were willing to follow the study Protocol. The exclusion criteria were: women who do not meet the who medical eligibility criteria for the use of IUDs.Women were consulted about post-placental and interval IUD administration during prenatal visits and / or after hospitalization. The women were told in detail about the study, including the advantages and limitations of different methods, and repeated counseling was performed before the caesarean section. Written informed consent was obtained from women who were willing to participate in the study and comply with the study Protocol.Post-placental insertion of the IUD was performed after removal of the placenta using Kelly forceps / manually through a uterine incision, and the device was placed on the bottom of the uterus. No attempt was made to direct the IUD tendrils into the vagina. Antibiotics were administered according to the Protocol of the maternity hospital for caesarean section. The women were monitored daily for postpartum bleeding, as well as any other complaints, throughout their hospital stay. Interval administration of IUDs was administered in the usual sterile manner, as described in the manufacturer's instructions for a 6-week postpartum visit. Before discharge, patients were indicated on the exchange card: VMC type, date of introduction, and expiration date. Participants were asked to return for scheduled follow-up visits in 6 weeks, 3 months, 6 months, and 12 months.Outcomes and side effects the use of IUDs after 6 months was determined by confirming the presence of IUDs in the uterus during physical examination or ultrasound. Expulsions were defined as the complete passage of the device through the cervix or the presence of an IUD in the cervical canal. Removal of the IUD was determined by the patient's report or removal documentation. Infection of the pelvic and cervical organs was thought to be present in women with purulent discharge, soreness of the cervix, appendages, or uterus, with or without fever. Patient satisfaction was determined by the patient report. Secondary outcomes included removal, expulsions, satisfaction, and adverse events such as infection, perforation, and pregnancy.To study the effect of intrauterine contraception on the state of the reproductive system, an ultrasound study of the pelvic organs was performed in dynamics in the postoperative period for 12 months in 76 patients. Echographic indicators were obtained using a real-time ultrasound detector from Toshiba (Xario SSA-660A).Ultrasound biometrics included changing three dimensions of the uterus (length, anterior-posterior size, and width), measuring M-echo, measuring the distance between the IUD and the bottom of the uterus, and measuring the distance between the IUD and the upper endometrial layer.The length of the uterine body was measured from the internal pharynx to the farthest point of the bottom in the longitudinal section. The anterior-posterior size of the uterine body was determined perpendicular to the previous measurement by the external contours of the anterior and posterior walls in the widest part of the uterine body. The width of the uterine body was measured by cross-scanning in the widest part from the right to the left contour of the side walls of the uterine body.Ultrasound of the endometrium assessed its thickness, structure, and compliance with the phase of the menstrual cycle. To assess the thickness of the endometrium, anterior-posterior m-echo measurement was used for longitudinal scanning of the uterus.The thickness of the anterior wall was measured in the projection of the scar, and attention was paid to the state of the ovaries.The first assessment of the state of the reproductive system was carried out 6-8 weeks after the start of contraceptive use, and then 3-6-12 months later. Particular attention was paid to the localization of the IUD, changes in values from the upper edge of the IUD to the bottom of the uterus, and the distance between the IUD and the upper endometrial layer.The conducted studies showed that the echographic parameters changed in the dynamics of the postoperative period and were in a certain dependence on the contraceptive used.
3. Results and Discussion
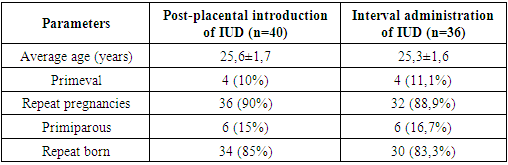
- A prospective study was conducted in the city Maternity hospital No. 2 in the city of Samarkand. To assess the echographic parameters of post-placental and interval administration of CU T 380 A IUDs in women who underwent cesarean section, the study included 76 women who were delivered by caesarean section and wanted to use CU T 380 a IUDs. All women met the who standard medical criteria for IUD administration and were prepared to comply with the study Protocol.The majority of women were between 21 and 30 years old (77.89%). Two women (4%) were over 36 years old and only one woman was under 20 years old (table 1).
|
|
 | Figure 1. VASH Scale |
|
 | Table 4. Echographic parameters in the dynamics of women using the IUD |
4. Conclusions
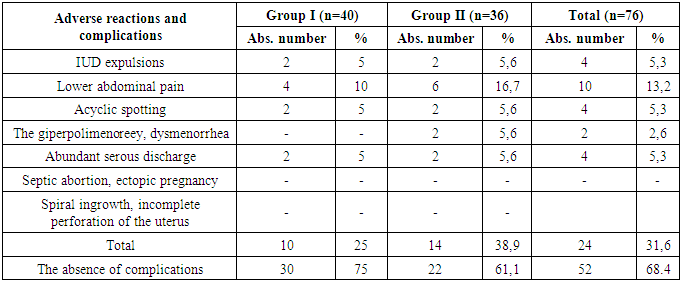
- Thus, properly selected contraception provides high efficiency and acceptability and thus plays a crucial role in maintaining women's reproductive health. Increasing access to contraception is a way to preserve the health of women and children and reduce maternal and infant mortality. Ensuring satisfaction with obstetric and perinatal care and family planning will reduce: maternal mortality by more than 2/3 (from 358,000 to 105,000); neonatal mortality by more than half (from 3.2 to 1.5 million); the number of unwanted pregnancies increased by more than 2/3 (from 75 to 22 million); the number of unsafe abortions - from 20 to 5.5 million; the death rate from unsafe abortions-by more than 4/5 (from 46,000 to 8,000). Every dollar spent on contraception saves $ 1.40 of costs for obstetric and perinatal care [11,18].Our results indicate that for the majority of women who have had a cesarean section, IUD does not have an adverse effect on their health and is a completely acceptable method of contraception, provided that its technology is followed. Adverse reactions in most women were transient and disappeared independently during the first 3-4 months of contraception.When using copper-containing intrauterine contraceptives administered to patients during cesarean section, when observed for 12 months, the echographic indicators of the reproductive system do not differ significantly from women who did not use contraception. The practice of installing a post-placental IUD during cesarean section is safe, but follow-up may differ from that of patients with normal interval management of IUD. It was also found that after 6 weeks, a distance of less than 10 mm from the upper edge of the IUD to the bottom of the uterus can lead to expulsions after some time of using the IUD.The effectiveness of contraception, short duration and low severity of adverse reactions allow the use of IUDs in women after abdominal delivery post-placental and interval.It should be noted that in our study there were no cases of complications in the form of uterine perforation and common inflammatory diseases (endometritis, peritonitis).During the use of intrauterine contraception, involutive processes in the uterus at 12 months were 60.3±0.7 mm in length, 41.1±0.8 mm in thickness, 56.4±0.5 mm in width in women with intraoperative IUD administration and 59.9±0.9 mm in length, 40.3±0.9 mm in thickness, 56.2±0.7 mm in width in women with interval IUD administration (p<0.05).The results do not indicate any differences in changes in the morphology of the uterus and endometrium in women who underwent cesarean section, who used IUD post-placental and interval. Echographic indicators of ovarian size in women using IUD post-placental and interval did not actually differ. The average thickness of the anterior wall in the projection of the scar was 9.1±1.8 mm in women who underwent cesarean section and used IUD post-placental and interval.Thus, changes in the echographic indices of the uterus and ovaries, the average thickness of the front wall in the projection of the scar in women undergoing cesarean section, primedic intrauterine devices intraoperatively and interval, after 6 weeks suggest that depending on the reproductive system, from the hypothalamic - pituitary activity in the postoperative period and different for involutive processes and the recovery mechanism of the reproductive system under the influence of contraceptive, but these data do not differ from the time of introduction of intrauterine system.In conclusion, I would like to say that the method of long - term reversible contraception-IUD, based on their effectiveness, are high-class contraceptives, since with their ideal and typical use, the incidence of pregnancy is less than 1% per year. These drugs are characterized by the highest frequency of satisfaction and long-term use of all methods of reversible contraception.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML