-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(11): 911-913
doi:10.5923/j.ajmms.20201011.17
Received: Sep. 29, 2020; Accepted: Nov. 4, 2020; Published: Nov. 28, 2020

Method of Improving Vasopressor Therapy for Acute Myocardic Infarction Complied with Cardiogenic Shock
Pulatova Sh. Kh.
Basic Doctoral Student of Bukhara State Medical Institute Named after Abu Ali Ibn Sina Ministry of Health of Uzbekistan
Correspondence to: Pulatova Sh. Kh., Basic Doctoral Student of Bukhara State Medical Institute Named after Abu Ali Ibn Sina Ministry of Health of Uzbekistan.
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article is devoted to the improvement of vasopressor therapy used in the treatment of patients with acute myocardial infarction complicated by cardiogenic shock. Today, despite the development of the medical field and the rapid growth of the pharmaceutical industry, one of the most serious complications of acute myocardial infarction is mortality after cardiogenic shock. Moderate acute myocardial infarction (OMI) is complicated by cardiogenic shock (CS) in 20-30% of cases. It is known from scientific sources that the death rate from KS has reached 30-40%. This is now one of the global challenges of the health care system.
Keywords: Cardiogenic shock, Vasopressor, Thrombolytic therapy (TLT), Antiaggregants
Cite this paper: Pulatova Sh. Kh., Method of Improving Vasopressor Therapy for Acute Myocardic Infarction Complied with Cardiogenic Shock, American Journal of Medicine and Medical Sciences, Vol. 10 No. 11, 2020, pp. 911-913. doi: 10.5923/j.ajmms.20201011.17.
Article Outline
1. Introduction
- It is known that acute myocardial infarction is one of the most serious pathologies in coronary heart disease, which in turn leads to a sharp decrease in work capacity and many fatal consequences. In most cases, lethal consequences are caused by myocardial infarction with cardiogenic shock.It is known that shock is the death of these cells. Numerous literatures show that in recent years the incidence of CK has decreased and accounts for 5-9% of OMI.Numerous studies have shown that achieving these results is not surprising given the widespread use of thrombolytic therapy (TLT) in medicine, surgical procedures, and the correct implementation of treatment tactics in this group of patients.However, the lethal consequences from the US remain high, having been found to be 40-90% today. Effective treatment of these patients still remains one of the major and challenging problems of the health care system.Le Dran first coined the term "shock" and its clinical significance in 1743, describing shock as a "post-addictive steady state." can develop.Throughout the history of the study of shock, with its descriptions and classifications in many literatures, Moore described it as follows: "The greater the cause of death, the more types of shock there are."Therefore, shock treatment should focus on the choice of vasopressor, infusion therapies, and organ preservation. Therefore, the correct choice of vasopressor therapy in the treatment of shock dramatically reduces mortality.Initiation of dopamine (equivalent to norepinephrine) in the treatment of shock affects dopamine receptors, α and breceptors, improving blood flow to internal organs and preventing cell death.The presented data show the importance of vasopressor therapy in the treatment of CK, its clinical and dermographic changes and its impact on mortality. OMI is intended to improve the treatment of CKD.The aim of this study was to improve the treatment of cardiogenic shock from vasopressor therapy by comparative diagnosis of norepinephrine and dopamine.
2. Materials and Methods of Research
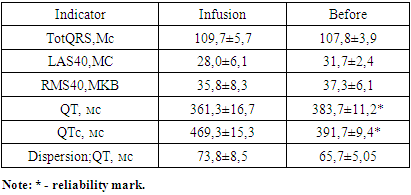
- In order to achieve this goal, 78 patients treated with the diagnosis of "acute myocardial infarction complicated by cardiogenic shock" in the Bukhara branch of the RCST in 2018-2020 were involved in research.All patients were prescribed additional vasopressor therapy in addition to standard therapy (anticoagulants, antiaggregants, nitrates, glucocorticosteroids, diuretics, and thrombolytics as directed).In order to evaluate the effectiveness of norepinephrine and dopamine, patients were divided into 2 groups: 30 patients in group 1 were prescribed norepinephrine (Norepin 0.2% -8mg 4.0 ml) intravenously in a 3-5 mcg / kg / min infusion for 24 hours); In 48 patients in group 2, dopamine (dopamine 40mg / ml- 4% -5.0ml) was administered intravenously at a dose of 2–10 μg / kg / min for 24 h, starting with arterial pressure (A / B), ventricular systole (SVS), under pulse control.The dose of medication is selected according to the instructions of the treating physician. Hemodynamics were not compared when doses were selected.All patients were asked to complete a general clinical analysis, i.e., general condition at the time of admission and post-infusion status in all patients, in which symptoms of acute heart failure were assessed on a H7 score system, i.e., +3 very good, +2 relatively good, + 1 is partially good, 0 is completely unchanged, -1 is worse, -2 is significantly worse, - 1 is very bad.Biochemical analysis of blood showed lipid spectrum (LPNP, LPVP, triglycerides, total cholesterol), glucose, urea, creatinine in all patients. and renal pelvic filtration rate in all patients was calculated based on the MDRD formula in ml / min / 1.73m2:- for men 186 x (amount [mg / dl] 1,154) x (age);- for women 186 x (creatinine in the blood [mg / dl]) x (age) x 0.742.Renal insufficiency Kidney ball filtration rate <90ml / min / 1.73m2 was calculated.Ultrasound examination of the heart (EXOKG), Doppler examination in M- and V-mode. The fraction of the left ventricle of the heart is FV LJ, and its final systolic measurement (KSR) and final diastolic measurement (KDR).Myocardial contractility (norm, hypokinesia, akinesia, dyskinesia) was observed. In evaluating the effectiveness of therapy, EXOKG was performed on day 1 of therapy and on the day therapy was discontinued.Electrocardiography was performed in 12 standard networks.To assess the arrhythmogenic effects of the drugs, Holter monitoring was performed 1 and after infusion cessation.QT interval dispersion was considered the norm to be up to 60 ms in standard 12 networks between maximum and minimum QT intervals. The monitor calculated supraventricular paraxysmal extrasystoles, the maximum frequency of ventricular extrasystoles, the maximum frequency of ventricular tachycardia.The diagnosis was based on the Killip scale, based on clinical and ECG signs.
3. Results and Discussion
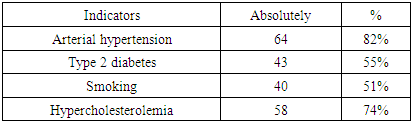
- The mean age of the 78 patients involved in the study was 66 ± 4.5 years. Of these, 52 are male and 26 are female.Of these, 64 (82%) cases had a history of arterial hypertension, type 2 diabetes mellitus 43 (55%), harmful habits - smoking 40 (51%), hypercholesterolemia 58 (74%) cases (Table 1). All patients were monitored during treatment. The mean day spent in the hospital was 10 ± 3.4 days.
|
|
4. Conclusions
- 1. In acute myocardial infarction complicated by cardiogenic shock, maximum vasopressor therapy should be selected for immediate relief of shock. This, in turn, prevents the recording of deaths and the increase in disability among patients.2. Complications of acute myocardial infarction with cardiogenic shock are more common in the elderly due to organic changes, in patients with low heart rate, in patients with a sharp decrease in renal function.3. The importance of vasopressor therapy in acute myocardial infarction is important because it provides the necessary hypoperfusion in the tissues. Dopamine can cause high blood pressure as well as tachycardia, which further increases the myocardium’s need for oxygen, deepening the ischemia. Norepinephrine does not affect IUDs and in turn raises blood pressure, making it superior to dopamine.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML