-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(1): 42-45
doi:10.5923/j.ajmms.20211101.11
Received: Jun. 20, 2020; Accepted: Aug. 6, 2020; Published: Jan. 25, 2021

Surgical Treatment of Patients with Bone Chondomas
Gulrukh Sh. Umarova, Saodat U. Asilova, Nigora Z. Nazarova
Republican Scientific and Practical Medical Center for Traumatology and Orthopedics, Tashkent Medical Academy
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article is devoted to the study of chondromas of limb bones, that takes first place (84.4%) in the structure of benign tumors and tumor-like diseases. The authors present the results of the analysis of 42 patients. In most cases, it was enchondroma (33 cases - 81%). Often, pathology was foundеd in the hand bones (78.8%). The choice of bone grafting method was determined using the computer “Program for the treatment of benign tumor and tumor-like diseases of the limb bones” DGU 20180831. Evaluation of the treatment results showed that the use of bone grafting using Collapan L material improved the consolidation of the bone defect in 82% of cases, which led to early patient mobilization, reduction of rehabilitation and disability periods, and ultimately improvement of treatment results.
Keywords: Chondroma, Bone, Limb, Minimally invasive, Surgical treatment
Cite this paper: Gulrukh Sh. Umarova, Saodat U. Asilova, Nigora Z. Nazarova, Surgical Treatment of Patients with Bone Chondomas, American Journal of Medicine and Medical Sciences, Vol. 11 No. 1, 2021, pp. 42-45. doi: 10.5923/j.ajmms.20211101.11.
1. Relevance
- In the structure of neoplastic bone lesions 56.5% belongs to benign tumors and tumor-like diseases [12,15].Chondroid neoplasms of the bones are the most common benign tumor of the bone system, the percentage of their occurrence reaches 84.4%. According to Vyrva, O.E. the incidence of bone chondroma ranges from 3 to 38% of cases. [1,2,3,26,27]. Pathology occurs in the form of various syndromes, most often multiple osteochondroma syndrome. All tumors of the musculoskeletal system, mainly appears in young people, in 80% of cases 20-30 years, with equal frequency of a female and male [2,25,26,27]. Analysis of the literature indicated that the authors are unanimous in the opinion that the most frequent sites of the tumor was small tubular bones of the hands [12]. Chondromas are borderline formations and have a potential malignancy and a pronounced ability to malignancy. Thus, according to various sources, up to 32% of cases with prolonged existence they were transformed into chondrosarcoma [4].According to summary data, relapses ranged from 1.4% to 19% in the treatment of patients with bone chondroma of various locations even at the performing of wide or segmental resections, which undoubtedly indicates a pronounced aggressiveness of these neoplasms. Moreover, some data indicates a decrease in the time between relapses with each reappearance of signs of the formation of a pathological focus [22]. Differential diagnosis of small bone tumors has certain difficulties, since it is necessary to conduct a thorough diagnosis both between the benign pathological processes themselves, and with malignant neoplasms of the bones, and with soft tissue diseases of the hand [7].The problem of treating of benign tumors and tumor-like diseases of the bones of the skeleton is very relevant and insufficiently developed [5,7,25]. The difficulties of surgical treatment of this pathology are primarily associated with the blast nature of the lesion, difficulties in early diagnosis, as well as the existence of various types of surgical treatment. All of them creates certain difficulties in choosing an appropriate method of surgical intervention. In addition, it is necessary to take into account their ability to malignancy with inadequate and untimely 9 surgical procedure [16,25].The improvement of the known methods of surgical treatment and replacement of bone defects and the choice of plastic materials used to replace bone defects for many years remains one of the main and urgent problems of oncorthopedics.In order to replace bone defects, use autografts, xenografts and allografts, artificial biomaterials even their combination is possible [13,23]. All known materials have certain advantages and disadvantages, and used strictly according to indications.The aim of the research was to study the results of surgical treatment of patients with chondroma of limb bones in the early and late postoperative period.
2. Materials and Methods
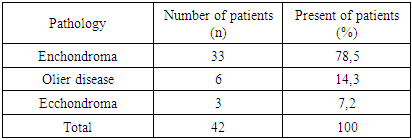
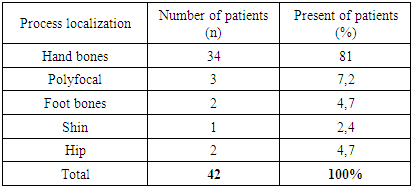
- 42 (24.8%) patients with chondroma of various shapes and localizations were treated. Among them, the enchondroma was 34 (81%), the ecchondroma was 3 (7%), Olier disease was 5 (11.9%) cases (table 1).
|
|
3. Results
- Clinical analysis of patients determined that in most cases, patients complained of pain - 42 cases, of which 6 cases had constant pain, in 8 cases it was occurred during physical exertion, in 5 cases with passive limb movement, in 23 cases the pain was episodic and not associated with physical activity and time of occurrence.At an external examination in 42 cases there was a thickening in 6 cases, deformation of the limb, and in 4 cases a pathological fracture was determined.The x-ray pattern differed from the process localization, while localization at the level of short tubular bones (foot brush) determined the characteristic pattern with the presence of a bleeding site — a bone defect with uneven thinning of the cortical layer at a given level, while the internal structure was heterogeneous with areas of compaction — “mottling”.When the process was localized in the area of the thigh and lower leg, the picture became less specific without a characteristic area of enlightenment with a definite shape; during the X-ray diffraction pattern, a section of a central location was often determined where alternation of areas of osteosclerosis and cartilage reconstruction was noted. As a rule, there were no signs of marked thinning of the cortical layer of the bone and thickening-expansion of the contours of the bone.To evaluate the results of treatment, in addition to the radiological and clinical signs of bone consolidation, a questionnaire was used to assess patients for episodes of relapse of pain, specifying their nature, intensity and time of occurrence, restoration of limb function, and the degree of fulfillment of household duties.As a result of the studies, 10 patients were identified as having episodic pain during the first week after the operation, in 28 patients the function was restored 7 days after the plaster cast was removed, and in 14 patients after 2 weeks.
4. Discussion
- Several of the most common methods of surgical treatment have been proposed in the world literature [23]. The main provisions of which are exoculating followed by cryo-, electro- or chemical treatment of the cavity and replacement of the defect with alloplastic material, or resection of the (marginal, segmental) bone with removal of the pathological focus and subsequent allo- or autoplasty of the defect [28], and in advanced cases offer endoprosthetics [9] or amputation of the limb. However, a large number of studies of surgical procedures, techniques for filling a bone defect, the use or rejection of auto or alloplasty proved that there was no single protocol for the treatment of this pathology, which allows us to continue this topic.In addition, the development of the Collapan implant, which is actively used in maxillofacial surgery and dentistry when filling small bone defects, is in time [10,11].In the reconstructive treatment of bone pathology of various origins the considerable interest is Collapan L. The implant can be used in the treatment of bone defects using the principles of minimally invasive surgery. This minimizes the volume and risk of surgery. This is especially relevantly for the localization of pathological foci in children, even near the growth zone or with damage to it, as well as in inaccessible areas of the skeleton.
5. Conclusions
- The study showed that the predominant number of benign tumors and tumor-like diseases of the limb bones was accounted for by bone chondroma (42 patients - 24%), in most cases, on enchondroma (33 cases - 81%). Often, pathology was found in the bones of the hand (78.8%).There are no signs to determine enchondroma. A preliminary diagnosis is made on the basis of the presence of a symptom complex such as periodic pain more often during physical exertion, a claviform thickening when localized in the area of the hand or forearm (which again is more often combined with pain), the presence of an area of enlightenment on the radiograph, as well as possible fractures on level of a thinned cortical layer.A distinctive feature of the diagnosis and treatment of tumor and tumor-like bone diseases is necessary for a mandatory multidisciplinary approach. This includes: collection of clinical data (patient complaints, clinical manifestations of the disease), adequate interpretation of data from radiation diagnostics and MRI studies, a careful assessment of the morphological picture and, if necessary, the use of other methods for making an accurate diagnosis.Evaluation of the treatment results has showed that the use of bone grafting with the use of Collapan L material improves the consolidation of the bone defect area in 82% of cases, which leads to early mobilization of the patient, shortening the rehabilitation and disability periods and ultimately improving treatment results.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML