Rakhmonkulov E. Zh., Gaziev Z. T., V. E. Avakov, Shodiev M. B., Chaqqonov O’. A.
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The studies were carried out in a multidisciplinary TMA clinic in 40 geriatric patients with a comorbid background who were operated on under conditions of combined spinal-epidural anesthesia. 29 patients underwent total hip arthroplasty (THA), 11 - total knee arthroplasty (TKA). Inclusion criteria: elderly (65 to 75 years) and senile (76-90 years) age, and over 90 - long-livers, pain syndrome for more than one year, no contraindications for regional methods of anesthesia. For continuous monitoring of the vital functions of the patient, we used the resuscitation-surgical monitor YUM 300 (LLC Company UTAS Ukraine). For elderly and senile patients with a high risk of comorbidity, the technique of unilateral spinal and epidural anesthesia with low doses of intrathecal local anesthetic (5 mg 0.5% hyperbaric solution of bupivacaine with 20 μg fentanyl) and additional administration of low doses of bupivacaine into the epidural space 7, 5 mg is a safe method of anesthesia and allows you to achieve the proper sensory - motor block, which is necessary for the replacement of the joints of the lower extremities.
Keywords:
Spinal-epidural anesthesia, Central and peripheral hemodynamics, Arthroplasty of the joints of the lower extremities
Cite this paper: Rakhmonkulov E. Zh., Gaziev Z. T., V. E. Avakov, Shodiev M. B., Chaqqonov O’. A., Endoprosthetics of Large Joints of the Lower Extremities in Elderly and Senile People with a Pronounced Comorbid Background, American Journal of Medicine and Medical Sciences, Vol. 10 No. 12, 2020, pp. 946-950. doi: 10.5923/j.ajmms.20201012.04.
1. Introduction
Endoprosthetics of large joints is considered one of the most significant achievements in orthopedic surgery of the last century, but these surgical interventions remain one of the most traumatic [1]. Total arthroplasty of large joints is amenable to various methods of regional anesthesia that can improve patient outcomes. Several authors attempted to answer whether regional anesthesia reduced mortality, cardiovascular morbidity, deep vein thrombosis and pulmonary embolism, blood loss, duration of surgery, pain, opioid-related side effects, cognitive impairments, and length of stay. Many authors have tried to answer the question of whether regional anesthesia improved rehabilitation. [7,9,10].Regional anesthesia (spinal and epidural) is often preferred for lower extremity surgery to induce the necessary sensory block with minimal sympathetic exposure [3,5]. The aim of unilateral spinal anesthesia, which is usually used in orthopedic surgery, is to limit the spread of somatic and sympathetic blockade [6,8]. Limiting the spread of the block provides a number of clinical advantages, including significantly reduces the hemodynamic effect of spinal anesthesia [2,4] and is useful for elderly patients with low cardiac output, such as the elderly and senile patients we study.
2. Purpose of the Work
To assess the efficacy and safety of unilateral combined spinal-epidural anesthesia in orthopedic patients with a high comorbidity index during endoprosthetics of large joints of the lower extremities.
3. Material and Methods
Results of examination of elderly and senile patients who were treated in the department of orthopedics of large joints and hands of the multidisciplinary clinic of the Tashkent Medical Academy, with a pronounced background of comorbidity, who underwent primary endoprosthetics of the joints of the lower extremities. We examined 40 patients of geriatric age who were operated on under conditions of combined spinal-epidural anesthesia. 29 patients underwent total hip arthroplasty (THA), 11 - total knee arthroplasty (TKA). Inclusion criteria: elderly (65 to 75 years old) and senile (76-90 years old), and over 90 - long-livers, pain syndrome for more than one year, no contraindications for regional methods of anesthesia. Body mass index <40kg / m2. In 31.5% of the examined patients, physical status was assessed as class 1-2 according to ASA, in 68.5% of patients it corresponded to class 3-4.The exclusion criteria from the study were: refusal of the patient from this type of pain relief, age less than 65 years, body weight less than 50 kg, history of allergic reactions to local anesthetics used, coagulopathy, neurological and neuromuscular diseases, severe liver disease, renal failure, impossibility of cooperation with the patient. The patients were diagnosed with 2 to 6 concomitant diseases, among which IHD with chronic circulatory failure, atherosclerotic cardiosclerosis, hypertension of the 2nd degree with a high risk of developing cardiovascular and respiratory complications, arrhythmias prevailed.Two-level epidural catheterization was performed according to the standard technique; in the selected lumbar space L2 - L3, all tests were performed to verify the position of the epidural catheter in the adjacent space L3 - L4 in the direction opposite to the installed epidural catheter, and spinal puncture was performed. After receiving the cerebrospinal fluid, the required dose of anesthetic was administered. The spinal needle from the Espocan kit (B. Braun, made in Germany) was removed together with the mandrel, after which the epidural catheter was fixed. Local anesthetic (0.5% bupivacaine 5mg with 20 μg fentanyl) was injected intrathecally in small doses. Sedation during anesthesia was carried out by intravenous administration of 1% propofol solution at the rate of 0.3-1.1 mg / kg / h.The main hemodynamic parameters were recorded using the YUM 300 resuscitation surgical monitor. Registration of hemodynamic parameters intraoperatively was carried out at first every 5 min, then every 10 min until the end of the operation. Registration of analgesic and analgesimetry and a marker of stress - reactions (cortisol in the blood) was carried out at the following stages: I - initially on admission, II - after 6 hours, III - after 24 hours, IV - 48 hours after surgery. The degree of development of the sensory block was assessed by the pinprick test method on a 4-point scale (0 - normal sensitivity; 1 - reduced sensitivity; 2 - hypoesthesia; 3 - complete sensory block). The degree of development of the motor block was determined by the Bromage method on a 4-point scale (0 - normal motor function in the hip, knee, lower leg, and fingers; 1 - motor block in the thigh; 2 - motor block in the hip and knee; 3 - motor block in the thigh, knee and ankle). Before the onset of the development of the sensory block, the time was taken when the sensitivity in the knee and ankle was lost. The beginning of the development of the sensory block was taken as the time when sensitivity on the knee was lost, and for the end - the time when the sensitivity on the knee was restored. Before the onset of the development of the motor block, the time was recorded when the patient could not raise the leg at the hip, and at the end - the time when the motor function of the thigh muscles was restored.
4. Results and Discussion
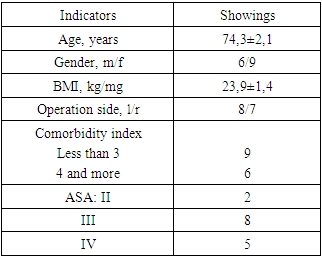
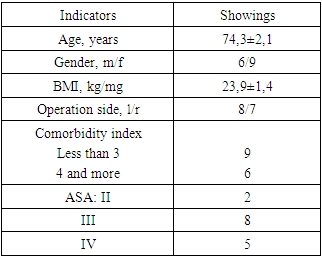
Table 1. Demographic and clinical characteristics of patients in this group (n = 40)
 |
| |
|
The peculiarity of patients in this group was elderly and senile age with a high comorbidity index (100%) and physical status ASA III and IV classes (86.6%).The most significant concomitant diseases in patients of this group were hypertension, coronary cardiosclerosis, myocardial infarction (2), chronic myocardial insufficiency, varicose veins of the lower extremities, severe pain syndrome.Table 2. Indicators of systemic hemodynamics in patients of this group at the stages of surgery and after it (n = 40)
 |
| |
|
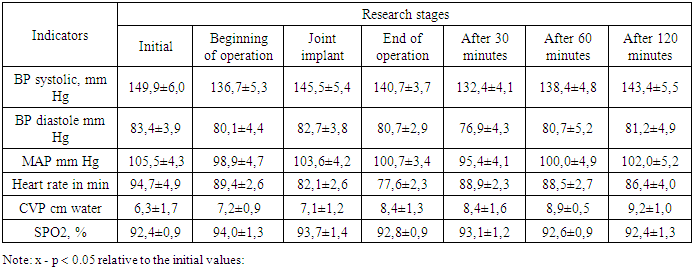
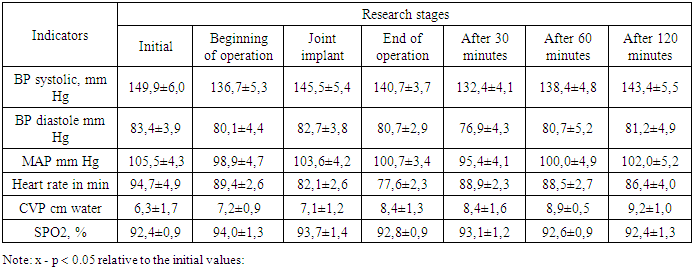
The presented data demonstrate rather stable indicators of systemic hemodynamics at all stages of the operation and the immediate postoperative period. There was only one episode of some decrease in blood pressure and systolic blood pressure by the beginning of the operation. However, this episode was short-lived and statistically insignificant, and this hypotension was only 8.8% lower than the baseline values of systolic blood pressure. Diastolic blood pressure and systolic blood pressure decreased by 4 and 6.3%, respectively (p> 0.05).The second episode of a decrease in blood pressure and systolic blood pressure was in response to the introduction of bupivacaine into the epidural space 30 minutes after the operative period for the purpose of pain relief. But here, too, the maximum decrease in blood pressure and systolic blood pressure was within 11.7%, 7.8% and 9.6%, respectively.As for heart rate, no episodes of severe tachycardia - or bradycardia - were recorded over the entire study period. During the operation, a tendency towards an increase in CVP was noted. However, the CVP indices remained within the physiological range, indicating an increase in the return of blood to the heart without an overload reaction on the part of the cardiovascular system. Pulse oximetry indicators slightly improved during the operation when oxygen was supplied through the mask, then returned to the initial values. We analyzed changes in blood pressure and systolic blood pressure immediately after administration of intrathecal 5 mg bupivacaine with 20 μg for 30 minutes.Table 3. Indicators of systemic hemodynamics after performing unilateral spinal - epidural anesthesia before the operation (n = 40)
 |
| |
|
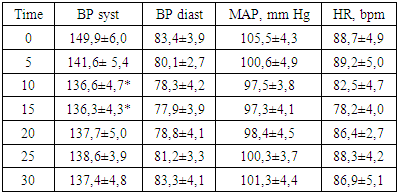
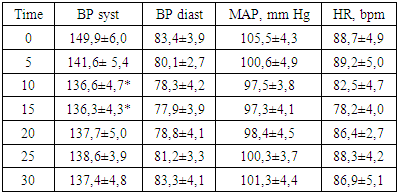
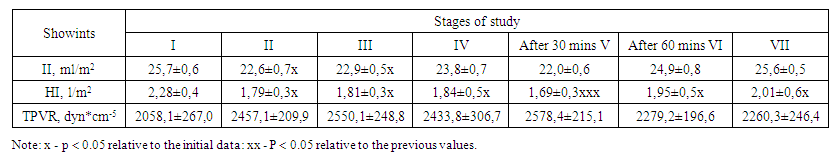
In general, hemodynamics is relatively stable. We see one episode of a moderate decrease in blood pressure and systolic blood pressure associated with the interthecal administration of bupivacaine with fentanyl, in response to which systolic, diastolic blood pressure and systolic blood pressure decreased by 9.3%, 6.6% and 4.7% at most by 10-15 minutes accordingly, the decrease in systolic blood pressure by 10-15 minutes was statistically significant, but it did not exceed 10%. As for the heart rate, its maximum decrease by 15 minutes was 11.9% relative to the 0 value (p < 0.05). We attributed this to the action of fentanyl. In no case did we note arterial hypotension exceeding 20%. The vascular load in this group was 1869.4 ± 278.4 ml.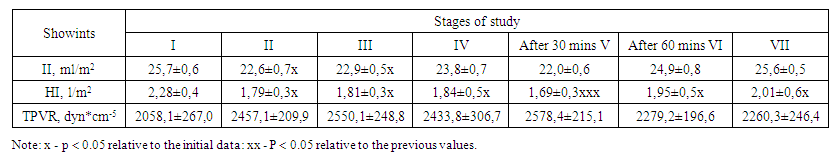 | Table 4. Dynamics of CH indicators at the stages of the operation and the postoperative period in the studied patients (n = 40) |
In patients, we register the initial hypodynamic circulatory regime with a decrease in one-time and minute cardiac output and relatively increased values of TPVR. And here we see two episodes of decrease in II and HI. One of them in the course of the operation - by the beginning of the operation, II and II decreased by 12.1% and 21.5%, respectively. In both cases, p < 0.05. In response to a decrease in these indicators, a tendency towards an increase in TPVR (by 20.1%) was noted. The second episode of a decrease in HI and II by 14.4% and 25.9%, respectively (p < 0.05) was associated with complaints of patients about pain in the postoperative wound before the introduction of bupivacaine into the epidural space, the systemic vascular resistance during this period increased by 21.9% (p < 0.05). The initial values of TPVR exceeded the proper values of this indicator by 5.5%, indicating the prevalence of spastic processes in the system of low blood pressure due to the overwhelming influence of the sympathetic nervous system. This was also evidenced by the Kerdo vegetative index and the level of cortisol in the blood at stages I and V of the study.Table 5. Indicators of sensory and motor blocks and total consumption of bupivacaine and fentanyl in the perioperative period in patients (n = 40)
 |
| |
|
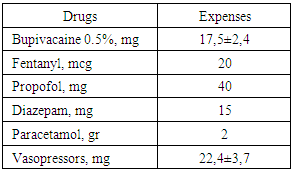
Analyzing the presented values, it can be indicated that with unilateral spinal-epidural anesthesia with low doses (5 mg bupivacaine), the timing of the onset of blocks and the time to reach the sensory block to the Th10 level are slightly lengthened. Noteworthy is the decrease in the duration of the sensory block and its regression time relative to the same indicators in the previous group by 14.5% and 19.4%, respectively, which we associated exclusively with a decrease in the dose of bupivacaine, since the dosage of intrathecal administration of an adjuvant in both groups was the same (20 mcg fentanyl).As for the motor block, its duration was sufficient for such operations, and it was regulated by the introduction of bupivacaine into the epidural space without opioids and other adjuvants. Sensory blockade of the operated limb up to the zones of innervation of the hip and knee joints (Th10 - Th11 and L5 - L4, respectively) was achieved in 100% of cases within 30 - 35 min with unilateral spinal epidural anesthesia.By 30–35 minutes after the beginning of the unilateral anesthesia procedure, all patients developed a motor block of the pathological limb, towards which the epidural catheter was oriented. Moreover, the motor blockade was 3-4 points on the Bromage scale.By the beginning of the operation, in one patient in this group (6.6%), we registered a motor blockade (1 - 2 points) of the contralateral limb. The development of motor blockade in a healthy leg in 2 patients in the postoperative period could be evidence of a central displacement of the tip of the epidural catheter. At the same time, a decrease in the dose of the rate of injection of bupivacaine into the epidural space led to the termination of the motor block of the contralateral limb.All patients underwent prophylaxis of thrombotic complications, perioperative prophylaxis of surgical infection in accordance with the protocols existing in the clinic.We did not observe intraoperative complications of patients. In one patient (6.6%) post-puncture syndrome (headache, nausea, vomiting, dizziness) was registered 24 - 26 hours after the operation, which was associated with the leakage of cerebrospinal fluid through a puncture of the dura mater. Double intravenous drip injection of 10% caffeine (200-300 mg each) and filling of the epidural space with autologous blood stopped this syndrome. One patient had pruritus and urinary retention. Another patient noted moderate back pain, which resolved on its own.Table 6. Total consumption of drugs in the perioperative period for each patient operated on under unilateral spinal epidural anesthesia (n = 40)
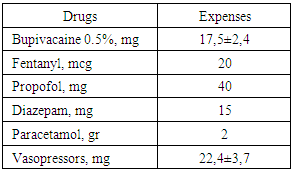 |
| |
|
From the presented data, it can be concluded that this method of analgesia has a significant opioid-saving nature, which is extremely important for geriatric patients undergoing such voluminous and traumatic interventions as large orthopedic operations.Summarizing the analysis, it should be noted that unilateral and spinal and epidural analgesia with small doses of intrathecal local anesthetic (0.5% bupivacaine 5mg with 20 μg fentanyl) and additional unilateral epidural analgesia is a new, safe and effective method of pain relief for lower limb arthroplasty.Despite some laboriousness of the method, hemodynamic stability, low doses of local anesthetic opiates, a limited number of complications and side effects, this method of analgesia is exclusively indicated in geriatric patients with a high degree of comorbidity.A mixture of 5 mg 0.5% bupivacaine with 20 μg fentanyl, administered intrathecally according to this technique, caused good sensory and motor blocks, and the technique helped to limit the spread of somatic and sympathetic blockade (diseased limb).Unilateral introduction of an epidural catheter allows for a predominantly unilateral distribution of local anesthetic in the epidural space with the development of selective sensory and motor blockade.Unilateral epidural anesthesia together with unilateral SA provide adequate protection of the patient from operational stress and effective postoperative pain relief in geriatric patients with arthroplasty of the lower limb joints.
5. Conclusions
1. For elderly and senile patients with a high risk of comorbidity, the technique of unilateral spinal and epidural anesthesia with low doses of intrathecal injected local anesthetic (5 mg 0.5% hyperbaric solution of bupivacaine with 20 μg fentanyl) and additional administration of low doses of bupivacaine into the epidural space 7, 5 mg is a safe method of anesthesia.2. Unilateral spinal-epidural anesthesia is characterized by hemodynamic stability, adequate protection from operational stress, a small number of complications and side effects, and an opioid-saving effect. It should find a niche for its use in elderly and senile people with a high comorbidity index and physical. status (II - IV) ASA.3. For the first time, a technique has been developed for unilateral spinal - epidural anesthesia with low doses of local anesthetic administered both intrathecally and epidurally, which is applicable to elderly and senile people during TEX and THA operations.
References
| [1] | Bessonov S.V. Features of anesthetic management of endoprosthetics of large joints of the lower extremities. S.V. Bessonov, A.K. Orletsky, V.L. Kassil. Bulletin of Traumvtology and Orthopedics. N.N Priorova. 2005; 1: 85-90. |
| [2] | Zagrekov V.I. Influence of the method of anesthesia on blood loss in hip arthroplasty. V.I. Zagrekov (and others). Medical almanac. 2010; 2 (11); 210-212. |
| [3] | Obukhov V.A. The choice of the method of pain relief for hip joint prosthetics. VA Obukhov et al. XI. In Seros. Cong. Of anesthesiologists and resuscitators: collection of articles. materials. SPb., 2008; 235-236. |
| [4] | Ovechkin A.M. Prevention of postoperative pain syndrome: pathogenetic basis and clinical application: abstract of thesis. Dr. med. sciences. Ovechkin A.M. 2000; 43 p. |
| [5] | Plakhotina E.N. Perioperative treatment of elderly and senile patients with degenerative-dystrophic diseases (experimental-clinical research. Abstract of thesis ... Dr. med. Sciences: 14.00.37. Plakhotina EN SPbMAPO. SPb 2009. 42 p.67. |
| [6] | Chakladar A, White SM. Cost estimates of spinal versus general anesthesia for fractured neck of femur surgery. Anasthesia 2010 aug 65 (8): 810-4 epub 2010 may 27/. |
| [7] | Matteu T. Continuous femoral nerve block: varying local anesthetic delivery method (bolus versus basal) to minimize quadriceps motor block while maintaining sensory block / T. Matteu (et al). Anesth 2011: 115 (4): 774-781. |
| [8] | Pugely AJ, Martin CT, Gao y, Mendozza-Lattes S, Callaghan JJ. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Joint Surg Am. 2013 feb 6:95 (3): 193-9 Epub 2012 dec 28. |
| [9] | Scarecrows AJ, Martin KT, Gao J, Mendozza-Lattes S, Callaghan JJ. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Joint Surg Am. 2013 feb 6: 95 (3): 193-9 Epub 2012 dec 28th (Pubmed) (goole scholar). |
| [10] | Sheferf R, Eberherda M (2009) Anesthesiology. Moscow: Geotar-Media. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML