-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(11): 914-918
doi:10.5923/j.ajmms.20201011.18
Received: Oct. 17, 2020; Accepted: Nov. 18, 2020; Published: Nov. 28, 2020

Endoscopic Hemostasis at Gastroduodenal Bleeding of Ulcer Etiology in Children
Kh. A. Akilov, N. T. Urmanov, M. A. Khoshimov, A. B. Eshmuradov
Republican Research Center of Emergency Medicine, Tashkent Institute of Post-Education Doctors, Tashkent, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

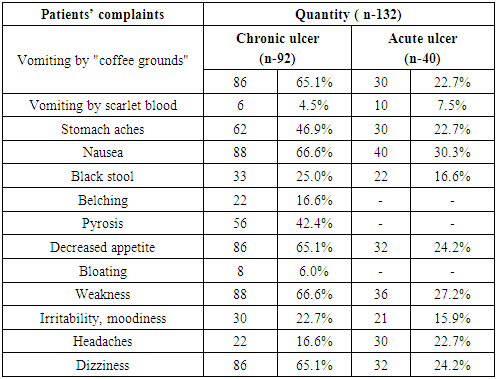
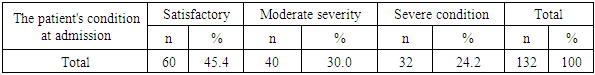
The aim of the research was to study the endoscopic hemostasis results at acute bleedings from gastro-duodenal ulcers in children. The study is based on the analysis of treatment results of 132 children with bleedings from acute and chronic gastric and duodenal ulcers, who were hospitalized to the Department of Emergency Pediatric Surgery of the Republican Research Center of Emergency Medicine from 2005 to 2019. There were 86 boys (65.1%) and 46 (34.9%) girls aged from 9 months to 18 years. Chronic forms of the disease were revealed in 92 (69.6%) cases, the remaining 40 (30.4%) cases were acute forms. Gastric ulcers were found in 9 (6.8%) patients and 6 (4.5%) of them had acute forms of the disease. In 123 (93.1%) patients ulcers were located in the duodenum: acute forms of ulcers were observed in 34 (25.7%) cases and in 89 (67.4%) - chronic ones. Patients with gastrointestinal bleeding were evaluated for their clinical condition upon admission to the clinic and the severity of blood loss was determined. The evaluation of the general condition severity in patients with gastroduodenal ulcerative bleeding was carried out according to the classification of A.I. Gorbashko (1986).Experience shows that the diagnostics should be complex in cases of gastric and duodenal ulcers complicated by bleeding. In this case, the endoscopic research method is of particular importance. Depending on the localization of the bleeding source and its intensity, a differentiated approach should be applied to the choice of endoscopic hemostasis method. The use of the combined method of chipping in combination with argon-plasma coagulation in most cases allows achieving stable hemostasis with ongoing intense bleeding.
Keywords: Duodenal ulcer, Endoscopic hemostasis, Gastroduodenal ulcer bleeding, Peptic ulcer disease
Cite this paper: Kh. A. Akilov, N. T. Urmanov, M. A. Khoshimov, A. B. Eshmuradov, Endoscopic Hemostasis at Gastroduodenal Bleeding of Ulcer Etiology in Children, American Journal of Medicine and Medical Sciences, Vol. 10 No. 11, 2020, pp. 914-918. doi: 10.5923/j.ajmms.20201011.18.
Article Outline
1. Introduction
- Gastroduodenal ulcer bleeding (GDUB) is one of the most difficult clinical problems in abdominal surgery associated with a high mortality rate and requiring urgent hospitalization [1-3]. Despite the progress of medical science and clinical practice and more than a century history of discussion of the issue, the problem of therapeutic tactics in patients with GDUB remains one of the most actual issues of modern emergency surgery [4-5].The decrease in the frequency of surgical operations for gastroduodenal ulcer bleeding is currently, first of all, associated with the use of such methods as antacid, anti-Helicobacter ones. But, in spite of this, the frequency of surgeries is still about 33% of all interventions on the stomach and duodenum, and 87.2% of them are emergency and performed in high-risk patients [6-7]. Surgery for GDUB often remains the last and most effective treatment [8-10]. Over the past decades, GDUB surgery has undergone impressive changes and today has been limited mainly by interventions due to severe complications [11-12]. As a result, further searches towards the development of organ-saving methods of surgical intervention of ulcerative gastroduodenal bleedings are justified.Organ-saving surgeries with vagotomy which are of primary importance in the treatment of gastroduodenal bleeding should be considered the modern stage of the surgical treatment of gastroduodenal bleedings [13-14].There is a tendency for many surgeons to refuse radical interventions in favor of organ-saving surgeries. New technologies allow to use a low-traumatic version of these operations. The methodology and technique of organ-saving surgeries continues to be improved. Thus, the widespread introduction of modern endoscopic technology into clinical practice which allows stopping bleeding, as well as the use of minimally invasive interventions led to a change in the tactics of treating patients with ulcerative gastroduodenal bleeding and to differentiated determination of indications for surgery [15-16]. Currently, endoscopy has a number of hemostasis methods, different in their effectiveness, reliability, safety and cost. Endoscopic hemostasis (EH) is sometimes the only method of local action on the source of bleeding in case of intolerance to surgery. However, despite the availability of many modern methods of endoscopic hemostasis, they are not always effective and often lead to recurrent bleeding. It is known that EH is effective only in some patients, and the period of its stability is calculated by hours [17-18].
2. The Aim
- The aim of the research was to study the endoscopic hemostasis results at acute bleedings from gastro-duodenal ulcers in children.
3. Material and Methods
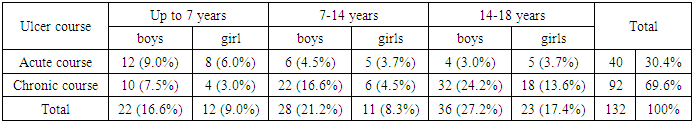
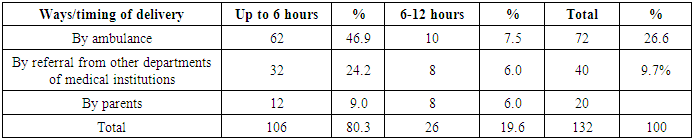
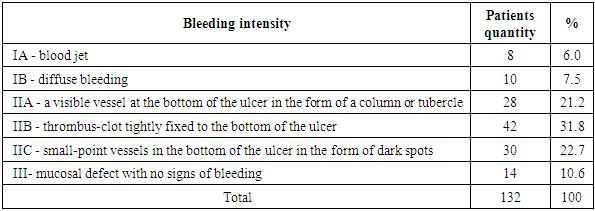
- The study is based on the analysis of treatment results of 132 children with bleedings from acute and chronic gastric and duodenal ulcers who were hospitalized to the Department of Emergency Pediatric Surgery of the Republican Research Center of Emergency Medicine (RRCEM) from 2005 to 2019. There were 86 boys (65.1%) and 46 (34.9%) girls aged from 9 months to 18 years. All children were divided into 2 groups on the basis of clinical-anamnestic and endoscopic data. The first group included 40 (30.4%) children with acute ulcers complicated by bleeding. The second group consisted of 92 (69.6%) children with chronic forms of the disease complicated by bleeding. The average age was 8.6 ± 1.3 years in the first group and 8.8 ± 1.4 years in the main group. Gastric ulcers were found in 9 (6.8%) patients and 6 (4.5%) of them had acute forms of the disease. In 123 (93.1%) patients ulcers were located in the duodenum: acute forms of ulcers were observed in 34 (25.7%) cases and in 89 (67.4%) - chronic ones.The frequency of bleeding from acute ulcers was most common in young children. In children with a chronic course it increased with age, while boys prevailed with a peak detection rate at the age of 14-18 years. Girls significantly less suffered from this pathology: in contrast to the first group, the peak detection rate of peptic ulcer disease in girls of the second group was in the age rate from 11 to 14 years. The data obtained reflect the general patterns of the prevalence of duodenal ulcer depending on age and gender (Tab. 1).
|
|
|
|
|
4. Results and Discussion
- Currently, endoscopic hemostasis methods play an important role in the treatment of patients with gastroduodenal bleeding. The introduction of endogemostasis into clinical practice helped to avoid emergency surgeries in many cases, allowing a fundamentally different look at the need for surgical treatment of many patients with gastroduodenal bleeding, at least allowing a delayed operation after appropriate preparation of the patient. More than 50 methods of endoscopic stopping of bleeding have been proposed, new or existing methods of influencing to the source of bleeding in gastroduodenal ulcers appear almost every year. We use injection, electrocautery and argon-plasma methods of endohemostasis in our Center. The infiltration method remains the most common method of endoscopic hemostasis. There are no absolute contraindications. The mechanism of infiltration hemostasis consists of hydraulic compression of blood vessels, vascular spasm, increased local thrombosis and sclerosis in the immediate vicinity of the hemorrhage source as a result of perifocal injection of drugs. We used 70% ethyl alcohol, 0.1% adrenaline solution for infiltration hemostasis. Electrocoagulation is one of the most widely used methods of endohemostasis. For electrocoogulation, the transformation of high-quality electric current (500 kHz-2 MHz) energy into thermal energy is used at the point where the electrical circuit is closed when the electrodes are in contact with biological tissue. The most formidable complication of this method is the perforation of a hollow organ wall as a result of tissue combustion with the formation of a black scab. In this connection, argon-plasma coagulation (APC) has been widely used since 2012. The main advantages of APC over electrocoagulation are considered to be non-contact exposure and the absence of welding of the coagulation scab to the electrode during APC.Eight (6.0%) patients were admitted to the hospital with ongoing jet arterial bleeding from an ulcer (F-1A). For this category of patients, we used the combined forms of endohemostasis: injections + argon plasma coagulation. Temporary hemostasis was achieved in 7 (5.3%) cases. In one case this combination was ineffective, and therefore a laparotomy, duodenotomy with suturing of a bleeding duodenal ulcer was performed urgently. In 2 (2.7%) cases with active arterial bleeding the cause was a stress duodenal ulcer, which developed in one case against the background of extensive thermal burns of the body by 90%, and in the second case - against the background of acute liver failure. The combined method of endohemostasis was also applied to these patients with achieving temporary hemostasis. Despite the intensive therapy, these patients had repeated episodes of bleeding which was the reason for the forced surgical intervention for life reasons: laparotomy, duodenotomy with suturing of the ulcer. The postoperative period in a child with an extensive burn of the body was ended by lethal outcome.In 10 (7.5%) patients diffuse bleeding had a venous nature (F-1B). Using the combined form of endohemostasis (injection + electrocoagulation) it was possible to achieve primary arrest of bleeding in all patients. There was a relapse of bleeding in 3 (3.2%) cases within first 6 hours and it was a reason for repeated endohemostasis. Due to the repeated relapse of bleeding in 2 (2.7%) cases with chronic forms of duodenal ulcers, children were operated on in a delayed emergency. Since these patients had combined complications (bleeding with stenosis of the outlet from the stomach), they were performed laparotomy, gastric resection according to Billroth-I, modified by L.G. Khachiev. In the remaining 5 (5.4%) cases children were operated on after stabilization of the state: the indication for surgery was frequent relapses of peptic ulcer disease, which were not amenable to conservative therapy for three years. All patients were performed gastric resection according to Billroth-I modified by L.G. Khachiev. The presence of a thrombosed vessel (F-2A) in the ulcer was initially diagnosed in 28 (21.2%) patients. In order to strengthen hemostasis in the ulcer, all patients were performed endoscopic hemostasis by the method of alcohol injection and a complete hemostasis was achieved in 100% of cases. In this type of patients surgeries were performed in 5 (3.8%) cases with chronic forms of duodenal ulcers. In this category of patients, operations were performed in 5 (3.8%) cases with chronic forms of duodenal ulcers. This group of patients were also performed gastric resection according to Billroth-I modified by L.G. Khachiev. F-2B bleeding occurred in 42 (31.8%) cases. In all cases, endoscopic hemostasis was also performed by the method of alcohol injection. Control endoscopy, performed one day later, revealed small-puncture thrombi at the bottom of the ulcer in all patients (F-2C). The presence of small-point thrombi in the ulcer according to F-2C was observed in 30 (22.7%) patients. They were not performed endoscopic hemostasis. On control endoscopy, three days later, in 100% of cases we observed that the bottom of the ulcer was completely cleared and covered with fibrin (F-3). Sixteen patients with Forrest-3 made up 17.3% of the total admissions. Control examination after three days revealed a clear bottom of the ulcer in 98% of cases. In 2% of cases small punctate thrombi appeared at the bottom of the ulcer. There were no signs of recurrent bleeding.
5. Conclusions
- Thus, experience shows that in case of gastric and duodenal ulcers complicated by bleeding, the diagnostics should be comprehensive. In this case, the endoscopic research method is of particular importance.Depending on the localization of bleeding source and its intensity, a differentiated approach should be applied to the choice of endoscopic hemostasis method. The use of the combined method of injection in combination with argon-plasma coagulation in most cases allows achieving stable hemostasis during ongoing intense bleeding.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML