-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(11): 866-869
doi:10.5923/j.ajmms.20201011.07
Received: Oct. 18, 2020; Accepted: Nov. 1, 2020; Published: Nov. 5, 2020

Improving the Quality of Life in Disorders of Vaginal Microbiocenosis in Women with Prolapse of the Genitals
Shamsiyeva Malika Shukhratovna, Nasimova Nigina Rustamovna
Department of Obstetrics and Gynecology No. 2, Samarkand State Medical Institute, Samarkand, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Genital prolapse (PG) is a huge health problem affecting millions of women around the world. The peak incidence (56.3%) of genital prolapse occurs at the age of over 50 years. The study of vaginal microflora in women with genital prolapse (PG), for whom surgical treatment is planned, is of particular importance. It is important to be able to change the qualitative composition of microflora, thereby exerting a beneficial effect on the course of the postoperative period, influencing the outcomes of surgical treatment. 67 women took part in this study. To assess the vaginal microflora, a vaginal smear analysis followed by microscopy and microbiological culture was performed, as a result of which 87% of them (58 female patients) were found to have vaginal dysbiosis.
Keywords: Genital prolapse, Vaginal biocenosis (VB), Pelvic organ prolapse (POP), Vaginal flora, Vaginal dysbiosis
Cite this paper: Shamsiyeva Malika Shukhratovna, Nasimova Nigina Rustamovna, Improving the Quality of Life in Disorders of Vaginal Microbiocenosis in Women with Prolapse of the Genitals, American Journal of Medicine and Medical Sciences, Vol. 10 No. 11, 2020, pp. 866-869. doi: 10.5923/j.ajmms.20201011.07.
Article Outline
1. Introduction
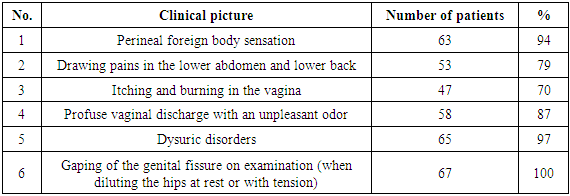
- Genital prolapse (PG) is a huge health problem affecting millions of women around the world. The peak incidence (56.3%) of genital prolapse occurs at the age of over 50 years.The problem of genital prolapse is particularly noteworthy because, according to a number of local and foreign authors, urinary incontinence in menopause affects about 50% of women [1].All of this together represents both a medical and a social problem, reducing the quality of life, including sexual function [2]. The anatomical structure and functional activity of the vagina contribute to the maintenance of a normal biocenosis, which, in turn, creates a system for protecting the reproductive system from the introduction of pathogens of a specific and non-specific infection and their subsequent spread through the genital tract. Normally, the vaginal biocenosis is 95–98 % composed of resident microorganisms and 2–5% of transient ones. Thus, the normal microflora of vagina provides the so-called colonizational resistance of the genital tract [3].Genital prolapse (GP) - common pathology reaching 34,1-56,3% in the female population of some countries [4]. Genital prolapse is an urgent clinical and surgical problem in modern gynecology [5]. There is no common understanding of etiopathogenesis and classification of GP, investigation standards, effective technologies of recurrence prevention after surgical correction in the present time [6].Pelvic floor failure (PFF) can be considered as a GP prodrome. The manifestation of PFF is often overlooked by outpatient doctors due to nonspecific complaints and insufficient knowledge of the anatomy of the perineum and underlying structures. In this regard, it should be additionally noted that normally, even in a multiparous woman, the genital fissure should not gap. A gaping genital fissure, resulting from a defect in the muscle-fascial structures of the pelvic floor, increases the risk of developing changes in the normal vaginal microbiota.Of particular relevance, the problem of GP is acquiring, in view of the tendency to "rejuvenate" this pathology [7], accompanied by severe dysfunctional changes in neighboring organs [8].Vaginal microbiocenosis is a collection of populations of different types of bacteria. It includes obligate, facultative and transient microorganisms. The number of bacteria does not exceed 10x5 - 10x6 CFU / ml [9]. According to the data of A.A. Sinyakova in the microflora of the vagina, there are about 300 species of microorganisms [10]. Most of the bacteria in the vagina are lactobacilli. The dominant species are 4 species of lactobacilli of the Lactobacillus acidophilus group: L. crispatus, L. Jensenii, L. gasseri and L. iners. There is evidence of the prevalence of lactobacilli species depending on ethnicity: in European and Asian women, 89% and 80%, and only in 61% of African women and 59% of Hispanic women [11]. The vaginal microbiocenosis reacts to any changes in the state of the woman's body [12]. Unprotected sexual intercourse, hormonal changes, changes in immunological reactivity, the use of antibiotics and many other factors contribute a damage to the natural defense mechanisms of the vagina, which creates favorable conditions for the development of opportunistic and pathogenic microflora. Dysbiotic processes of the vagina contribute to the development of VB [13]. For bacterial vaginosis, there is a characteristic symptomatology in the form of abundant discharge from the genital tract with an unpleasant odor for a long time. Many women do not attach any importance to this [14]. Some patients report itching, burning and pain during intercourse, which is the main reason for seeking medical attention.The study of the vaginal microflora in women with genital prolapse (GP), for whom surgical treatment is planned, is of particular importance.It is important to be able to change the qualitative composition of microflora, thereby exerting a beneficial effect on the course of the postoperative period, influencing the outcomes of surgical treatment [15].Purpose of the study. Development of methods for restoring vaginal microbiocenosis in women with genital prolapse.
2. Materials and Research Methods
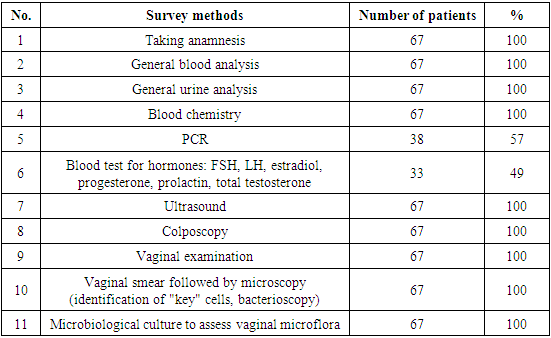
- To solve the tasks set by us, the study included 67 women of reproductive, pre- and postmenopausal age who were on inpatient treatment in the gynecological department of the Regional Perinatal Center (RPC) in Samarkand in the period of 2019-2020, as well as patients who applied to the private clinic "DOCTOR" with diagnosed GP, requiring surgical correction.The inclusion criterion at the first stage of the study was a history of surgical treatment for POP with impaired vaginal biocenosis in women.In stage II of the study conducted the visual inspection of women, in dependence on the algorithm of violations of vaginal biocenosis, which comprises of:1. Careful collection of anamnesis: complaints of discharge, itching, burning (complaints may be absent).2. Vaginal examination: - the presence and nature of the discharge; -determination of the pH of vaginal secretions - examination without a pH-metry should be considered defective at the present time; - amine test (sample with 10% KOH).3. A smear from the vagina followed by microscopy (identification of "key" cells, bacterioscopy).4. Microbiological culture study to assess the vaginal microflora.Stage III - Improving the quality of life of women with impaired vaginal biocenosis in GP.1. Creation and maintenance of optimal pH of the vaginal environment.2. Restoration of the concentration of lactobacilli at least 107 CFU / ml.
3. Research Results and Their Discussion
- Based on the examination, all 67 women (100%) for evaluation of the vaginal microflora, analyzed of vaginal smear, followed by microscopy and microbiological culture results. Vaginal dysbiosis was diagnosed in 58 (87%) patients, in 9 not identified (13%).
|
|
|
4. Conclusions
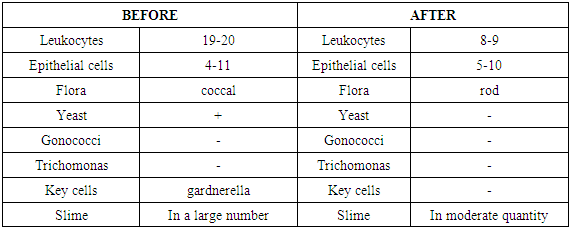
- Summing up, it should be noted that genital prolapse leads to a gaping genital fissure, provoking a violation of the vaginal biocenosis.In turn, the biocenosis of the vagina leads to changes in the structures of the pelvic floor accelerates its failure, worsening the prognosis.It is obviously clear that, the anatomical abnormalities of pelvic bottom caused by trauma can only be corrected by surgical intervention.Carrying out levatoroplasty in the first 10 years after traumatic childbirth creates the prerequisites for a reliable restoration of the vaginal biotope.However, surgical intervention performed on tissues with bacterial vaginosis can lead to intra- and postoperative complications.It is possible to get out of this vicious circle thanks to the use of probiotics at the stage of preparing patients for surgery, as well as in the postoperative period in order to avoid relapses.It was found that the use of the drugs metronidazole + micanazole and Lactobacillus acidophilus showed positive treatment results in 93% of cases.Thus, improving vaginal biocenosis before and after surgery for GP enables safely conduct GP correction, reducing the incidence of recurrence of the disease, accelerates rehabilitation process of patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML