-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(10): 796-802
doi:10.5923/j.ajmms.20201010.15
Received: Sep. 15, 2020; Accepted: Oct. 10, 2020; Published: Oct. 17, 2020

Idices of Hepatocellular Function at Extracorporeal Detoxification in Patients with Obstructive Jaundice Complicated by Liver Failure
R. A. Ibadov1, R. A. Sadikov1, F. N. Nishanov2, B. R. Abdullajanov2, B. B. Rakhmanov2
1Republican Specialized Scientific and Practical Medical Center for Surgery Named after Academician V. Vakhidov, Tashkent, Uzbekistan
2Andijan State Medical Institute, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Aim of study was to improve the surgical treatment results of patients with endogenous intoxication and hepatocellular insufficiency on the background of obstructive jaundice by developing an original method of extracorporeal detoxification. Material and methods. The authors evaluated the effectiveness of the improved method of hyperbaric plasma adsorption in the treatment of severe obstructive jaundice. 50 patients treated in the clinic of the Andijan State Medical Institute in 2018-2019 were selected for the study. The study included only patients with severe obstructive jaundice on the background of cholelithiasis complicated by choledocholithiasis. Sessions of modified plasma adsorption were conducted in patients with obstructive jaundice and liver failure. Conclusion. The use of the improved technique of hyperbaric plasma adsorption in the complex treatment of the complicated course of obstructive jaundice by the third day after the choledocholithiasis allowed to accelerate the regression of hyperbilirubinemia from 201.5 ± 19.0 to 75.4 ± 11.3 μmol / L. These indices decreased from 194.3 ± 13.2 to 131.5 ± 13.1 μmol / L (t = 3.24; p <0.05) at standard conservative therapy. Accordingly, we observed a more intense decrease in the severity of the patients’ condition (from 11.1 ± 1.3 to 3.5 ± 1.0 points versus - from 11.1 ± 0.9 to 7.4 ± 1.0 points; t = 2.75; p <0.05). Indicators of hemostasis and inflammation markers were also significantly improved 3-5 days after procedures.
Keywords: Choledocholithiasis, Obstructive jaundice, Liver failure, Plasma adsorption
Cite this paper: R. A. Ibadov, R. A. Sadikov, F. N. Nishanov, B. R. Abdullajanov, B. B. Rakhmanov, Idices of Hepatocellular Function at Extracorporeal Detoxification in Patients with Obstructive Jaundice Complicated by Liver Failure, American Journal of Medicine and Medical Sciences, Vol. 10 No. 10, 2020, pp. 796-802. doi: 10.5923/j.ajmms.20201010.15.
1. Introduction
- According to the World Health Organization, biliary tract diseases affect a significant part of the world's population. One of the most common complications of this disease is obstructive jaundice which makes up approximately 45-50% of cases among all types of jaundice [1]. The highest rates of cholelithiasis are recorded in Western countries - 64% for women and 29% for men. The Asian region has an intermediate prevalence of 13.9% for women and 5.3% for men. However, the available statistics show that the prevalence of liver failure associated with obstructive jaundice is the highest among the population of the Asian continent [2]. New research in hepatology has significantly improved the understanding of the processes occurring at obstructive jaundice for recent years. Despite the presence of a large number of reasons that cause obstruction of the biliary tract, the mechanisms of the pathogenesis of the development of hepatic failure are non-specific and the main features of these changes for various etiological reasons are the same [3]. In most clinical situations associated with obstructive jaundice, one has to deal with endogenous intoxication, which is a sophisticated pathogenetic complex, including metabolic and functional disorders of almost all organs and systems. Today, ways to improve the results of obstructive jaundice treatment have the goal of not only improving the technical means of surgical treatment, but also eliminating the main causes of complications and mortality (cholemic and inflammatory intoxication). The methods of efferent therapy have been increasingly used to achieve this goal for recent decades. Many studies have been published on the use of extracorporeal hemocorrection methods in the treatment of liver failure, both acute and chronic for the past 20 years. The literature data are contradictory, based on the analysis of treatment results of small and heterogeneous groups of patients [4-5]. There are no studies that evaluate the complex application of various extracorporeal detoxification methods in the available literature. Most hepatology clinics in our country adhere to conservative treatment tactics for patients. There are disagreements in the definition of treatment tactics for severe liver lesions, especially in the fulminant variant of the course of the disease. There is still no consensus on the effectiveness of plasmapheresis in severe liver lesion associated with obstructive jaundice [6-8]. The appearence of modern hematoprocessors and devices for artificial support of the main liver functions, advances in transfusiology and resuscitation, new technologies in liver surgery allow to study the problem of treating liver failure from new positions and at a modern level. Aim of study was to improve the surgical treatment results of patients with endogenous intoxication and hepatocellular insufficiency on the background of obstructive jaundice by developing an original method of extracorporeal detoxification.
2. Material and Methods
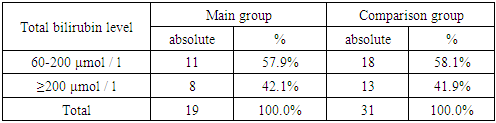
- The main direction for the clinical stage of research was the assessment of the improved method of hyperbaric plasma adsorption effectiveness in the treatment of severe obstructive jaundice. 50 patients treated in the clinic of the Andijan State Medical Institute in 2018-2019 were selected for the study. The study included only patients with severe obstructive jaundice on the background of cholelithiasis complicated by choledocholithiasis. All patients were divided into two groups. The main group included 19 patients treated in 2019, who were used an improved method of hyperbaric plasma sorption in complex treatment after endoscopic or surgical elimination of obstructive jaundice cause (choledocholithiasis). The comparison group included 31 patients treated in 2018, in whose rehabilitation the standard protocol for the management of patients with complicated obstructive jaundice was applied. There were 38 (74%) women and 12 (26%) men. The mean age was 43 years. Endoscopic papillosphincterotomy (EPST) with lithoextraction was performed in 21 cases, suprapapillary choledochoduodenostomy (SPCDS) with lithoextraction - in 8 (16%) patients and cholecystectomy, choledocholithotomy with drainage according to Ker – in 21 (42.0%). All patients according to the severity of obstructive jaundice were distributed according to the classification of E.I. Halperin (2012), proposed to assess and predict postoperative results. Initially, the assessment took into account the indicators of total bilirubin and total protein, but later in 2013 E.I. Halperin presented a simplified classification that takes into account only the total bilirubin indicator. Classification also takes into account the manifestations of complications of obstructive jaundice (cholangitis, renal failure, liver failure (signs of encephalopathy), gastrointestinal bleeding, sepsis). The total bilirubin level is distributed as follows: <60 µmol / L - 1 point, 60-200 µmol / L - 2 points, ≥200 µmol / L - 3 points (Tab. 1).
|
|
3. Results
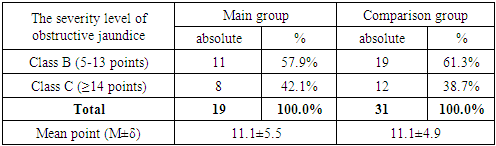
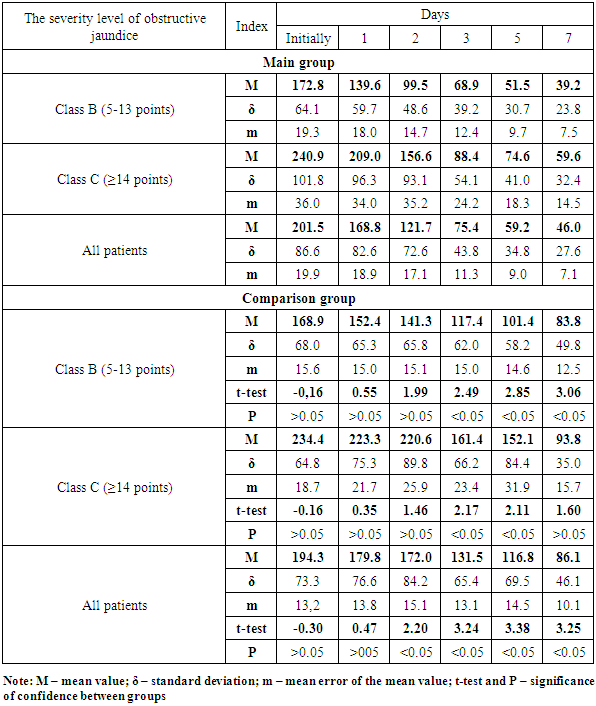
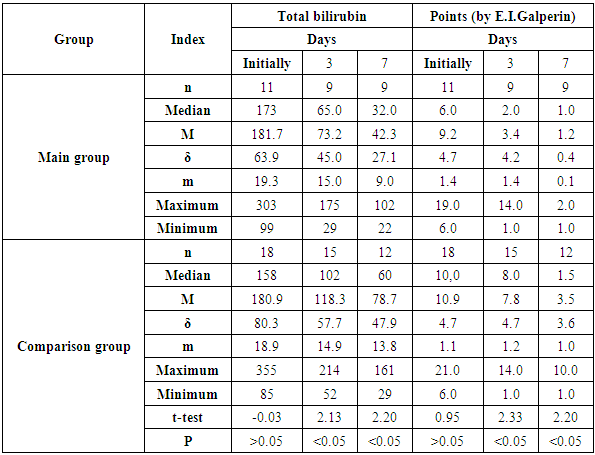
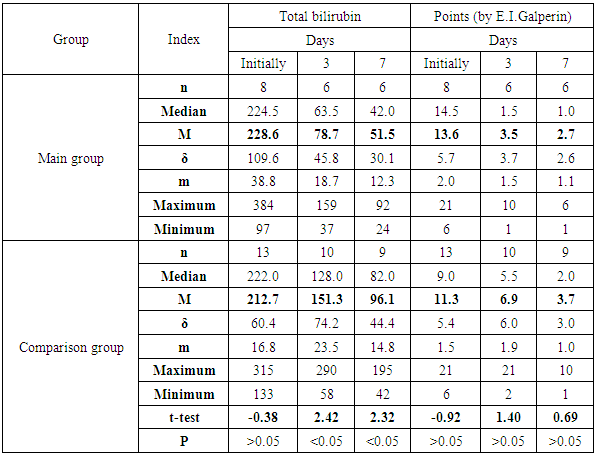
- Table 3 shows the dynamics of total bilirubin depending on the patient's initial class according to the severity of the obstructive jaundice clinical course. So, according to the baseline indicators of total bilirubin in classes "B" and "C" the compared groups were representative, with a coefficient of representativeness of 1.54.
|
|
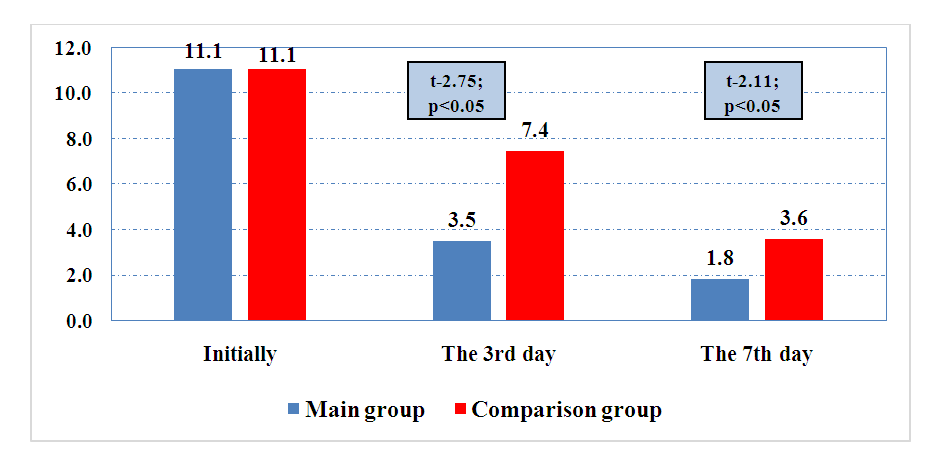 | Figure 1. The dynamics of the obstructive jaundice severity in points according to E.I. Galperin |
|
|
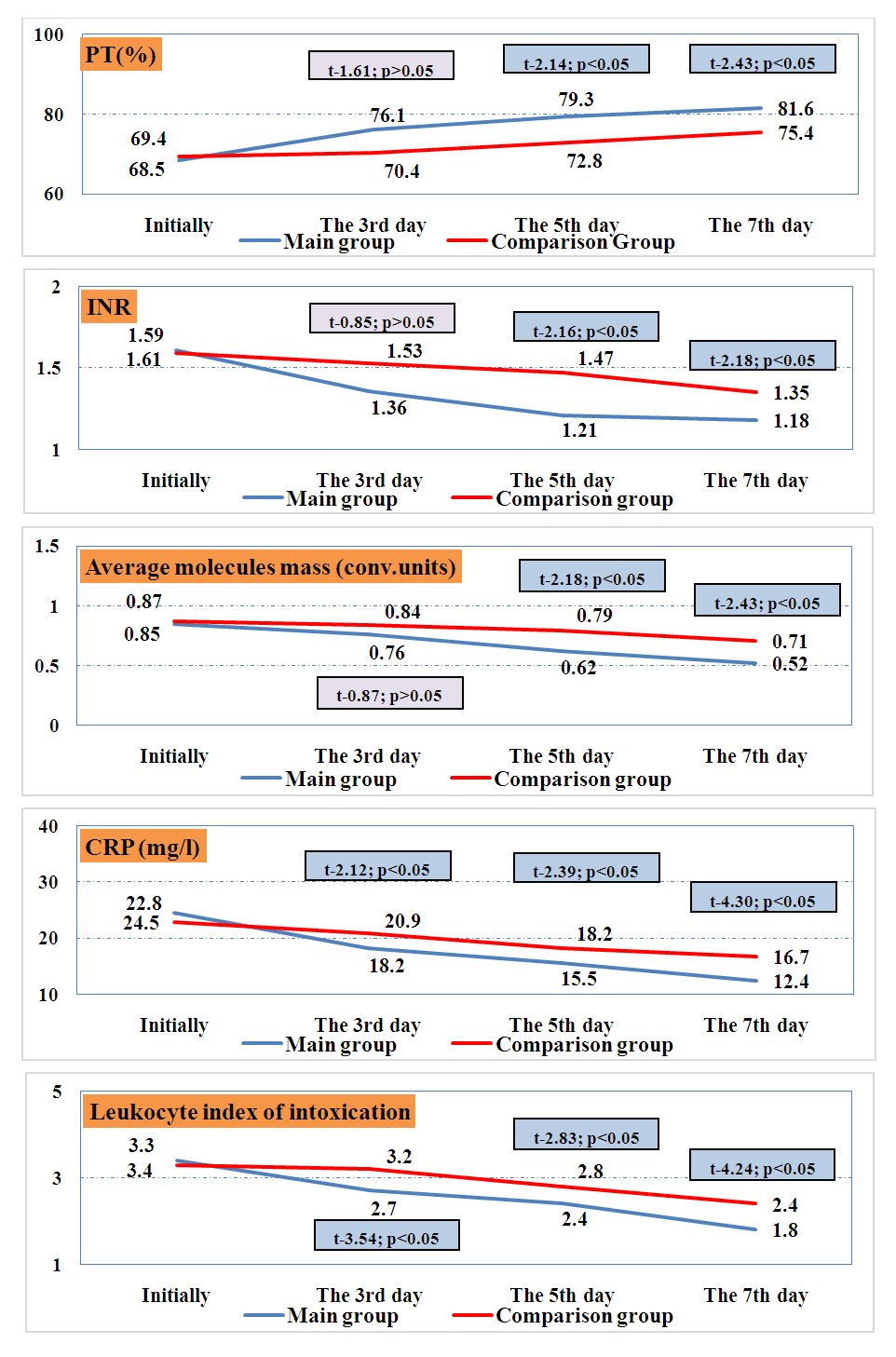 | Figure 2. Dynamics of indicators of hemostasis and inflammation markers |
4. Discussions
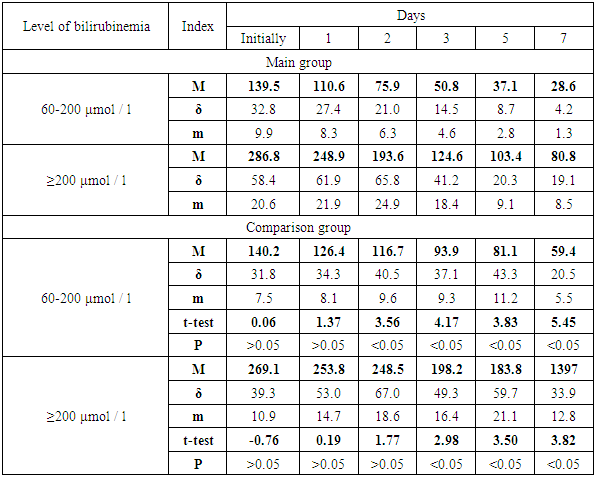
- The phenomena of endotoxicosis were eliminated immediately after sessions of modified plasma adsorption in patients of the main group. It was manifested by an improvement of the clinical condition of patients and a decrease in specific indicators of intoxication and inflammation: Average molecules mass (conventional units) - from 0.87 ± 0.11 to 0.52 ± 0.05 on the 7th day, in contrast to the comparison group, where this indicator decreased from 0.87 ± 0.11 to 7.4 ± 0.06 (with a significant intergroup difference within t-2.43 and p <0.05); C-reactive protein (CRP) (mg / l) decreased from 24.3 ± 1.2 to 12.4 ± 0.6 on the 7th day, in contrast to the comparison group, where this indicator decreased from 22.8 ± 1.4 to 16, 7 ± 0.8 (with a significant intergroup difference within t-4.40 and p <0.05); Leukocyte index of intoxication - from 3.4 ± 0.2 to 1.8 ± 0.1 on the 7th day, in contrast to the comparison group, where this indicator decreased from 3.4 ± 0.2 to 2.4 ± 0.1 ( with a significant intergroup difference within t-2.18 and p <0.05) (Fig. 2).
5. Conclusions
- The use of the improved technique of hyperbaric plasma adsorption in the complex treatment of the complicated course of obstructive jaundice had allowed to accelerate the regression of hyperbilirubinemia from 201.5 ± 19.0 to 75.4 ± 11.3 μmol / L by the 3rd day after choledocholithiasis. At a standard conservative therapy the decrease in these indicators was from 194.3 ± 13.2 to 131.5 ± 13.1 μmol / L (t = 3.24; p <0.05). Accordingly, a more intense decrease in the severity of the patient's condition was noted (from 11.1 ± 1.3 to 3.5 ± 1.0 points versus - from 11.1 ± 0.9 to 7.4 ± 1.0 points; t = 2, 75; p <0.05). The use of the improved technique of hyperbaric plasma adsorption also improved hemostasis indices (INR and PT with a significant improvement on the 5th day and inflammation markers (average molecules mass, C-reactive protein and leukocyte index of intoxication with a significant improvement on the 3rd -5th days).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML