-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(11): 881-884
doi:10.5923/j.ajmms.20201011.10
Received: Sep. 23, 2020; Accepted: Oct. 25, 2020; Published: Nov. 15, 2020

Optimization of Radiological Diagnostics of Injuries of the Soft Tissue Structures of the Knee Joint and Their Complications
Хamidov Obid Abduraхmаnovich
Samarkand State Medical Institute, Republic of Uzbekistan, Samarkand
Correspondence to: Хamidov Obid Abduraхmаnovich, Samarkand State Medical Institute, Republic of Uzbekistan, Samarkand.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Relevance. The main advantages of MRI are the ability to directly visualize and simultaneously assess the state of the synovial membrane, articular cartilage, fibrocartilaginous structures, bones and paraosseoussoft tissues, as well as the possibility of morphological identification of tissues and control of tissue contrast based on their different signal characteristics in different modes of study. the aim of the study is to improve the radiological diagnosis of injuries to the soft tissue structures of the knee joint and their complications. Material and methods. The study included 11 patients with partial and complete cruciate ligament injuries. Research results. Ligamentous apparatus injuries were clinically characterized by various manifestations. In the case of cruciate ligament injuries, clinical symptoms were nonspecific and included pain, swelling, and limitation of movement in the joint, and a drawer symptom. Conclusion. Due to the possibility of obtaining a multi-plane spatial image of the ligaments with the help of MRI, a significantly higher quality image of the ACL, including due to the lack of anisotropy effect and the need for forced knee flexion, MRI is a more effective diagnostic method in recognizing injuries of the ligamentous apparatus.
Keywords: Knee joint, Damage to intra-articular structures, Diagnostics, Ultrasound, Magnetic resonance imaging, Arthroscopy
Cite this paper: Хamidov Obid Abduraхmаnovich, Optimization of Radiological Diagnostics of Injuries of the Soft Tissue Structures of the Knee Joint and Their Complications, American Journal of Medicine and Medical Sciences, Vol. 10 No. 11, 2020, pp. 881-884. doi: 10.5923/j.ajmms.20201011.10.
Article Outline
1. The Relevance of Research
- Considering that only 6% of injuries of the knee joint are related to bone structures, and the rest to damage to soft tissue structures [3,6,7], the role of ultrasound and MRI, highly informative methods for diagnosing menisci and ligaments of the knee joint, becomes obvious. The main advantages of MRI are the possibility of direct visualization and simultaneous assessment of the state of the synovial membrane, articular cartilage, fibrocartilaginous structures, bones and paraosseous soft tissues, as well as the possibility of morphological identification of tissues and control of tissue contrast based on their various signal characteristics in different modes of study [2,4,8]. Therefore, the use of MRI is a highly informative non-invasive (as opposed to arthroscopy) method for diagnosing injuries of the knee joint, but insufficient availability and high cost of examination limit the use of this method at present.The literature data on the diagnostic value of ultrasound in injuries to the soft tissue structures of the knee joint [1,3,9] are rather high, but still not informative enough, compared with MRI and arthroscopy, which requires further improvement of the method. The indicators of the effectiveness of ultrasound in relation to damage to each intra-articular element of the knee joint, especially the ligaments, are insufficiently covered, which would allow to optimize the algorithm of clinical and radiation examination [5,7,10].Thus, the high frequency of injuries and insufficient knowledge of pathological changes in the knee joint determine the urgency of the problem and substantiate the need to improve the issues of radiological diagnosis of pathologies of the soft tissue structures of the knee joint.
2. Aim of the Study
- Aim of the study is to improve the radiological diagnosis of injuries to the soft tissue structures of the knee joint and their complications.
3. Research Material
- The study included 11 patients with partial and complete cruciate ligament injuries.
4. Research Results
- In 36.4% of cases, the presence of fluid in the volvulus and the joint cavity was determined. Signs of deforming arthrosis were not identified in this group. In 19.3% of patients with ligament injuries, areas of bone marrow edema were identified.Ligamentous apparatus injuries were clinically characterized by various manifestations. In the case of cruciate ligament injuries, clinical symptoms were nonspecific and included pain, swelling, and limitation of movement in the joint, and a drawer symptom.X-ray of joints in patients of this group in 80.8% of cases did not reveal any pathological changes, and in 19.2% - signs of subluxation in the joint were determined. Ultrasound signs of cruciate ligament injury were local changes at the site of injury as compared to the contralateral side. In case of complete ruptures, the site of injury was filled with a hematoma, which was detected as an an- or hypoechoic zone with or without hyperechoic inclusions. In case of partial damage to the ligaments at the site of damage, an - or hypoechoic area, thickening and partial interruption of the ligament fibers, concomitant edema of soft tissues was determined.The damage to the anterior cruciate ligament according to ultrasound was characterized by a decrease in echogenicity (69%) and its thickening (67%) compared to the contralateral side (Fig. 1). The diagnosis was difficult because the anterior access for the ultrasound beam was limited, since the patient could not bend the knee optimally due to pain. When viewed from the posterior approach, in 26% of cases, a delimited accumulation of a hypoechoic fluid along the lateral edge of the intercondylar sulcus was revealed, which corresponded to the appearance of a hematoma.
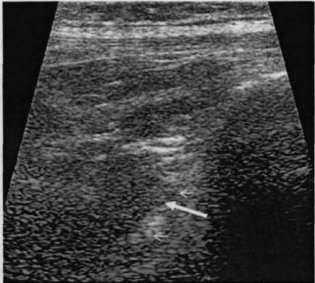 | Figure 1. Echogram of the knee joint. Partial damage to the anterior cruciate ligament |
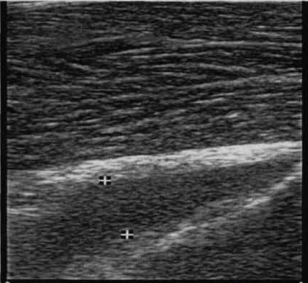 | Figure 2. Echogram of the knee joint. Partial injury to the posterior cruciate ligament |
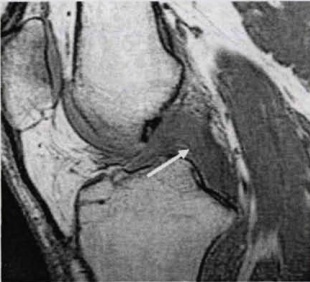
 | Figure 3. MRI of the knee joint. Sagittal projection. Partial damage to the anterior cruciate ligament |
 | Figure 4. MRI of the knee joint. Sagittal projection. Partial injury to the posterior cruciate ligament |
 | Figure 5. Arthroscopy. Anterior cruciate ligament rupture |
5. Conclusions
- Thus, when diagnosing ruptures of the ligamentous apparatus of the knee joint, ultrasound, MRI and arthroscopy demonstrate high diagnostic capabilities in comparison with radiography, since these methods can reveal direct signs of damage to the ligaments that are not visible on radiographs. Indicators of the diagnostic significance of MRI in detecting ligament ruptures are higher than with ultrasound. The X-ray method is low-informative in relation to data on pathological changes in the ligamentous apparatus, but this method must be used as a technology designed to exclude other pathological processes.Analysis of the results of the study of patients in this group allowed us to clarify the ultrasound and MP symptoms of ligament injuries. The main ultrasound criteria for detecting damage to the ligamentous apparatus were a thickening and a decrease in echogenicity, violation of the integrity of the fibers, their anatomical continuity. Intra- and periarticular edema was an additional sign. Although these ultrasound signs for the knee ligaments were identical, there were also differences in diagnosis. Edema of soft tissues was absent with damage to the LCS, due to its extracapsular location, which made ultrasound diagnostics much more difficult. There were also differences in the diagnosis of injuries of the lateral ligaments and the patella's own ligament from the cruciate ligaments and were associated with the following points. First, the depth of the cruciate ligaments, especially the ACL, is greater than the others, which directly leads to a decrease in the quality of ultrasound imaging. Secondly, the possibility of maximum flexion of the knee joint for optimal visualization of the ACL is often limited by pain, which practically excludes an adequate diagnosis of its damage. And, thirdly, this is the effect of anisotropy, which worsens the diagnosis of the cruciate ligaments to a much greater extent than the lateral ligaments, and even more so, the patellar ligament itself. MPT signs of traumatic damage to the ligaments were reduced to the appearance of an area of increased intensity of the MP signal on T2-WI in the ligament substance, discontinuity of a low-intensity ligament strip, partial or complete absence of its image, change in the ligament axis, the presence of a localized zone of edema or fluid accumulation around the ligament. Due to the possibility of obtaining a multiplanar spatial image of the ligaments with the help of MRI, a significantly higher quality image of the ACL, including due to the lack of anisotropy effect and the need for forced knee flexion, MRI is a more effective diagnostic method in recognizing injuries of the ligamentous apparatus. presence of a localized area of edema or accumulation of fluid around the ligament. Due to the possibility of obtaining a multiplanar spatial image of the ligaments with the help of MRI, a significantly higher quality image of the ACL, including due to the lack of anisotropy effect and the need for forced knee flexion, MRI is a more effective diagnostic method in recognizing injuries of the ligamentous apparatus. presence of a localized area of edema or fluid accumulation around the ligament. Due to the possibility of obtaining a multi-plane spatial image of the ligaments with the help of MRI, a significantly higher quality image of the ACL, including due to the lack of anisotropy effect and the need for forced knee flexion, MRI is a more effective diagnostic method in recognizing injuries of the ligamentous apparatus. Conflicts of interest: The authors have no conflicts of interest. Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML