-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(11): 885-893
doi:10.5923/j.ajmms.20201011.11
Received: Sep. 23, 2020; Accepted: Oct. 26, 2020; Published: Nov. 15, 2020

Optimization of the Therapeutic and Diagnostic Approach in Inflammatory Periodontal Diseases in Patients with Systemic Lupus Erythematosus
Zoirov Tulkin Elnazarovich, Absalamova Nigora Fakhriddinovna
Department of Dentistry No. 2 Samarkand State Medical Institute, Samarkand
Correspondence to: Absalamova Nigora Fakhriddinovna, Department of Dentistry No. 2 Samarkand State Medical Institute, Samarkand.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Relevance. Chronic gingivitis and periodontitis in systemic lupus erythematosus is described as one of the earliest and most vivid symptoms of the disease, however, with regard to the characteristics of periodontal pathology in SLE, the literature remains controversial: some authors speak about the long-term preservation of the teeth and the development of a process similar to periodontal disease, while others describe early necrotic changes in periodontal disease and related tooth loss in patients with SLE. The aim of the study is to improve the diagnosis and treatment of the pathology of the periodontal tissues in patients with systemic lupus erythematosus by correcting microcirculatory disorders of the oral mucosa. Materials and research methods. The study is based on the results of treatment of 122 patients with inflammatory diseases of the mucous membrane of the cavity, admitted to the orthopedic department of the Samarkand Regional Dental Clinic. The patients were divided into two groups. Research results. In the main group of patients during the differentiated methods of complex treatment using a gas ozone-oxygen mixture and sodium hypochlorite solution, no complications were observed, the patients noted the comfort and painlessness of these procedures. This leads to many advantages of their use: direction of action, non-invasiveness and painlessness. Conclusions. Due to the local application and high clinical efficiency of the ozone-oxygen mixture generated by the Prozone device, the need for the use of a number of drugs with undesirable side effects has been significantly reduced. According to ultrasound Doppler ultrasound with dynamic observation, ozone therapy improved blood circulation in the microvasculature by 40%.
Keywords: Oral mucosa, Inflammatory diseases of the oral mucosa, Systemic lupus erythematosus, Microcirculatory disorders, Treatments, Quality of life
Cite this paper: Zoirov Tulkin Elnazarovich, Absalamova Nigora Fakhriddinovna, Optimization of the Therapeutic and Diagnostic Approach in Inflammatory Periodontal Diseases in Patients with Systemic Lupus Erythematosus, American Journal of Medicine and Medical Sciences, Vol. 10 No. 11, 2020, pp. 885-893. doi: 10.5923/j.ajmms.20201011.11.
1. Relevance
- Systemic lupus erythematosus (SLE) is one of the most common pathologies in the group of systemic connective tissue lesions. The incidence of SLE in developed countries ranges from 1.8 to 27.1 cases per 100,000 population, with large differences in different populations. There is evidence that over the past 40-50 years this indicator has almost tripled, and the upward trend continues [5,8]. Systemic collagenoses are autoimmune rheumatic diseases, the pathogenesis of which is based on defects in immunoregulation, leading to uncontrolled hyperproduction of autoantibodies to components of own tissues and the development of autoimmune and immunocomplex inflammation affecting many organs and systems [2,6].Chronic inflammatory periodontal diseases remain one of the most common dental pathologies, the cure efficiency of which is still low [1,2,5]. Despite the generally recognized role of the microbial factor and occlusive disorders in their development, one of the important aggravating factors of the state of the oral mucosa are somatic disorders [5,9,13]. The problem of diagnosing steatogenic pathology is of particular relevance in patients with chronic somatic diseases of autoimmune genesis, in which their own immunity is sharply weakened [4,5,12].Currently, such signs of lupus are known as lupus- vasculitis on the face in the form of a "butterfly", periorbital petechiae [3,8,11], necrotic mouth ulcers. Chronic gingivitis and periodontitis in systemic lupus erythematosus (SLE) is described as one of the earliest and most striking symptoms of the disease, however, with regard to the features of the periodontal pathology in SLE, the literature data remain controversial: some authors (Grinin) talk about the long-term preservation of the periodontaltissues and the development of a process similar to periodontal disease, others [2,6,10] describe early necrotic changes in the periodontal and the associated loss of teeth in patients with SLE. With SLE, pronounced immune, rheological, and regenerative disorders in tissues develop quite early, which negatively affects the state of the oral mucosa.In this regard, a number of questions concerning the detailed characteristics of the pathology of the oral mucosa in SLE, their relationship with general immune homeostasis in systemic lupus, as well as the effect of SLE on the state of the periodontal tissues of the oral cavity have not been sufficiently reflected in studies [7,13].
2. The Aim of the Study
- The aim of the study is to improve the diagnosis and treatment of the pathology of the periodontal tissues in patients with systemic lupus erythematosus by correcting microcirculatory disorders in the periodontium.
3. Material and Research Methods
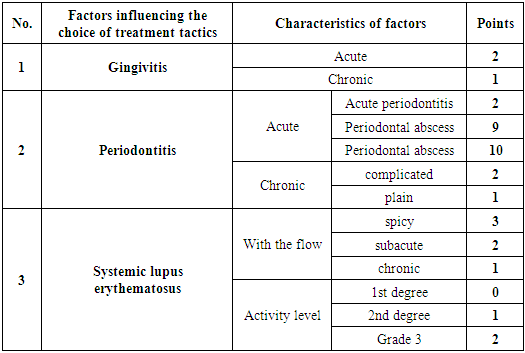
- The study is based on the results of treatment of 122 patients with inflammatory periodontal diseases admitted to the orthopedic department of the Samarkand Regional Dental Clinic. The patients were divided into two groups. The main group included 84 patients. They had concomitant somatic SLE pathology. In this group of patients, ozone therapy was included in the treatment tactics in order to improve the microcirculation of the periodontal tissues. The comparison group consisted of 38 patients without somatic pathology. All selected patients with SLE met the diagnostic criteria. According to the nature of the course of the underlying disease, SLE patients were: acute course - 15 (17.8%) patients, subacute course - 16 (19.0%), chronic course - 53 (63.1%). All patients underwent a comprehensive clinical and laboratory examination using general, private and special methods. General methods, including clinical examination of organs and systems, X-ray of the temporomandibular joint and hand joints to determine the X-ray stage of the disease, laboratory tests to determine the degree of activity of the process, biochemical and immunological blood tests were carried out in accordance with the examination standards adopted by the Ministry of the Republic of Uzbekistan.SLE had a vivid clinical picture with the involvement of the maxillofacial region, the symptoms of which were clearly visible, sufficiently evident and were verified by doctors. On the skin of the face with SLE, foci of dermatitis were usually found in a characteristic "butterfly" shape - these are hyperemic spots or pronounced telangiectasias with elements of vasculitis.In the mouth, vasculitis was manifested by various pathological elements: spots, papules, and sometimes ulceration. So, often there was a focus of congestive hyperemia in the midline of the hard palate (enanthema), sometimes accompanied by erosion and ulceration.The lesion of the periodontal disease in SLE at the initial stages of the disease was represented by catarrhal gingivitis, proceeding as an acute (and then chronic) inflammation. As a rule, the marginal gums of one or both dentitions were affected. Clinically, the pathological process at the initial stage often manifested itself in the form of bright hyperemia and edema of the gingival margin, somewhat reminiscent of hypertrophic gingivitis (edematous form).The patients complained of a feeling of pain, discomfort, sometimes burning in the gums, bad breath, bleeding of the gums when eating or brushing teeth. In the case of a chronic course of SLE lasting at least 5 years, bright hyperemia of the marginal gums and interdental papillae was replaced by a congestive bluish tinge, it was thickened (like roller-like thickenings). In the future, the process progressed like periodontitis with the formation of periodontal pockets, destruction of the tooth-gingival attachment and increased tooth mobility. In severe cases, there was a displacement of the tooth in the dentition, a violation of occlusion.In patients with SLE, the clinical picture of periodontitis was often aggravated by multiple manifestations of vasculitis, telangiectasias, and petechiae. In the area of these elements, patients had a particularly severe course of periodontitis. As a rule, the presence of extensive subcutaneous and submucosal hemorrhages, petechiae, ecchymosis in SLE patients was combined with the presence of antiphospholipid syndrome in them, which often aggravates the course of SLE and is characterized by significant hemodynamic disorders. Extensive areas of hemorrhage and vasculitis sometimes cover large areas of the body. Of the aggravating factors, there were also frequent trophic disorders in the distal regions of the body (especially the hands and feet). When located in the area of the hands, this significantly impaired the function of the hands, which affected the level of oral hygiene and, of course, worsened the level of oral hygiene, the accumulation of dental deposits and made the course of periodontal pathology heavier. In patients without adequate therapy, destructive phenomena in the periodontium rapidly increased, which were supplemented by necrotic elements of vasculitis, multiple petechiae, and ulcers. As the underlying disease progressed, the tooth - gingival ligament was destroyed and the tooth mobility increased. The clinical picture of inflammatory-dystrophic changes was combined with destructive changes in the bone tissues surrounding the tooth, characterized by the presence of deep bone "pockets" during a long course of the disease and subsequently causing tooth loss.To determine the degree of general inflammatory activity of the disease, all patients underwent determination of the levels of hemoglobin, leukocytes, immunoglobulins, ESR in the peripheral blood, etc. were carried out in the clinical and immunological in the conditions of the clinical diagnostic laboratory of the 1st clinic of the Samarkand State Medical Institute.Immunological study of blood sera included determination of rheumatoid factor titers by latex agglutination, hemolytic activity of complement, antinuclear factors, quantitative determination of immunoglobulins, circulating immune complexes and other parameters of immunological assessment of SLE.The laboratory examination included the determination of the clinical blood test (the content of hemoglobin and erythrocytes, ESR, leukocytes, the number of lymphocytes, monocytes, rod and segmented neutrophils, eosinophils and basophils), lymphocyte subpopulations (T-, B- and zero lymphocytes, T-cytotoxel T-lymphocytes and natural killer cells - MK-cells), phagocytic and adhesive activity of neutrophils, as well as a protein of the acute phase of inflammation - C-reactive protein.The clinical analysis of blood was determined by a conventional method. The content of leukocytes in blood was counted, diluted in 20 times 3%-nym solution of acetic acid in the Goryaev camera. The leukocyte formula was calculated in a blood smear stained according to Romanovsky- Giemsa using a light microscope.Subpopulations of lymphocytes were determined by differentiated antigens on the cell surface by enzyme immunoassay, as well as using a set of methods of rosette formation.The complex of methods of rosette formation and phagocytosis was set from capillary blood from a finger using microtechnology. Leukocytes were isolated from whole blood by hemolysis of erythrocytes with distilled water, followed by restoration of the osmotic pressure of the fluid by adding physiological solution of 10-fold concentration. Then the resulting suspension of leukocytes was introduced into the wells of plates for immunological reactions.The level of C-reactive protein (CRP) was determined by the latex-agglutination method. The method is based on an immunological reaction between CRP and antibodies to CRP immobilized on the surface of latex particles. We used the Human test system (Germany).Patients of the main group underwent ozone therapy. The ozone therapy procedure was carried out using the UOTA-60-01-Medozon apparatus.Special research methods included a set of objective indicators characterizing the state of teeth and periodontal tissues (for the convenience of mathematical processing of the results, numerical expressions were used using indices).The data obtained in the study were subjected to statistical processing on a Pentium- IV personal computer using the Microsoft Office Excel-2016 software package, including the use of built-in statistical processing functions. We used the methods of variational parametric and nonparametric statistics with the calculation of the arithmetic mean of the indicator under study (M), standard deviation (σ), standard error of the mean (m), relative values (frequency, %). The statistical significance of the obtained measurements when comparing the mean values was determined by the Student's test (t) with the calculation of the error probability (P) when checking the normal distribution (by the kurtosis criterion). The level of reliability P < 0.05 was taken as statistically significant changes.The influence of SLE in the complex treatment of inflammatory periodontal diseases attracts the attention of clinicians and morphologists. Modern studies of periodontitis and SLE indicate the relationship between these diseases. Uncontrolled SLE and its complications aggravate infectious and inflammatory processes in the course and development of various forms of periodontitis, and impaired peripheral blood circulation in the periodontal tissues negatively affects the treatment process and further provokes systemic inflammatory processes. A number of works indicate the dominant role of SLE in increasing the risk of periodontal disease [Sundukov V.Yu.]. A relationship has been established between SLE and an increased risk of infectious complications, with a special role being played by impaired microcirculation. In addition, disturbance of microcirculation can inhibit the proliferation of osteoblasts. Clinically The comorbidity of SLE and periodontal diseases in the oral cavity is manifested by bleeding and swelling of the gums, the presence of multiple simultaneous periodontal abscesses, the proliferation of granulation tissue, gum recession, and progressive bone loss [5-8]. The study of the morphology of the soft tissues of inflammatory foci in the complex treatment of infectious and inflammatory processes of the periodontium against the background of SLE will allow the development of new methods of influencing the periodontal tissues.To achieve the goal, gingival biopsies were taken from 28 patients with SLE for morphological study of histological changes in periodontal tissues in SLE. The material was the tissue of the gingival mucosa taken before and after the complex treatment of periodontal diseases using ozone therapy in this group of patients. Ozone therapy was carried out according to generally accepted methods. According to the indications, the patients were prescribed mouthwash with ozonized antiseptics. The study of periodontal soft tissues was carried out before complex treatment and 1-3 months after treatment. Thus, in 12 cases, the material was taken before the treatment of periodontitis. In the second group, 16 biopsies were examined one month after the complex treatment of periodontitis and SLE.The object of the study was fragments of soft tissues of the marginal periodontium measuring 0.2 x 0.5 cm (2-4 fragments in each observation), fixed in a 10% solution of buffered formalin. The material was embedded in paraffin according to the standard technique; until the block was completely cut off, serial histological sections with a thickness of 5 μm were prepared and stained with picrofuchsin, hematoxylin, and eosin.Biopsies were examined under a light microscope; the total volume of the examined material was 28 histological preparations. Objectification of morphological studies was ensured by the use, along with descriptive microscopy, of morphometric techniques. In our work, we used the calculation of the percentage (volumetric density) of epithelium, connective tissue, inflammatory infiltrate on preparations stained with picrofuchsin. Subsequent statistical processing of the obtained data was carried out with the Windows 7.0 program using the standard Statistica 6.0 software package, by the point counting method based on the Videotest- Morfo image visualization computer program. Histometric algorithm the study included preliminary measurements with the determination of the required number of counting signs, determination of the correction factor for tissue shrinkage, testing the hypothesis for normal distribution and actually taking measurements of 12 in each histological specimen.The study was carried out in the histological laboratory of the department of histology, embryology and cytology (head of the department, DSc, associate professor Oripov F.S.) of the Samarkand State Medical Institute. Histological preparations of gum tissue reflected preexisting changes in the soft tissues of the periodontium in chronic inflammatory diseases, primarily in chronic periodontitis, in patients with SLE. In biopsy specimens, fragments of the mucous membrane had pronounced changes characteristic of chronic inflammatory diseases both from the side of the stratified squamous epithelium and from the underlying fibrous tissue. In the epithelium, acanthosis is expressed with vacuolization of cells in the Malpighian layer, edema and loss of intercellular contacts of epithelial cells. In some biopsies, the epithelial layer was sharply thinned, with smoothing of the papillae and areas of desquamation of the epithelium, intraepithelial leukocyte infiltration of the basal and prickly layers.All examined patients with SLE showed degeneration of the epithelial layer of the gums, the presence of vacuoles in the epithelial cells of the surface layer. Focal accumulations of PAS-positive material were noted. These changes may indicate the beginning of the formation of parakeratosis. Along with this, acanthosis was noted, mostly moderate, sometimes pronounced.Changes in the papillary and reticular layer of the connective tissue stroma were moderately expressed. Swelling and homogenization of collagen fibers was noted. When stained picrofucsin observed 80 pikrinofiliya, while PAS-reaction - the accumulation of a raspberry-red granules. These phenomena are indicative of the accumulation of plasma proteins in the stroma. Quite often, patients with SLE had collagen necrosis with the formation of basophilic deposits in the gum tissues. The infiltrate contained a large number of plasma cells with the formation of Russel's bodies (in almost all examined patients).In the zones of forming granulations in the walls of numerous vessels and in the fibers of the connective tissue, there was a different severity of tinctorial properties when stained with picrofuchsin, different fiber thickness and the formation of collagen clumps.Against the background of the described chronic inflammatory process in some preparations, it was possible to draw attention to the presence of thickening of their wall from the side of small arterial vessels with the deposition of loose protein masses in it in the form of lumps, homogeneous deposits, or the formation of split thin collagen fibers. These signs are characteristic of lupus microangiopathy.In addition, the mucous membrane of the gums had pronounced features of proliferative processes with signs of dysregeneration due to disturbances in the vascular blood supply and a shift in normal epithelial- stromal relationships that were observed during the duration of the inflammatory process against the background of SLE. On the preparations, this was expressed in the presence of signs of metaplasia and dysplasia of the epithelial layer, some coarsening of the collagen fibers of the stroma with a predominance of the cellular component. So, in some areas in the epithelial layer, a granular layer appeared, indicating the tendency of the multilayer squamous non-keratinizing epithelium to keratinization, intraepithelial the formation of vessels with an edematous thickened wall. In several preparations, zones with signs of mild dysplasia of epithelial cells and loss of vertical anisomorphy inherent in multilayer epithelium were found.The general morphological picture corresponded to a pronounced chronic inflammatory process with the presence of disturbances in the proliferative- reparative relationship, often with signs of exacerbation, the appearance of exudative-necrotic reactions and lesions of small arterial vessels.Actively treated patients with long-term disease were characterized by sclerosis and hyalinosis of the gingival stroma. The number of fibroblasts increased. These changes were observed in 5 patients.In the mucous membrane, elements of vasculitis, characteristic of the lupus process, were often determined. In 6 patients, productive vasculitis (mainly capillaritis and venulitis) was revealed. Proliferation of the endothelium, pronounced intratissue edema of the walls of all vessels was noted. PAS staining revealed neutral mucopolysaccharides of plasma origin in the basement membrane. These changes were accompanied by the presence of a large number of lymphohistiocytic elements with an admixture of plasma cells in the perivascular spaces. Productive-destructive vasculitis occurred in 3 patients... The exit of erythrocytes outside the vessel lumen was noted. Hardening of blood vessels occurred in 2 patients with SLE duration of at least 9 years.All patients with SLE had varying degrees of severity of inflammatory changes in the gums (alterative or productive), which correspond to the morphological picture of chronic gingivitis. Massive diffuse lymphoplasmacytic stromal infiltrates were detected in 3 patients.Focal lymphohistiocytic infiltrates were observed in 3 patients and minimal - in 4. It should be noted that 5 patients had a nuclear pathology - a pathognomonic sign of lupus. These were patients with III degree of SLE activity. The nuclei of the inflammatory cellular infiltrate in the places of pronounced inflammation were hyperchromic, there were fragments of nuclei up to the formation of "nuclear dust". Necrotic collagen was impregnated with nuclear material and formed basophilic deposits.Exacerbation of the pathological process was manifested by diffuse and diffuse-focal lymphoplasmacytic infiltration, signs of nuclear pathology, as well as the saturation of the walls of blood vessels and collagen fibers with plasma proteins of the blood.1 month after the standard treatment of periodontitis with the use of ozone therapy in patients with chronic periodontitis and the presence of SLE II and III activity in the tissues of the marginal periodontium, the signs of a chronic inflammatory process changed, often with an improvement in microcirculation.In most cases, polymorphic cell and lymphoid infiltration remained, fibrotic changes increased, but mature collagen fibers replaced only a small part of the area against the background of pronounced granulations. There were also noted morphological signs of dysregeneration both from the side of the epithelium and from the side of stromal structures with the presence of collagen fibers of varying degrees of maturity and tinctorial properties.Thus, microscopic examination of histosections of periodontal tissue with signs of inflammation in patients with SLE and subjected to complex treatment with ozone therapy showed the following changes.The tendency of the inflammatory process to subside with a significant development of the reparative process noted in the description of the drugs, signs of maturation of connective tissue and restoration of the structure of the epithelial lining, persisting changes in the microvascular bed are confirmed by the results of histometric studies.As a result of a morphological study of the gum tissue in inflammatory periodontal diseases, it can be concluded that against the background of SLE and the presence of lupus microangiopathy on the part of the arterial vessels of the gingival mucosa, complex treatment with ozone therapy leads to a significant decrease in the inflammatory process. Already a month after treatment, most patients showed morphological signs with a subsiding of the inflammatory process, an increase in proliferative reactions, as well as an increase in the degree of blood flow in the microvasculature.Comparative study of periodontal tissue histosections against the background of inflammatory changes in patients with SLE before and after complex treatment with ozone therapy showed a significant difference in positive changes in dynamics.Thus, in SLE, the most striking changes were observed in patients with active lupus, as well as with subacute and chronic course of the disease. Typical signs were lymphocytic infiltrates with an admixture of plasma cells, nuclear pathology and productive vasculitis. Exacerbation of the pathological process was manifested by diffuse and diffuse focal lymphoplasmacytic infiltration, signs of nuclear pathology, as well as the saturation of the walls of blood vessels and collagen fibers with plasma proteins of the blood. Remission was characterized by a predominance of stromal and vascular sclerosis. The combination of active inflammation and sclerotic changes reflected the undulating course of the disease and periodically conducted active therapy.The tactics of treating inflammatory periodontal diseases in patients with SLE and in somatically healthy patients provided for the most individualized approach, considering the data of general and dental status.The treatment was complex in nature with the use of local effects and systemic measures, which were aimed not only at eliminating the inflammatory process in the periodontium, but also at eliminating the side effects of SLE.Regardless of the form and stage of the pathological process in the periodontium, local treatment began with a thorough removal of dental plaque. The procedure was performed using a scaler or sharp excavators and hooks. Tartar removal was completed with antiseptic treatment of the gingival margin.Local treatment of inflammatory diseases of the periodontal tissues in patients with SLE (main group of patients) and without somatic pathology (comparison group) was differentiated. Patients of the comparison group without somatic pathology received local treatment according to the standard.In catarrhal gingivitis, the first step is to teach the patient how to care for the oral cavity. Tartar and plaque were removed, hygienic measures were prescribed using pastes and rinses, which have anti-inflammatory and anti- exudative effects.At the edematous stage of hypertrophic gingivitis, the choice of treatment method was determined by etiological factors. After removing dental deposits, it was advisable to resort to therapeutic dressings with steroid ointments, for which they were mixed with artificial dentin powder. As a keratolytic agent, a 30% solution of resorcinol on turunda and a 25% solution of zinc chloride were used. Prescribed rinsing to relieve swelling: sodium chloride solution and chamomile decoction, preparations of the nitrofuran series.In the fibrous form of hypertrophic gingivitis, surgical excision of the papillae followed by electrocoagulation was performed.Since the main role in the etiology of ulcerative gingivitis belongs to the microbial factor, the success of treatment largely depended on the local use of antibacterial drugs. Treatment began with antiseptic treatment of the gums using 2% hydrogen peroxide solution, potassium permanganate solution (1: 1000), 0.2% chlorhexidine and furacilin solution. Interdental spaces were treated with turunda, after which they proceeded to a thorough and careful removal of dental plaque. The procedure was performed under application and infiltration anesthesia in the form of aerosols or lidocaine- based ointment.For patients with concomitant SLE in inflammatory periodontal diseases, local therapy was differentiated depending on the severity of the inflammatory process, the nature of the course of the disease and morphological changes in the periodontium. We evaluated the factors that influenced the treatment results using a point scale (table 1).
|
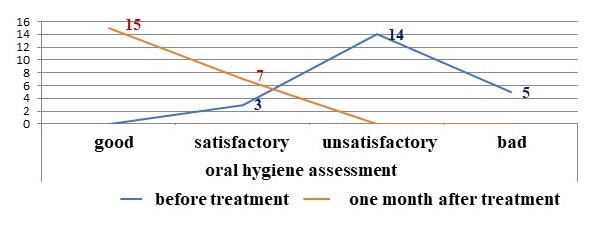 | Figure 1. Evaluation of the oral hygiene index before and after inhalation with ozonized oral solution in patients of the main group |
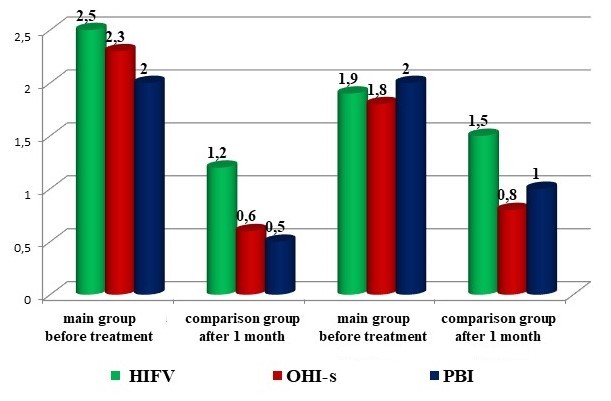 | Figure 2. Assessment of changes in the level of oral hygiene and bleeding of the gums by the reduction of indicators of hygienic indices and the index of bleeding |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML