-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(11): 858-865
doi:10.5923/j.ajmms.20201011.06
Received: Oct. 20, 2020; Accepted: Oct. 28, 2020; Published: Oct. 30, 2020

Simultaneous Laparoscopic Operations in Patients with a High Degree of Operational Risk with Chronic Calculous Cholecystitis
Batirov D. Yu., Yangibaev Z. R., Yangibaev O. Z., Rakhimov A. P., Yusupov D. D.
Urgench Branch of the Tashkent Medical Academy, Urgench, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

There have been analyzed results of clinical examination of 168 patients with chronic calculous cholecystitis with associated pathology of abdominal cavity organs, of them 88 patients with high operative risk who were performed various simultaneous laparoscopic operations. Aim of the inquiry: to improve results of the treatment of patients with chronic calculous cholecystitis with associated diseases of the abdominal cavity and high operative risk with improvement of laparoscopic methods of operations. Methods of investigation: general clinical analyses of blood, urine and feces; biochemical blood analyses; ECG; ultrasonography of the liver, gall bladder, biliary ducts, pancreatic gland, spleen and small pelvis; esophagofibrogastroduodenoscopy. The results achieved and their novelty: improved methods of simultaneous laparoscopic operations which increase diagnostic and therapeutic possibilities in associated pathology of abdominal cavity organs, particularly in the patients with higher operative risk factors that increased range of indications for simultaneous laparoscopic operations. Use of our improved methods of simultaneous laparoscopic operations in the patients with higher operative risk factors allow maximum reduction of the frequency of intra- and postoperative complications (bleeding, peritonitis, thromboembolic complications, intestinal paresis, commissural ileus, wound infection, ligature fistula, postoperative hernia, deforming scars and others) and provide high economical effect due to decrease in the costs for the following in-patients and ambulatory treatment and payment of the day of disability. Practical value: improved methods of simultaneous laparoscopic operations are safe, mini-invasive and reliable that allows their performance even in the patients with high operative risk factors (with associated therapeutic diseases).
Keywords: Laparoscopic cholecystectomy, Eppendectomy, Hernioplasty, Chronic calculous cholecystitis, Ovarian cycts, Adhesive disease
Cite this paper: Batirov D. Yu., Yangibaev Z. R., Yangibaev O. Z., Rakhimov A. P., Yusupov D. D., Simultaneous Laparoscopic Operations in Patients with a High Degree of Operational Risk with Chronic Calculous Cholecystitis, American Journal of Medicine and Medical Sciences, Vol. 10 No. 11, 2020, pp. 858-865. doi: 10.5923/j.ajmms.20201011.06.
Article Outline
1. Introduction
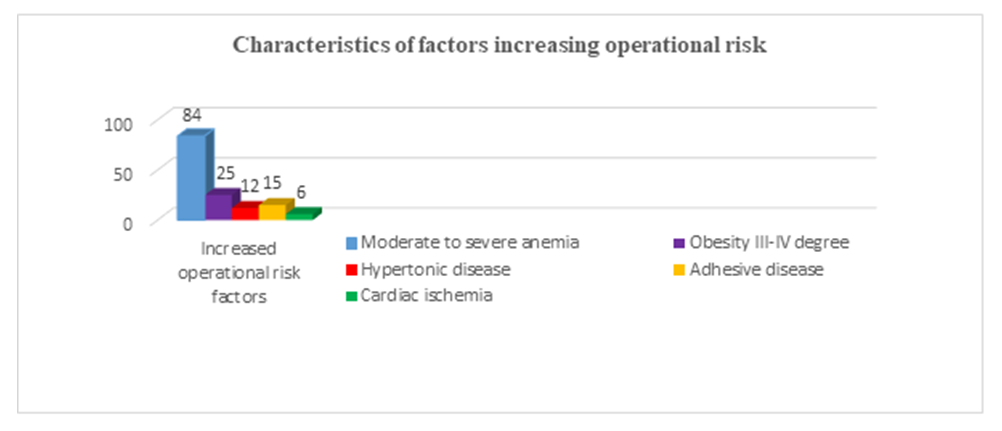
- In recent years, an increase in the number of combined pathologies of the abdominal organs requiring surgical intervention has been observed everywhere. Mass surveys of the population of the USA, Germany, Great Britain, Japan, Sweden, etc. (WHO, 1985) showed that 30% of patient’s subject to surgical treatment suffer from one or more diseases. However, simultaneous operations are performed only in less than 6% of cases (in the world's leading clinics by experienced specialists). This means that more than 94% of them in the future expect repeated surgical interventions or continue to suffer from these diseases (Malinovsky N.N. et al., 1983; Potashov L.V. et al., 1989; Stebunov S.S. and et al., 1998 and others, Brekhov E.I., 2010; Surico D., 2010).The reason for refusing to perform simultaneous operations on the abdominal organs using traditional open methods is the high risk of complications such as bleeding, peritonitis, thromboembolic complications, intestinal paresis, adhesive intestinal obstruction, wound suppuration, ligature fistulas, postoperative hernias, gross deforming scars, etc. (up to 25.5%). Mortality after such operations ranges from 5 to 26% (Krotov N.F. et al., 1997; Prudkov I.D. et al., 1997; Gallinger Yu.I. et al., 2002; Kubyshkin V.A. and et al., 2002; Karimov Sh.I. et al., 2004; Akilov Kh.A. et al., 2004; Geshelin S.A. et al., 2008; Zieniewicz K. et al., 1993; Adrales GL et al., 2003; Griffin S., 2006).The presence of concomitant therapeutic diseases, such as severe anemia, obesity III-IV degree, hypertension (HD) and coronary heart disease (СHD), as well as previous open abdominal surgery (due to adhesions) complicate even routine operations.Since the 90s of the last century, with the introduction of laparoscopic technologies in surgery, it became possible to simultaneously correct several surgical pathologies. However, despite the undeniable advantages of laparoscopic surgical methods over traditional surgical interventions (Gallinger Yu.I. et al., 1997; Balalykin A.S., 1997; Yangiev A.Kh. et al., 1997; Karimov Sh.I. and et al., 2000; Kim V.L., 2002; Hart S., 2010), many aspects of this problem have not received proper coverage.The experience accumulated in recent years, the improvement of surgical techniques, anesthetic and resuscitation care have changed not only the psychology of surgeons, but also the attitude of patients towards operations. Many of them want to simultaneously get rid of several diseases (Strekalovsky V.P. et al., 1999; Zuker KA et al., 1991; Khatkov I.E. et al., 1997; Dronova V.L. et al., 2013; Zaniotto G. et al., 1993; Jocko JA, 2013).It is known that women over 40 years of age often suffer from Chronic calculous cholecystitis (CCC), which in many of them is combined with gynecological diseases. It is in these patients that chronic anemia of moderate and severe severity is detected with a high frequency. Severe anemia is still a risk factor for even simple operations (Baulina N.V., 2005; Lebedeva E.A., 2010; Olivari N. et al., 2007).In this regard, it is of particular importance to develop, improve and introduce into surgical practice minimally invasive, reliable and easily tolerated patients with combined pathologies of the abdominal organs with a high degree of surgical risk due to concomitant therapeutic diseases (coronary artery disease, hypertension, severe chronic anemia, obesity III -IV degree), simultaneous operations using laparoscopic technologies. All this is currently acquiring not only theoretical, but also enormous practical significance.
2. Purpose of the Research
- Improvement of the results of surgical treatment of patients with chronic calculous cholecystitis and combined pathologies of the abdominal organs with a high degree of operational risk (with concomitant therapeutic diseases) by improving simultaneous laparoscopic operations.
3. Material and Research Methods
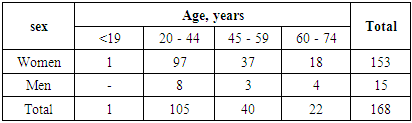
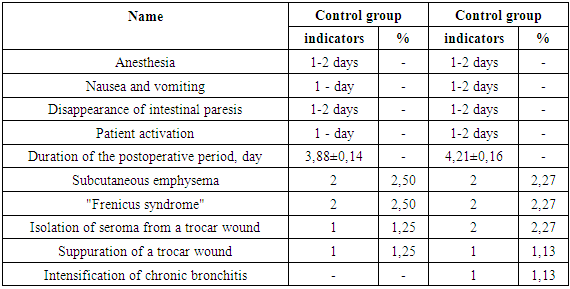
- The work is based on the results of a clinical examination of 168 patients who underwent various versions of simultaneous laparoscopic operations (SLO).The data on the distribution of patients by sex and age, made according to the WHO classification (1962), are presented in the table.As can be seen from Table 1, the majority of patients (62.50%) were at the most working age - from 20 to 44 years old.
|
 | Diagram 1 |
|
|
|
|
4. Conclusions
- 1. Application of our improved methods of simultaneous laparoscopic operations in patients with chronic calculous cholecystitis and combined pathologies of the abdominal organs with a high degree of operational risk due to therapeutic pathologies (coronary artery disease, hypertension, moderate and severe anemia, obesity of III-IV degree), and in patients, who had previously undergone open surgery on the abdominal organs, made it possible to reduce postoperative complications to 3.41% and to avoid deaths.2. Ease, simplicity, speed and minimally invasiveness of our improved simultaneous laparoscopic operations allows them to be performed even in patients with a high degree of surgical risk due to concomitant therapeutic diseases, who have previously undergone operations on the abdominal organs.3. The use of our improved simultaneous laparoscopic operations allows to reduce the time of hospital stay, to reduce the cost of treatment and payment of temporary disability certificates, which is of great medical and social importance.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML