-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(10): 809-816
doi:10.5923/j.ajmms.20201010.17
Received: Sep. 15, 2020; Accepted: Oct. 2, 2020; Published: Oct. 26, 2020

Risk Factor Profile for Morbidity and Mortality in COVID-19 Patients - A Brief Review
Prosper Obunikem Adogu1, Chika Florence Ubajaka1, Henry Nnaemeka Chineke2
1Department of Community Medicine, Nnamdi Azikiwe University, Awka, Nigeria
2Department of Family Medicine, Imo State University, Owerri, Nigeria
Correspondence to: Chika Florence Ubajaka, Department of Community Medicine, Nnamdi Azikiwe University, Awka, Nigeria.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus (SARS-CoV-2). The first known severe illness was in 2003 when it presented as severe acute respiratory syndrome (SARS) epidemic in China. The current outbreak and spread of the COVID-19 in human population is phenomenal with clinical features, diagnoses, management and prognosis posing daunting public health and clinical challenges. Consequently, the objective of this review is an attempt to identify the possible risk factors of COVID-19. This will possibly make for patient profiling, and ensure better public health and clinical management of disease for reduced morbidity and mortality. It is important to learn about risk factors for severe COVID-19 illness because it can help to take extra precautions to avoid exposure to the virus that causes COVID-19, and to better understand how a medical condition could affect health of patients with the disease. Also it helps to anticipate medical treatment of victims and reduce the risk for severe COVID-19 illness by instituting appropriate and timely management protocols.
Keywords: COVID-19, Patient Profile, Risk factors, Morbidity, Mortality
Cite this paper: Prosper Obunikem Adogu, Chika Florence Ubajaka, Henry Nnaemeka Chineke, Risk Factor Profile for Morbidity and Mortality in COVID-19 Patients - A Brief Review, American Journal of Medicine and Medical Sciences, Vol. 10 No. 10, 2020, pp. 809-816. doi: 10.5923/j.ajmms.20201010.17.
Article Outline
1. Introduction / Historical Perspective of COVID-19 Pandemic
- Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus (SARS-CoV-2). [1], [2] It is an enveloped non-segmented positive-sense RNA virus. [2] SARS-CoV-2 belongs to the broad family of viruses known as coronaviruses. [1] The first known severe illness caused by a corona virus was the 2003 severe acute respiratory syndrome (SARS) epidemic in China. A second outbreak of severe illness began in 2012 in Saudi Arabia with the Middle East respiratory syndrome (MERS). [3], [4] Corona represents crown-like spikes on the outer surface of the virus; thus, the name-coronavirus. [5]The virus is thought to be natural and has a zoonotic origin. [1], [4] and there are several theories about where the very first case (the so-called patient zero) originated. The first case of someone suffering from Covid-19 can be traced back to November, 2019. [1], [6] At least 266 people, starting from 17 November, contracted the virus and came under medical surveillance, weeks before authorities announced the emergence of the new virus. The Chinese government was widely criticized over attempts to cover up the outbreak in the early weeks, including crackdowns on doctors who tried to warn colleagues about a new SARS-like virus which was emerging in the city of Wuhan in Hubei province. The data said a 55-year-old from Hubei province could have been the first person to contract Covid-19. For about one month after that date there were one to five new cases reported daily, and by 20 December there were 60 confirmed cases. [6]Based on the genomic sequencing analysis of the virus, some researchers concluded that the virus evolved to its current pathogenic state through natural selection in a non-human host and then jumped to human, a replay of previous coronavirus outbreaks. In this case, bats were fingered as the most likely reservoir for SARS-CoV-2 as it is very similar to a bat coronavirus. There are no documented cases of direct bat-human transmission, however, suggesting that an intermediate host was likely involved between bats and humans. [3] Other researchers, believed that a non-pathogenic version of the virus jumped from an animal host into humans and then evolved to its current pathogenic state within the human population. However, a study co-author cautioned that it is difficult if not impossible to know at this point which of the scenarios is most likely. If the SARS-CoV-2 entered humans in its current pathogenic form from an animal source, it raises the probability of future outbreaks, as the illness-causing strain of the virus could still be circulating in the animal population and might once again jump into humans. The chances are lower of a non-pathogenic coronavirus entering the human population and then evolving virulent properties similar to SARS-CoV-2. [3] Therefore, strengthening the monitoring of wild mammals is an urgent measure needed to prevent similar viruses from infecting humans in the future. On January 7, a novel coronavirus, originally abbreviated as 2019-nCoV by WHO, was identified from the throat swab sample of a patient. This pathogen was later renamed as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by the Coronavirus Study Group and the disease was named coronavirus disease 2019 (COVID-19) by the WHO. [7] The name was chosen to avoid stigmatizing the virus's origins in terms of populations, geography, or animal associations. [8] Human-to-human transmission was confirmed by the WHO and Chinese authorities by 20 January 2020. [1] During the early stages of the outbreak, the number of cases doubled approximately every seven and a half days. In early and mid-January 2020, the virus spread to other Chinese provinces, helped by the Chinese New Year migration and Wuhan being a transport hub and major rail interchange. [1] On 30 January, the WHO declared the coronavirus a public health emergency of international concern. By this time, the outbreak spread by a factor of 100 to 200 times. On March 11, 2020, the WHO declared COVID-19 a global pandemic, its first such designation since declaring H1N1 influenza a pandemic in 2009. [8] From the foregoing, the spread of the COVID-19 among human population is phenomenal and the presentation, diagnoses, management and prognosis of this disease present daunting clinical and public health challenges. Therefore, the objective of this review is an attempt to identify the possible risk factors of COVID-19. This will possibly make for patient profiling, better public health and clinical management of disease for reduced morbidity and mortality.
2. Risk Factors and Patient Profile in COVID-19
- The global death rate for corona virus is about 3.4%, and this fatality is based on several factors, including where a patient is being treated, their age, the severity of the disease, and any pre-existing health conditions they might have. [9] Experts have also predicted that the fatality rate of the disease will decrease as the number of confirmed cases continues to rise. There is another whole cohort that is either asymptomatic or minimally symptomatic," There are some noted differences between the coronavirus and other infectious diseases, like MERS, SARS, and influenza: data suggests COVID-19 does not transmit as efficiently as the flu and that people who are infected but not yet sick with the flu are major transmitters of the disease, which does not appear to be the case for coronavirus. Also COVID-19 appears to cause a "more severe disease" than the seasonal flu, and while people around the world may have built up an immunity to the flu over time, the novelty of the coronavirus means no one yet has immunity, and more people are susceptible to infection. [9]Coronavirus is a unique virus with unique characteristics and the mortality rate of the disease can differ greatly based on the country of treatment. Furthermore, people with mild cases of the disease will recover in about two weeks, and those with severe cases may take three to six weeks to recover. Despite the higher global death rate, the number of fatalities is based on several factors including where a patient is being treated, their age, the severity of the disease, and any pre-existing health conditions they might have. [9]A study conducted recently from the Chinese Center for Disease Control and Prevention showed that the virus most seriously affected older people with preexisting health problems. The data suggests a person's chances of dying from the disease increase with age. Notably, the research showed that patients ages 10-19 years had the same chance of dying from COVID-19 as patients in their 20s and 30s, but the disease appeared to be much more fatal in people ages 50 and over. [10]COVID-19 can affect anyone, and the disease can cause symptoms ranging from mild to very severe. For some other illnesses caused by respiratory viruses (such as influenza), some people may be more likely to have severe illness than others because they have characteristics or medical conditions that increase their risk. These are commonly called “risk factors.” Examples include being 60 years of age or older or having serious underlying medical conditions.CDC in collaboration with state, local, and territorial health departments; public health, commercial, and clinical laboratories; vital statistics offices; health care providers; emergency departments; and academic and private sector partners, is conducting disease surveillance and field investigations to better understand why some people are more likely to develop severe COVID-19 illness. These efforts will provide vital information to help public health officials make decisions to protect the most vulnerable populations.It is important to learn about risk factors for severe COVID-19 illness because it can help to take extra precautions to avoid exposure to the virus that causes COVID-19, and better understand how a medical condition could affect health of patients with COVID-19. Also it helps to anticipate medical treatment of victims and reduce the risk for severe COVID-19 illness by instituting appropriate management.
3. People at Higher Risk for Severe Illness Include
- People 60 years and older
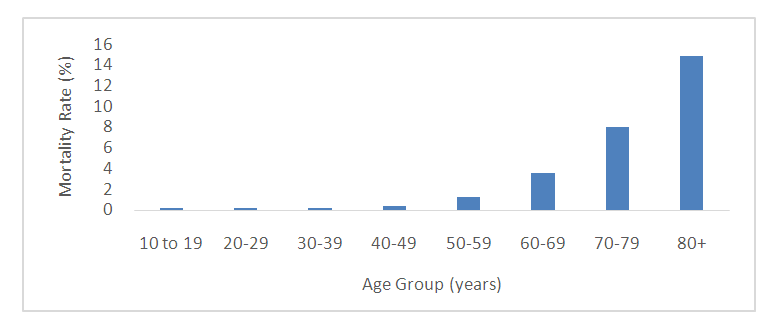 | Figure 1. COVID-19 Mortality rate by age (Source: Chinese Center for Disease Control and Prevention) |
4. Conclusions
- This brief review is an attempt to stereotype the profile of a COVID-19 victim with a view to developing and adopting appropriate, effective and efficient public health precautions and clinical measures that might reduce morbidity and mortality among people at risk, and to control the global spread of COVID-19 pandemic. This brief review is of practical significance in the sense that it offers an explanation for the hitherto amazingly low morbidity and mortality of this disease in tropical regions of Africa and Nigeria in particular. Need for further research: The pattern and clinical features of COVID-19 are still unfolding. There is therefore need for continued further research that will make for better understanding of the holistic epidemiology and control of this new scourge in the global community.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML