-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(11): 894-897
doi:10.5923/j.ajmms.20201011.12
Received: Oct. 17, 2020; Accepted: Nov. 5, 2020; Published: Nov. 15, 2020

Effect of Flavanoids on Kidney Function in Patients with Chronic Kidney Disease before Dialysis
Munavvarov Burkhonjon Abdujalilovich, Sabirov Maksud Atabayevich
Department of Therapy Subjects №2, Tashkent State Dental Institute, Tashkent, Uzbekistan
Correspondence to: Sabirov Maksud Atabayevich, Department of Therapy Subjects №2, Tashkent State Dental Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Chronic renal failure is a disease resulting in severe uremic intoxication. In this study, the hypoazotemic efficacy of the domestically produced flavanoid Nephrocizine in patients with chronic kidney disease was studied. The results show, that in the group of patients who took the drug Nephrocizine provided a significant decrease in the levels of urea, creatinine and an increase in the glomerular filtration rate unlike the control group.
Keywords: Chronic kidney disease, Glomerular filtration rates, Flavanoids, Nephrocizine
Cite this paper: Munavvarov Burkhonjon Abdujalilovich, Sabirov Maksud Atabayevich, Effect of Flavanoids on Kidney Function in Patients with Chronic Kidney Disease before Dialysis, American Journal of Medicine and Medical Sciences, Vol. 10 No. 11, 2020, pp. 894-897. doi: 10.5923/j.ajmms.20201011.12.
Article Outline
1. Introduction
- Improving the quality of life and overall survival of patients with chronic renal failure (CRF), the prevalence of which is steadily increasing in the world, are the urgent problems of modern nephrology [1,2]. According to the results of epidemiological studies, patients with a glomerular filtration rate (GFR) less than 60 ml / min constitute 5% of the total adult population in the world [9,10,11].The increase in the prevalence of CRF is explained not only by an increase in the number of patients with primary renal pathology, but also by diabetes mellitus, obesity, aging (long life expectancy) and damage to individual renal vessels [4,5,6]. Kidney disease is more severe when multiple risk factors are present. Over the past 15-20 years, the number of patients receiving renal replacement therapy has increased more than 4-5 times [7,8].In the early stages of the occurring of renal failure, there are no symptoms of renal dysfunction. A further decrease in the loss of functioning nephrons (up to 30% of the norm) leads to a more expressed impairment of renal function - an increase in the concentration of nitrogen metabolites (urea, creatinine), electrolyte imbalance, anemia, and so on. [12,13]. From the literature it can be seen that in cases of hyperazotemia, bioflavonoids made from plant materials are effective drugs, of which flavonoids are the drugs of choice for complex use in the treatment of renal failure (the most widely used) [6,7]. Nephrocizine, a drug belonging to the group of flavonoids, was developed as a substance at the Institute of Plant Chemistry of the Republic of Uzbekistan (reg No. 2 of 12.06.2009). The most valuable property of flavonoids is their excretion of urea and other nitrogenous products from the blood, which is extremely important for chronic kidney diseases of various etiologies. Thus, we considered it necessary to monitor the effect of Nephrocizine on renal function parameters and evaluate its hypoazotemic efficacy for the complex treatment of CKD patients in the pre-dialysis period.
2. Purpose of the Research
- The purpose of the research is to study the effect of Nephrocizine on renal function indicators and evaluate its hypoazotemic efficacy in patients with chronic kidney disease in pre-dialysis stage.
3. Materials and Methods
- For the study, 123 patients were selected with CKD with of nephropathy of various origins (GFR 15-59 ml / min / m2), who were treated at the Department of Nephrology of the Tashkent Medical Academy. The age of the patients ranged from 19 to 50 years (averagely 38.63 ± 1.09). The duration of the disease ranged from 5 to 10 years, with an average of 7.8 ± 2.3 years. All patients were randomly divided into 4 groups: 1 A (n-32), 1 B (n-31) (GFR 30 - 59 ml / min) and 2 A (n-30), 2 B (n-30) (GFR 15 - 29 ml / min): group 1 A and 2 A of the patient received traditional treatment in accordance with the recommendations of international standards; group 1 B and 2 B patients, in addition to traditional treatment in accordance with international treatment standards, received Nephrocizine at a dose of 300 mg / day (50 mg in a tablet, 1 tablets 2 times a day, for 3 months). At the time of inclusion in the study, all patients had a documented diagnosis of stage III or IV CKD based on the eGFR determined from the serum creatinine concentration using the CKD-EPI formulas (2009) modified in 2011 (an on-line calculator was used on the website http://nefrosovet.ru/). At the beginning of treatment, after 10 days, after 1 and 3 months, all patients were determined by the level of urea and creatinine, as well as GFR. The results were statistically analyzed.
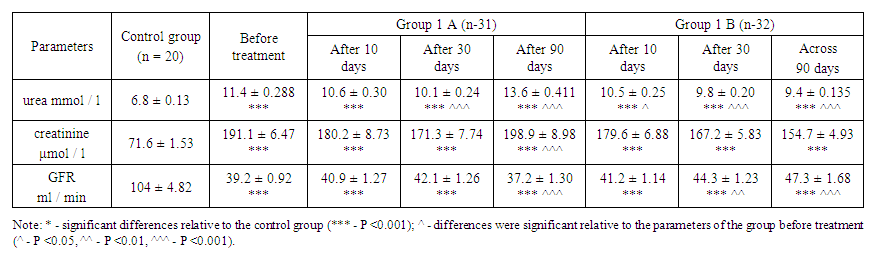 | Table 1. The state of renal function in patients with stage 3 of CKD |
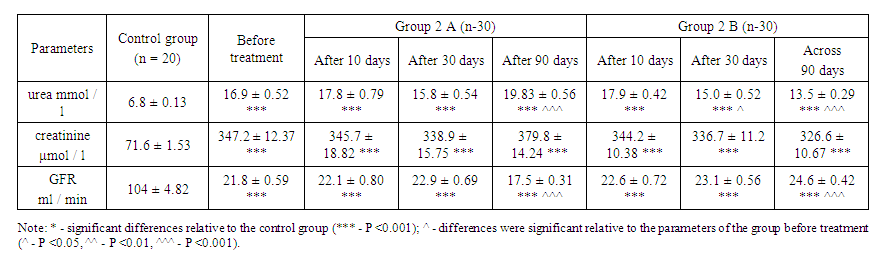 | Table 2. Renal function status in patients with stage 4 of CKD |
4. Results and Its Discussion
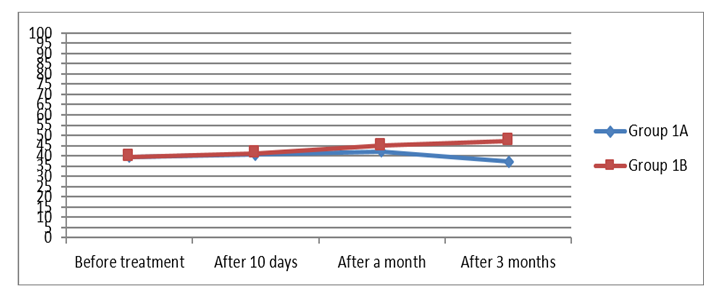
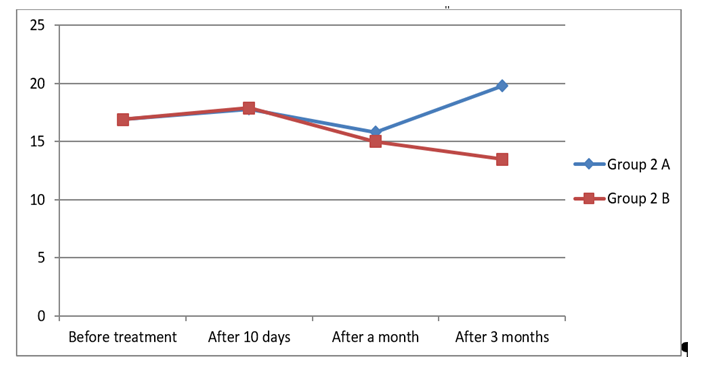
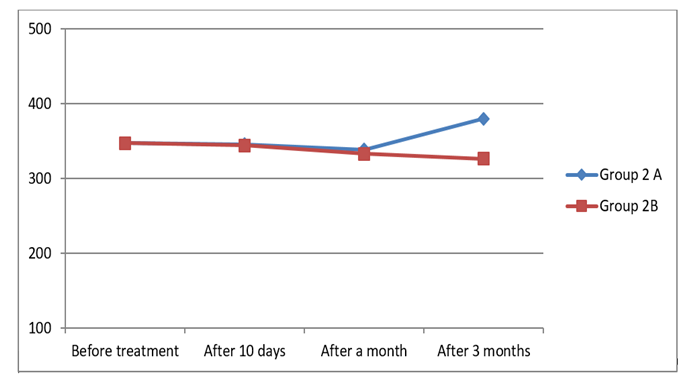
- The state of renal function: in groups 1A and 1B, the urea level averaged 11.4 ± 0.28 before treatment; the level of creatinine increased by an average of 191.1 ± 6.47, GFR decreased to 39.2 ± 9.2 ml / min.On the 10th day of treatment in patients of group 1A, the urea level averaged 10.6 ± 0.30; creatinine decreased by an average of 180.2 ± 8.73, GFR increased to 40.9 ± 1.27 ml / min. One month after the start of therapy, the urea level in group 1 A was 10.1 ± 0.24; creatinine decreased to 171.3 ± 7.74, GFR was 42.1 ± 1.26, and after three months, urea parameters increased to 16.6 ± 0.41; creatinine increased to 198.9 ± 8.98, GFR decreased to 37.2 ± 1.30 ml / min. In patients in group 1 B, urea on the 10th day of treatment averaged 10.5 ± 0.25; creatinine decreased to an average of 179.6 ± 6.88, while GFR increased to 41.2 ± 1.14. After a month, the urea values were 9.8 ± 0.20; creatinine decreased to 167.2 ± 5.83, GFR increased to 44.3 ± 1.23, three months after the start of treatment, the urea level was 9.4 ± 0.135;If we consider each indicator in the assessment of renal function, it can be seen that on the tenth day of treatment there was a slight decrease in the level of urea in both groups (A and B). One month after treatment, despite a positive shift, the levels of urea and creatinine were almost the same in both groups. However, after 3 months there was a significant decrease in the level of urea in group 1B receiving Nephrocizine compared with group 1A, a positive change was evident.
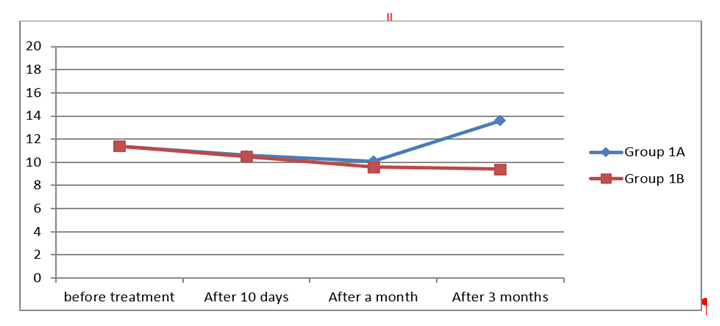 | Figure 1. Urea in dynamics |
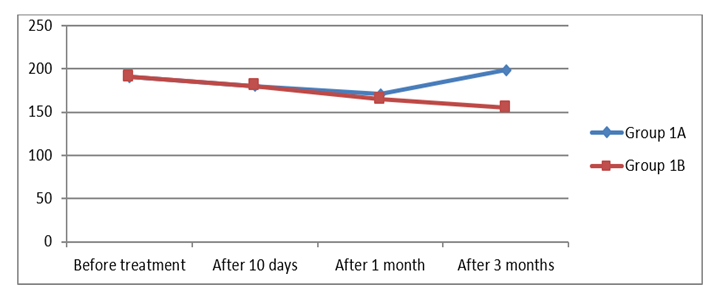 | Figure 2. Creatinine in dynamics |
 | Figure 3. Glomerual filtration rate in dynamics |
 | Figure 4. Urea in dynamics |
 | Figure 5. Creatinine in dynamics |
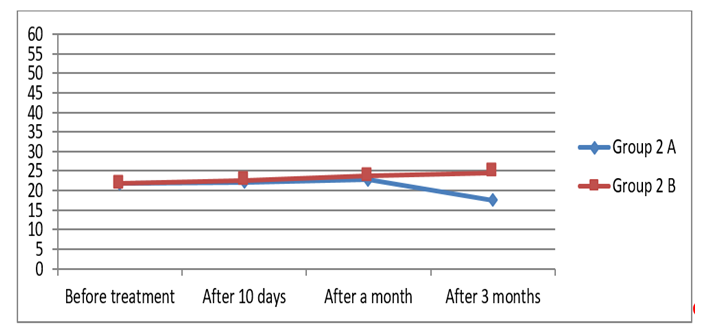 | Figure 6. Glomerual filtration rate in dynamics |
5. Conclusions
- 1. In all patients with CKD in the pre-dialysis period, an improvement in renal function and a certain positive shift in treatment are achieved with the use of Nephrocizine.2. The hypoazotemic effect of Nephrocizine at stage 3 is more effective than at stage 4 CKD.3. The drug Nephrocizine reduces uremic intoxication and slows down the progression of CKD.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML