-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(12): 990-994
doi:10.5923/j.ajmms.20201012.12
Received: Dec. 1, 2020; Accepted: Dec. 14, 2020; Published: Dec. 15, 2020

Comparative Assessment of the Effectiveness of the Use of Transtracheal Drainage and Bronchoscopic Debridement in the Treatment of Patients with Lung Abscesses Complicated by Bronchial Fistula
B. B. Safoev, A. K. Khasanov, N. R. Karshiyev, SH. G. Mirsoliev
Bukhara State Medical Institute, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The results of studies of 92 patients with lung abscesses complicated by bronchial fistula of various etiologies, who were treated in the purulent surgical department of the clinical base of Bukhara State Medical Institute in the period of 2010-2019, were analyzed. All patients, depending on the method of treatment, were divided into 2 groups: I - comparative group and II - main. The control group I consisted of 68 (73.9%) patients who received traditional conservative methods of treatment with the use of daily endobronchial sanitation of the bronchial lumen. In the 2nd -main group included 24 (26.1%) patients who, in addition to conservative treatment, underwent transtrachial drainage of a purulent focus with sanitation with antibacterial and thinning drugs. The analysis of the obtained results revealed that although transtrachial drainage of the purulent focus of the lung is a more effective method than the conservative method of treatment with the use of bronchoscopic lung debridement and has its drawbacks in the form of complications such as: in the form of suppuration of soft tissues in the area of microtrachestomyup to 12.5%, acute tracheobronchitis 20.8%, bronchospasm 8.3%, in 16.7% cases, there is an independent extradition of drainage in the bronchus, loss of microdrainage from the purulent cavity 8.3%.
Keywords: Transtracheal drainage, Bronchoscopic debridement, Lung abscess
Cite this paper: B. B. Safoev, A. K. Khasanov, N. R. Karshiyev, SH. G. Mirsoliev, Comparative Assessment of the Effectiveness of the Use of Transtracheal Drainage and Bronchoscopic Debridement in the Treatment of Patients with Lung Abscesses Complicated by Bronchial Fistula, American Journal of Medicine and Medical Sciences, Vol. 10 No. 12, 2020, pp. 990-994. doi: 10.5923/j.ajmms.20201012.12.
1. Introduction
- The authors’ researches show the percentage of development of pulmonary-pleural complications with lung abscesses ranges from 30 to 70%, and the incidence of gangrenous forms from 28 to 74% [2,4,6]. In general the mortality rate also remains high with various forms of purulent-necrotic process in the lungs from 12.7% to 77.8%. [3,7]The main treatment for an abscess is drainage. However, lung abscess is usually treated conservatively because drainage of the lung abscess is problematic. Drainage is considered only in cases of refractory lung abscess; in such cases, percutaneous lung drainage is usually used. Even when drainage is successful, percutaneous drainage is associated with the risk of complications such as pneumothorax and pleural culture; such complications occur in 16.1% of patients. [1]The main goal of interest is the article by scientists from the American Association of Bronchology and Interventional Pulmonology (AABIP) Raman Tuhina, Mcclelland Sarenthia, Bartter Thaddeus (2018) with the increase in the availability of methods for treating pleural effusion, including medical thoracoscopy (MT) and tunnel pleural catheter (TPC), in practice, there has been evolution Takaki Masahiro, Nobuaki Tsuyama, Eriko Iked (2019) A lung abscess is usually treated with long-term antibiotic therapy. Due to the lack of a safe and simple drainage technique, drainage is only used in special cases. [10,11]The experience of successful closure of persistent air leaks in patients with severe pleural empyema - the use of an endoscopic unilateral endobronchial valve is presented in the work of the authors of Schweigert. [12]Currie G.P., McKean M.E., Kerr K.M., Denison A.R. (2011) Over the past decade, the Endobronchial Ultrasound Transbronchial Aspiration Needle (EBUS-TBNA) has become one of the most exciting and innovative developments in respiratory medicine. This procedure allows for the selection of mediastinal lymph nodes and masses in both malignant and benign diseases and overcomes some of the disadvantages associated with mediastinoscopy and blind transbronchial aspiration with a needle. [9]The use of techniques that ensure the supply of antibacterial and other drugs to the pathological focus through the vascular bed presents great difficulties for their implementation, especially in the group of seriously ill patients and, in addition, do not solve many problems of local treatment. In this situation, it becomes necessary to carry out sanitation measures through the chest wall using the techniques of "minor pulmonary surgery". [5]Modern methods of treatment of abscesses and gangrene of the lungs are aimed at removing purulent contents from cavities by minimally invasive methods, endoscopic or transthoracic methods. The authors (Sizdikbaev М.К., Кurtukov V.А., Shoyxet Ya.N.) argue that bronchial destenosis is an effective method in complex treatment in patients with cicatricial stenosis of the bronchi against the background of purulent-inflammatory processes in the lungs, complicated by acute lung abscess and lung gangrene. [8]New technologies in the diagnosis and treatment of purulent-inflammatory lung diseases have made it possible over the past decades to slightly reduce the incidence, which is confirmed by existing literary publications, but the search for the most effective and low-traumatic treatment options is extremely relevant.Purpose of the study: to reveal the effectiveness and disadvantages of transtracheial drainage and sanitation in the treatment of patients with lung abscess complicated by bronchial fistula.
2. Materials and Methods
- Examined and treated of 92 patients with abscesses of mild bronchial fistula of various etiology were treated in the purulent surgical department of the clinical base of Bukhara State Medical Institute, the period from 2010 to 2019 were analyzed. All patients, depending on the method of treatment, were divided into 2 groups: I - comparison group and II - main. The control group I consisted of 68 (73.9%) patients who received traditional methods of treatment - conservative, antibacterial, general strengthening symptomatic treatment with the use of daily endobronchial sanitation of the bronchial lumen. II - the main group included 24 (26.1%) patients, for whom conservative treatment was supplemented with transtrachial drainage of a purulent focus with antibacterial and thinning drugs (trypsin, chymotrypsin).The effectiveness of the used and proposed clinical methods for the treatment of suppurative lung diseases was assessed by the duration of bronchopulmonary symptoms, general symptoms of intoxication, the dynamics of a decrease in the size of the purulent-destructive cavity, the value of the total bed-day.Methodology for sanitation bronchoscopy.Sanitation bronchoscopy was performed using a flexible bronchoscope, apparatus KARL SHTORS (Germany 2006). Bronchoscopic manipulation was performed in a sitting position of the patient. For the purpose of local anesthesia, immediately before the study, the nasal and oral cavity was treated with 10% Lidocaine spray. To reduce the gag reflex at the time of the introduction of the bronchoscope, the patient was recommended to breathe shallowly and as often as possible. The endoscope was introduced into the airway under visual control, gradually examining the underlying parts of the tracheobronchial tree from both sides. If necessary that the bronchial tree was sanitized along the way by aspiration. After sanitation from the aspiration material, a qualitative and quantitative bacteriological study was carried out, as well as the determination of the sensitivity to antibiotics of the identified microflord was carried out to determine the tactics of further antibiotic therapy.The technique of applying microtrachestomy.After appropriate premedication in the supine position of the patient, local anesthesia was performed on the anterior surface of the soft tissues of the trachea and along the midline of the neck. After three times skin treatment with 96% alcohol, 2 cm longitudinal incision of the skin and soft tissues was made. A puncture is performed between 2-3 cartilaginous rings of the trachea, a thin trocar, a tracheostomy is performed with the help of a microtroacor. Microdrainage is carried out through the lumen of the microtrocar with a lumen with a diameter of 2.0 mm. The microtroacor is removed, the microdrainage is fixed to the skin of the neck using polypropylene sutures, and an aseptic bandage is applied. Technique of drainage of the abscess cavity through tracheostomy.The position of the patient and the technique of anesthesia was carried out as noted above. A flexible bronchoscope, 5.2 mm in size, is passed through the nose, larynx and vocal cords under vosual control. The inflated microdrainage is captured through the microtracheostomy with the help of the bronchoscope spike and further, under strict visual control, is brought to the fistula gate and drainage is carried out by introducing the end of the microdrainage into the abscess cavity.
3. Results and Discussion
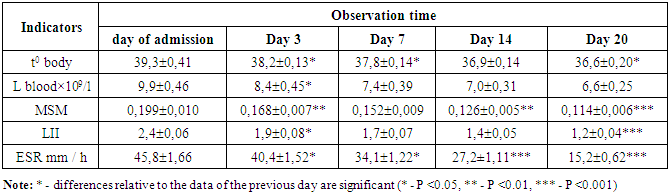
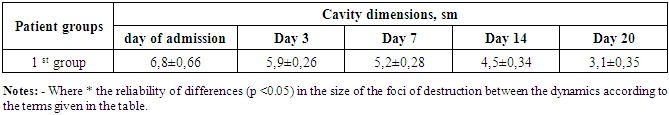
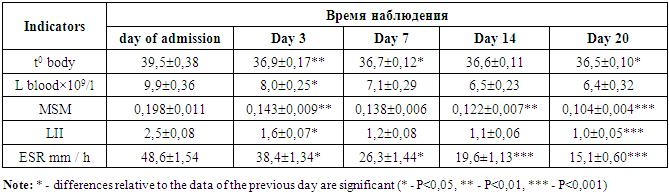
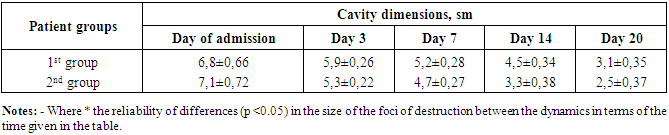
- In all patients, laboratory indicators of signs of endogenous intoxication from peripheral blood (hemoglobin concentration, leukocytosis, ESR, LII, LI, MSM), analysis of the duration of anti-inflammatory therapy, the qualitative composition of sputum micro flora, and the length of hospital stay were studied in all patients. At the time of admission and in the course of treatment, the patient's condition was assessed by clinical signs, according to laboratory and instrumental examination methods, as well as using X-ray research methods.Bacteriological studies in patients of group I were carried out from the lavage fluid of the bronchial tree, in group II the microflora was studied from catheter discharge from the abscess cavity. In most cases, 65 (70.6%) patients had pathogenic staphylococci (Staphylococcusaureus) inoculated. Pneumococcus was sown in 30 (32.6%) cases, E. coli was sown in 9 (9.8%) cases. It was inoculated in 5 (5.4%) cases, followed by streptococci (Streptococcus haemoliticus) in 13 (14.1%) cases. Pseudomonas aeruginosa (Pseudomonas aeruginosa) was inoculated in 8 (8.6%) patients.The analysis of the results of indicators of intoxication of the organism of patients with purulent lung diseases of the I group of comparison revealed the following changes (table 1). As can be seen from the table, on the first day of treatment, the body temperature of patients averaged 39.3±0.41°C. The content of blood leukocytes was on average 9.9±0.46 x 109 / l. The volume of medium molecules averaged 0.199 - 0.010 units. Similarly, an increase in LII and ESR was noted. On the third day of treatment, there was a slight decrease in body temperature indicators from 38.2±0.13 to 37.8,140.14, the number of blood leukocytes decreased on average to 8.4±0.45 × 109 / l. The volume of medium molecules averaged 0.168 ± 0.007 units. There was a decrease in LII and ESR indicators to 1.9 до0.08 and 40.4±1.52, respectively. By the seventh day of treatment, patients in the comparison group with purulent lung diseases retained a slight subfebrile condition (37.8 - 0.14°C). At the same time, according to all indicators of organism intoxication: L, MSM, LII and blood ESR, their further decrease was noted, that is, there was a tendency towards normalization –7,4±0,39×109; 0,152±0,009; 1,7±0,07; 34,1±1,22 respectively.
|
|
|
|
4. Conclusions
- Thus, our research revealed the following:With an abscess of the lung complicated by a bronchial fistula, St. aureus and Pneumococcus dominate from the pathogenic microflora.When using the method of treatment of bronchoscopic sanitation of patients with lung abscess, complications in the form of tracheobronchitis were noted up to 23.52%, hoarseness of the voice up to 2.94% of cases. The average duration of conservative treatment of patients is 18±1.5 days.The use of permanent catheterization of the purulent cavity and sanitation with the use of antibiotic therapy is an effective method in comparison with conservative therapy.When used in a complex for the treatment of endotracheobronchial catheterization of purulent cavities of the lung with sanitation and antibiotic therapy, it accelerates the normalization of all indicators of intoxication and improves the dynamics of reducing the size of purulent cavities by 2-3 days.The average duration of treatment for a lung abscess complicated by a bronchial fistula using transstrachial drainage is 14±1.8 days, which is 2-3 days ahead of the duration of treatment for a conservative method of treatment with the use of endobronchial sanitation.Although there are advantages of a positive effect compared to conservative treatment, patients with constant catheterization of purulent cavities have some complications of this method: in the form of suppuration of soft tissues in the area of microtrachestomy up to 12.5%, acute tracheobronchitis 20.8%, bronchospasm 8.3%, in 16, In 7% of cases, there is an independent extradition of the drainage in the bronchus (exit of the end of the catheter into the bronchus). Spontaneous loss of microdrainage is observed up to 8.3% of patients. That indicates the need to improve the methods of drainage of purulent lung cavities and which do not have the above disadvantages.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML