-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(11): 876-880
doi:10.5923/j.ajmms.20201011.09
Received: Oct. 5, 2020; Accepted: Oct. 30, 2020; Published: Nov. 15, 2020

Characteristics of Metabolic Syndrome and Cardiovascular Injuries in Gout
Doston Rustamovich Tairov, Saodat Khabibovna Yarmukhamedova, Munira Alisherovna Khusainova
Samarkand State Medical Institute, Samarkand, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

50 patients with gout were examined. Of the examined, 28 (56%) patients were diagnosed with metabolic syndrome. The most common risk factors for cardiovascular damage in patients with gout are hypertension, a decrease in high-density lipoprotein cholesterol, high cholesterol, additional factors - an increased body mass index and hypertriglyceridemia, which aggravate the course of the disease in relation to the clinical course of the underlying disease.Metabolic syndrome was diagnosed in 28 (56%) patients participating in the study. Metabolic syndrome was found in 49.2% of patients with recurrent gout and in 58.1% of patients with chronic gout.
Keywords: Gout, Metabolic syndrome, Arterial hypertension, Cholesterol, Cardiovascular diseases, Diabetes
Cite this paper: Doston Rustamovich Tairov, Saodat Khabibovna Yarmukhamedova, Munira Alisherovna Khusainova, Characteristics of Metabolic Syndrome and Cardiovascular Injuries in Gout, American Journal of Medicine and Medical Sciences, Vol. 10 No. 11, 2020, pp. 876-880. doi: 10.5923/j.ajmms.20201011.09.
Article Outline
1. Introduction
- Gout belongs to diseases known since ancient times: crystals of sodium urate were found in one of the Egyptian mummies in the area of the big toe. The first classical description of gouty arthritis ("Treatise on gout and dropsy", 1683) belongs to the English clinician Th. Sydenham. In 1883, A. Garrod, with the help of a thread dipped into the blood of a patient with gout, discovered the fact of an increase in the level of uric acid in the blood - hyperuricemia. In 1889, urate crystals were found in the articular fluid of a patient during acute gouty arthritis. A. Gatman (1950), on the basis of "essential hyperuricemia", characterized the disease as a congenital disorder of purine metabolism. Only in 1961 MacCarty and Hollander finally established the role of urate crystals in the development of acute gouty arthritis. The possibilities of modern diagnostics and clinical pharmacology make the global perception of a pathological state absolutely accessible to the doctor as an interconnected complex of disorders with chain reactions and reversibility of processes in a large percentage of cases. This looks optimistic for both the patient and the doctor, increasing the desired compliance [1,2,3].For the first time, the hypothesis of the relationship between uric acid levels and cardiovascular diseases was discussed in the British Medical Journal back in 1886. At present, according to the results of numerous studies, hyperuricemia can actually be considered as an independent risk factor for cardiovascular complications, it is directly related to other metabolic risk factors and acts as a significant component of the metabolic syndrome. Previously, two possible pathogenetic variants were considered, according to which defects in uric acid metabolism are realized. The first is a violation of purine biosynthesis at its various stages, leading to hyperuricemia, and later to the development of gouty arthritis and visceral changes. The second hypothesis suggested the primary damaging effect of hyperuricemia on the kidneys with the development of urate nephropathy and, as a consequence of impaired excretion of uric acid, the development of gouty arthritis and aggravation of visceral lesions [4,5].The medical and social significance of gout is explained by the annual increase in morbidity among the population, a decrease in the working capacity of patients and an increase in disability rates [6]. Gout affects 1% of the male population [7,8,9] and is the leading cause of arthritis in middle-aged men [10,11,12]. Despite improvements in screening and treatment methods, the incidence of gout has increased dramatically over the past 30 years [8,9]. In particular, according to M.S. Eliseeva et al., 65% of patients with gout die due to cardiovascular complications. In this case, atherosclerotic changes play a key role in the development of cardiovascular complications [13,14]. The high incidence of cardiovascular disease in patients with gout indicates the importance of a comprehensive study of the disease.The association of gout with components of the metabolic syndrome has been known for a long time. For at least a century, gout has been associated with various metabolic disorders such as hypertension, dyslipidemia, obesity and coronary heart disease. According to Terkeltaub A. “for a discerning doctor, the diagnosis of gout is a signal to look for concomitant diseases,” and, above all, metabolic syndrome, hypertension, and nephropathy. A high incidence of insulin resistance per se in patients with gout has been shown. The significance of insulin resistance in general lies in the fact that the combination of disorders characteristic of the metabolic syndrome significantly accelerates the development and progression of atherosclerosis. Back in the 60s of the last century, it was noted that more than 60% of patients with gout die from cardiovascular complications. As a result of numerous epidemiological studies, factors that increase the risk of developing coronary heart disease have been identified and scales have been developed for calculating cardiovascular risk. The most commonly used scales are those given in the National Cholesterol Education Program (NPCS) and SCORE (Systemic Coronary Risk Evalution), respectively, the American and European scales [15,16].Objective is to study cardiovascular lesions in patients with gout and their relationship with metabolic syndrome.
2. Materials and Methods
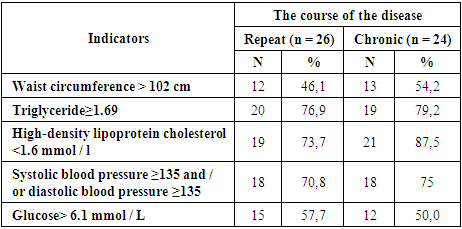
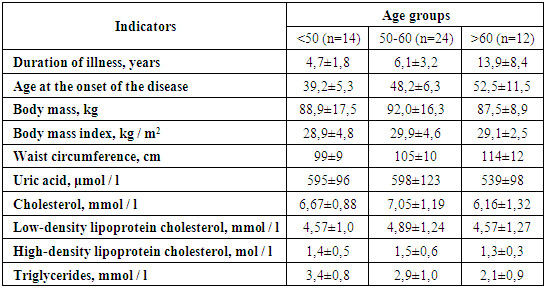
- Examination of patients was carried out in the consultative polyclinic of the 1st polyclinic of the Samarkand State Medical Institute, the department of cardiology, rheumatology, the Samarkand city polyclinic No. 3, and the Samarkand regional cardiological dispensaries. 50 patients with gout were examined. The criteria of the American College of Rheumatology (ACR, 1977) were used to diagnose patients. The average age of patients was 52.6 ± 8.2 years (from 38 to 65 years). 44.4 years - 12.4%, from 45 to 59 years - 58.7%, from 60 to 65 years - 28.9%. The average age of patients at the onset of the disease was 42.8 ± 8 years. In most patients (74.1%) the onset of the disease was observed at the age of 42-52 years. Symptoms of recurrent arthritis were found in 52% of patients, chronic arthritis - in 48% of patients. Metabolic syndrome was diagnosed based on criteria developed by the US National Institutes of Health (2001). Metabolic syndrome was confirmed if at least 3 of the following criteria were determined: - waist circumference> 102 cm; - triglycerides ≥ 1.69 mmol / l; - high density lipoproteins
3. Results
- Metabolic syndrome was diagnosed in 28 (56%) patients participating in the study. Metabolic syndrome was found in 49.2% of patients with recurrent gout and in 58.1% of patients with chronic gout.The average age of patients with metabolic syndrome was 52.8 ± 8.3, and the average age of patients without metabolic syndrome was 50.4 ± 7.6. The duration of the disease was 8.9 ± 0.27 and 6.1 ± 0.21 years, respectively. The frequency of metabolic symptoms was significantly higher among patients, as shown in Table 1. However, it should be noted that these two groups of patients have two components of the disease severity index: the number of affected joints (10 (5; 16) versus 10 (4; 15) and the amount of uric acid in plasma was 586.0 (382.0; 627.0).), in contrast to 580.0 (433.0; 621.0) μmol / l, showed almost the same values (p <0.002).
|
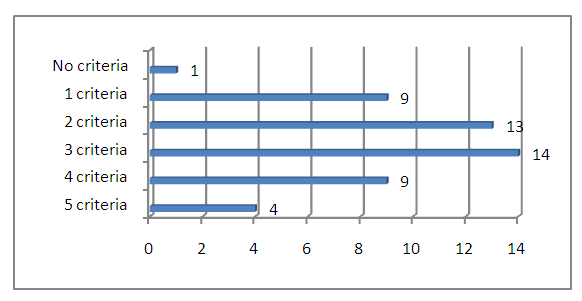 | Figure 1. Criteria for the incidence of metabolic syndrome in patients with gout |
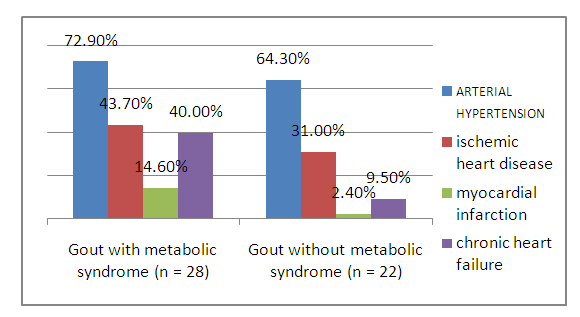 | Figure 2. Frequency of cardiovascular diseases in patients with gout with metabolic syndrome |
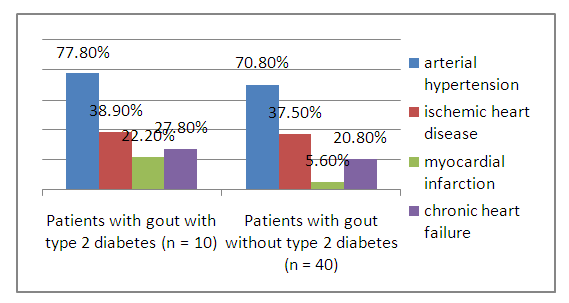 | Figure 3. The incidence of cardiovascular disease in patients with gout diagnosed with type 2 diabetes |
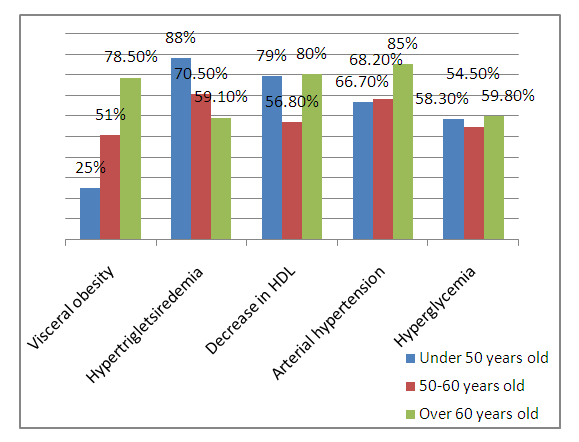 | Figure 4. Age-related frequency of metabolic syndrome and arterial hypertension in patients with gout |
|
4. Conclusions
- 1. The main risk factors for cardiovascular damage in patients with gout are hypertension, a decrease in high-density lipoprotein cholesterol, an increase in cholesterol, additional factors - an increase in body mass index and hypertriglyceridemia, which are associated with the clinical course of the disease.2. The results of the analysis of indicators show that the importance of obesity and hypertension in the early onset of gout, as well as the fact that these two factors are closely related to each other, exacerbate each other.3. The course and severity of arterial hypertension, the components of the metabolic syndrome increase in proportion to the age of the patients.
ACKNOWLEDGEMENTS
- We are grateful to the staff members of Samarkand State Medical Institute for the cooperation and support in our research. The participants kindly gave full written permission for this report.
Consent
- Written informed consent was obtained from all participants of the research for publication of this paper and any accompanying information related to this study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML