-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(11): 833-836
doi:10.5923/j.ajmms.20201011.01
Received: Oct. 5, 2020; Accepted: Oct. 28, 2020; Published: Oct. 30, 2020

Possibilities of Bioimpedansmetry in Non-Alcoholic Fat Liver Disease
Daminov Botir Turgunpulatovich1, Usmanova Umida Shuhratovna1, Sobirova Guzal Naimovna2
1Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
2Republican Specialized Scientific and Practical Medical Center for Therapy and Medical Rehabilitation, Tashkent, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article provides an analysis of the literature data regarding the frequency of distribution, modern diagnostics and complex treatment of NAFLD. Non-alcoholic fatty liver disease (NAFLD) is currently one of the most common hepatology diseases leading to poor quality of life, disability, and death. This is primarily due to the high level of progressive development caused by non-alcoholic steatohepatitis (NASH), liver failure and hepatocellular carcinoma. Primaraly there is a high risk of progressive development non-alcoholic steatohepatitis, (NASH) liver failure and hepatocellular carcinoma caused by non-alcoholic fatty liver disease The total prevalence of NAFLD in the population varies from 10 to 40%, while the frequency of NASH is 2–4% [1].
Keywords: Non-alcoholic fatty liver disease (NAFLD), Cardiovascular diseases (CVD), Non-alcoholic steatohepatitis (NASH) insulin resistance, Hepatocardiaccontinuum (HC), Metabolic syndrome (MS)
Cite this paper: Daminov Botir Turgunpulatovich, Usmanova Umida Shuhratovna, Sobirova Guzal Naimovna, Possibilities of Bioimpedansmetry in Non-Alcoholic Fat Liver Disease, American Journal of Medicine and Medical Sciences, Vol. 10 No. 11, 2020, pp. 833-836. doi: 10.5923/j.ajmms.20201011.01.
Article Outline
1. Introduction
- Among patients with NAFLD in 90% of cases, at least one component of the metabolic syndrome is observed according to IDF 2005 [2]. On the contrary, as the number of components of the metabolic syndrome increases, the likelihood of developing NAFLD increases. According to a large cohort study, steatosis was detected in 70% of patients with diabetes mellitus [3,4].In obese patients, the prevalence of various clinical forms of NAFLD is significantly higher than in the general population and, according to research data, is 75-93%, Nash is diagnosed in 18.5-26%, fibrosis-20-37%, and cirrhosis of the liver in 9-10% of patients [5]. At the same time, up to 25% of patients with NAFLD may not be obese, but have clear laboratory and instrumental evidence of changes in the liver by the type of fatty hepatosis [6]. It was reported in one study that among NAFLD patients who did not have diabetes, 22% were thin, 64% did not meet the minimum criteria for metabolic syndrome, and 12% did not have any criteria. Korean scientist Y. Chang and cowriters. [7] showed that liver steatosisdevelopedof patients with an increase in body weight, not accompanied by an increase in body mass index (BMI). Steatosis, according to researchers, is formed during the very process of weight gain, regardless of whether the BMI exceeds normal values.Undoubtedly, BMI is a simple, easily reproducible, reliable screening criterion for assessing normal, overweight and obesity. At the same time, recent studies show that BMI is not a sufficient criterion for predicting the development and course of all diseases associated with obesity and overweight. This was reflected at the 23rd annual scientific Congress in 2014, where the American Association of endocrinologists reviewed a new algorithm for diagnosing obesity, which includes two components: a) an ethnic-adjusted BMI score to identify individuals with an increased amount of adipose tissue, and b) the presence and severity of obesity-related complications. It is even proposed to consider changing the term "obesity" (for example, "adiposity — based chronic disease" (ABCD)). Thus, today there is a shift from BMI-based obesity assessment ("BMI-based approach") to obesity assessment based on the presence or absence of obesity-related diseases or disease conditions ("complication-based approach"). These diseases included NAFLD, and its complicated forms included fatty hepatosis in combination with fibrosis and/or positive inflammatory tests [8].In this regard, one of the promising methods for diagnosing and monitoring NAFLD therapy is the method of bioimpedance measurement. Bioimpedance measurement (BIA) or bioimpedance analysis is a method for diagnosing the composition of the human body by measuring the impedance — the electrical resistance of parts of the body – in different parts of the body. It allows you to assess the nutritional status of the patient, conduct an in-depth diagnosis of obesity and metabolic syndrome, assess the sufficiency of the protein component of nutrition, and evaluate the patient's motor activity. In addition, it helps to assess the physical development of children and adolescents, identify violations of body hydration, and identify the risks of a wide range of chronic catabolic diseases [9].
2. Materials and Methods
- The essence of bioimpedance measurement is to pass a weak electric charge through the body. As a result, depending on the intensity of the charge passing through different parts of the body, the computer generates a General picture of the content of fat, muscle, mineral and water-salt mass in your body. On bioimpedance charts, this is reflected in the following blocks: body mass index; fat mass; lean mass; active cell mass; musculoskeletal mass; specific basal exchange; total fluid; extracellular fluid; waist/hip ratio; classification by percentage of fat mass (or degree of obesity) [10].
3. Results and Discussion
- There are several systems of bioimpedance measurement and, accordingly, methods of bioimpedance analysis. With Bioimpedance using the "8 electrodes" method, a person stands on a special device, wraps his hands around the handles. And the electrodes of the bioimpedance sensor, located at the level of the thumbs (1 and 2), index fingers (3 and 4), heels (5 and 6) and forefoot (7 and 8), read information about the state of your body by passing an electric current [11].Bioimpedance measurement using the "Stimulus multi-frequency measurement" method is the most sensitive technology to changes in the component composition of the body and changes in the distribution of fluid. Features of the technology are that during the measurement process, 6 frequencies of electric current simultaneously pass through the body's tissues, which creates a higher level of accuracy of bioimpedasny measurement of liquid media at the cellular level [12].Bioimpedance measurement using the method of "Direct segmental analysis" is that the device examines individual parts of the body, independently of each other. That is, if the previous devices considered the body as a whole, then here you will get separate data about the state, for example, of your hands or feet, which will allow you to more correctly direct the load during training.Bioimpedance research allows you to clearly obtain the ratio of substances in the body such as: water, muscle mass, the amount of fat, as well as for the possibility of an objective assessment of metabolism. In addition to everything else, a bioimpedance analysis is carried out to identify different conditions of the body such as exhaustion, a fitness standard, normal, overweight or obese. Bioimpedance analysis is a completely harmless procedure, but it has its own nuances. Bioimpedance measurement should be performed on an empty stomach, or 1.5-3 hours after eating and / or drinking, depending on the intensity of metabolism. Water is easier to conduct electricity and if a person drank a lot of water before the procedure, the indicators will show a higher percentage of body fat than it actually is. In addition, bioimpedance testing is not recommended for pregnant women.
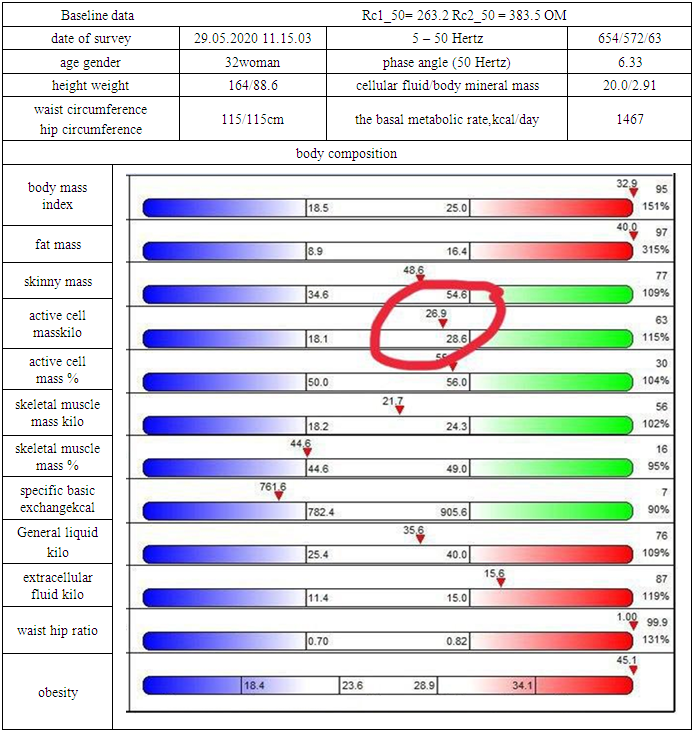
4. Example of Bioimpedance Metrics
- Showed that liversteatosis developed in case of an increase of mass patients body. To facilitate the perception of the results of bioimpedance measurement, indicators are dseivided into the necessary number of groups, for example, muscle mass, fat mass, mineral mass, as well as the level of metabolic processes occurring in the body.In addition to the known indicators of BMI, and the girts of the hip and waist bioimpedance allows you to determine the phase angle of bioimpedance - this is the value of resistance expressed by the angle to the impedance, which directly depends on the state of the cell. Body fat mass provides information about the sum of all the body's lipids (fats). The indicator of fat mass is the most plastic and can change depending on physical activity and the General condition of the person. It should be understood that the normal lipid content is directly dependent on both age and gender indicators. Thus, the norm of body fat mass for young women is 17-25%, and for men of the same age category, 12-22%. Also, it is necessary to take into account that fat accumulates both under the skin (subcutaneous fat) and near internal organs (visceral fat), and this important factor is taken into account in bioimpedance measurement [12]. Lean body mass for the most part, forms the total amount of fluid, mineral skeleton and CMB (cell mass of the body). The lean body mass norm is defined as the sum of total body water and dry body mass without fat. Active cell mass (ACM) is metabolic tissue this tissue includes liver tissue, nerve tissue, lung tissue, and others. It should be understood that the tissues related to ACM are the most sensitive to how the individual eats, to our physical, mental and psychical loads.Musculoskeletal mass – (MSM) is an indicator that characterizes the overall level of physical development of a person. Musculoskeletal mass, or bony musculature, is a muscle that has one or more ends attached to the bones, thereby allowing us to perform movements. The average amount of skeletal muscle in the limbs reaches 75% of the total MSM of our body. Bioimpedance sensors can measure skeletal musculature in all 4 limbs, allowing you to calculate the skeletal muscle mass of the entire body.Total body water is the sum of cellular and extracellular fluid. Normally, it is 45-60% of the total body weight. Using this indicator, bioimpedance sensors can detect fluid retention in the body and the presence of edema, both visible externally and hidden, which we may not even know about.Extracellular fluid (FCF) is water that contains minerals, proteins, hormones, and also regulates the water-salt balance of both cells and the body as a whole. It is found in all body tissues. Normally, the blood volume is up to 94%. With a decrease in the amount of extracellular fluid (deviation from the norm in the negative direction), blood clots occur and the risk of thrombosis increases, and with high blood counts (deviation from the norm in the positive direction), the reverse process occurs, and the blood liquefies, which can lead to bleeding, which will be very difficult to stop. Intracellular fluid (ICF) is a fluid that is located inside a cell and forms a framework for the cellar.It provides transport of substances, both from the cell and into the cell and also it provides delivery of hormones and enzymes to the place of their direct action. The ratio of FCF and ICF shows the fluid balance in the body. At high rates, edema is formed, and at low rates there is a risk of tissue dehydration.The following indicators reflect the characteristic of body mineral mass. Fat-free body mass – FFBM) - an indicator indicating the amount of water in the body, combined with the amount of tissue free of fat, such as skeletal, muscular, glandular, etc. The norm of fat-free body mass is calculated as the sum of active cell mass (ACM) and intracellular fluid (ICF), that is, FFBM = ACM + ICF.The speed of basic metabolism is an indicator that tells us how fast the metabolic processes that ensure the vital activity of our body, that is, metabolism, are going. Or in other words, how quickly calories are burned for the necessary processes, such as transferring oxygen to the tissues, ensuring brain activity, etc. You can also get additional data. Proteins –are the main component of skeletal muscle. They are also part of hormones, enzymes, are oxygen carriers in the blood, and maintain a water-salt balance in the cells.
5. Conclusions
- Thus, bioimpedance indicators can help develop personalized dietary recommendations and dosed physical activity, taking into account the indicators of fat and carbohydrate metabolism. These recommendations can contribute to the restoration of disturbed parameters of the liver in NAFLD and prevent progression of the disease.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML