-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(10): 788-795
doi:10.5923/j.ajmms.20201010.14
Received: Aug. 8, 2020; Accepted: Oct. 6, 2020; Published: Oct. 17, 2020

Predictive Value of Inflammatory Mediators and Effectors in Coronary Atherosclerosis - Its Link with Adverse Outcomes of Percutaneous Coronary Intervention
F. G. Nazirov, Z. P. Khaybullina, S. D. Abdullaeva
State Institute “Republican Specialized Scientific-Practical Medical Center of Surgery Named after Academician V. Vakhidov”, Tashkent, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

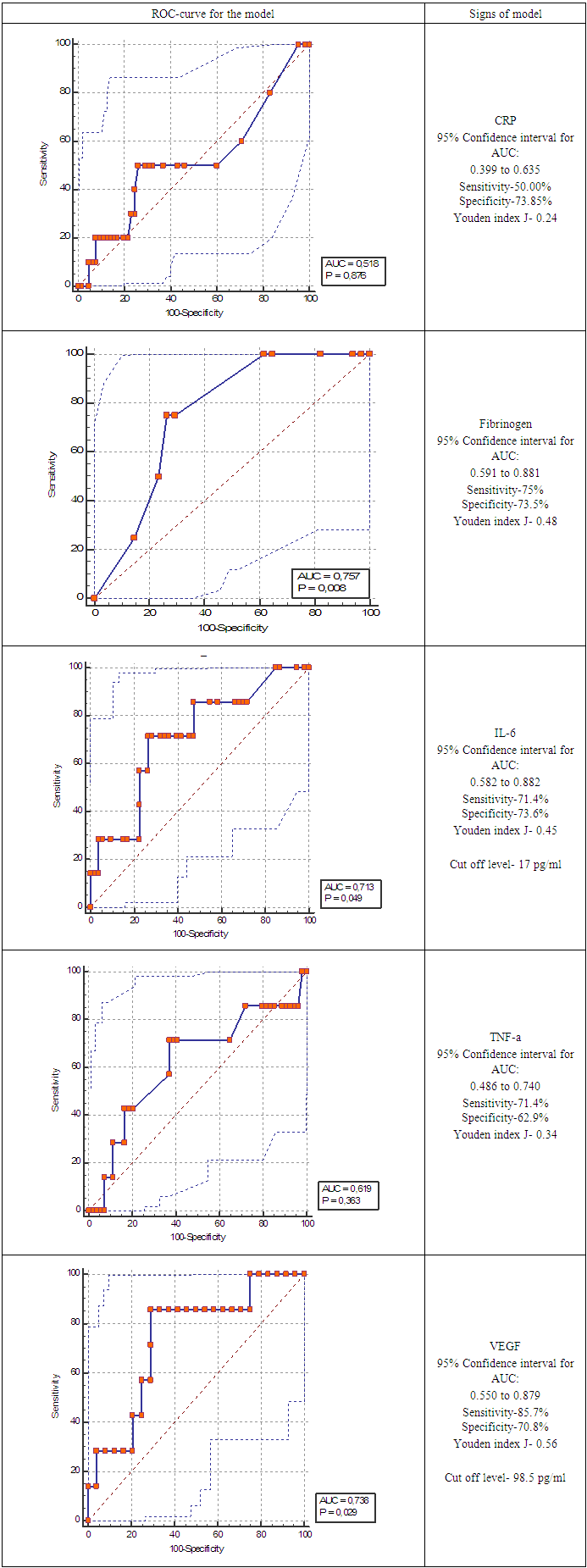
Introduction. Progress of interventional cardiology causes decrease of CHD complications, but new problems such as late thrombosis and stent restenosis, as well as neoarterogenesis were come in sight. According the literature data, stent thrombosis after percutaneous coronary intervention (PCI) developed in 0,5-1,5% of cases, restenosis if stent due neointimal hyperplasia a – in 2-10%, frequency of recurrent coronary interventions – 6-23%, that depends on type of stent (drug eluting stents with everolimus or bare metalic stents). The “latecatchup” fenomen caused weak and long inflammation, that can cause this complications. Aim of research was to study the level of inflammatory effectors and mediators in 164 patients with coronary atherosclerosis and to establish their prognostic value in major adverse coronary events (MACE) development in the long-term period after the percutaneous coronary intervention (PCI). Material and methods. The study included 164 patients with coronary atherosclerosis (CA), who were treated at the State Institution “Republican Specialized Scientific Practical Medical Centre of Surgery named after academician V. Vakhidov” in the period from 2012-2017. All patients had CHD, stable angina of functional class 3 (FC-III) according to the classification of The Canadian Cardiovascular Society (CCS). ROC – analysis was performed and area under curve were evaluated for CRP, VEGF, TNF-a, IL-6. Results. According to the results of ROC-analysis, the following markers have a predictive value in determining the risk of MACE 12 months after the PCI: baseline level of VEGF, IL-6; the threshold level for predicting an unfavorable long-term PCI result for IL -6 - is more than 17 pg/ml; for VEGF - more than 98.5 pg/ml. An increase in the concentration of CRP from 1 to 5 days after PCI, as well as a consistently high level of IL-6 and TNF-a within 5 days after PCI are associated with a high risk of MACE; high quality test found for CRP delta between 1 and 5 days after PCI (AUC=0.809 (95% CI: 0.686 to 0.899), with 71% sensitivity, 98% specificity.
Keywords: Coronary heart disease, Proinflammatory cytokines, Percutaneous coronary intervention, MACE
Cite this paper: F. G. Nazirov, Z. P. Khaybullina, S. D. Abdullaeva, Predictive Value of Inflammatory Mediators and Effectors in Coronary Atherosclerosis - Its Link with Adverse Outcomes of Percutaneous Coronary Intervention, American Journal of Medicine and Medical Sciences, Vol. 10 No. 10, 2020, pp. 788-795. doi: 10.5923/j.ajmms.20201010.14.
Article Outline
1. Introduction
- According to a World Health Organization (WHO) report, there were more than 56.4 million deaths worldwide, coronary heart disease (CHD) was the cause of 15 million deaths from this in 2017 [1]. The survival rate of patients with CHD for 10 years with functional class I (FC) is 54.6%, with FC-II – is 46.2%, FC -III – is 35.7%, with FC IV -20.6%. Mortality within 5 years with a single-vessel lesion of coronary vessels is 10.2%, for two-vessel lession – is 11.8%, and 20% for three-vessel lesion [2]. Progress of interventional cardiology causes decrease of CHD complications, but new problems such as late thrombosis and stent restenosis, as well as neoarterogenesis were come in sigh [3,4]. According the literature data, stent thrombosis after percutaneous coronary intervention (PCI) developed in 0,5-1,5% of cases, restenosis if stent due neointimal hyperplasia a – in 2-10%, frequency of recurrent coronary interventions – 6-23%, that depends on type of stent (drug eluting stents with everolimus or bare metalic stents) [5,6] The “latecatchup” phenomena caused weak and long inflammation, that can cause this complication. Inflammation is the basis of the pathogenesis of atherosclerosis and the destabilization of atherosclerotic plaque [7,8]. Epidemiological and clinical studies have shown that the baseline level of C-reactive protein (CRP), an effector of inflammation, is directly related to the risk of developing fatal and non-fatal acute myocardial infarction (AMI), stroke, as well as stenosis coronary arteries. The importance of an increase in the inflammatory mediator interleukin-6 (IL-6) [9,10] for myocardial damage has been proved, since IL-6 in excessive concentration destroys the intercellular connections of cardiomyocytes and fibroblasts, disrupts the structural and functional properties of the extracellular matrix [10]. The commonality of inflammation and atherogenesis from a pathophysiological point of view is quite natural, since both syndromes form the same cells: endothelial and smooth muscle, fibroblasts, monocytes and macrophages, neutrophils, platelets and, to a lesser extent, T and B lymphocytes [11,12]. In addition, the inflammatory response can aggravate the atherosclerotic process, affecting the movement of lipoproteins within the artery, because inflammatory mediators - tumor necrosis factor alpha (TNF-a), interleukin-1 and macrophage colony-stimulating factor - increase the affinity of low-density lipoproteins (LDL) for endothelium and smooth muscle cells, increase the transcription of the LDL receptor gene [13,14]. After binding to scavenger receptors in vitro, the modified LDL initiates a series of intracellular events that include the formation of urokinase and inflammatory cytokines such as IL-1, IL-6, etc. [14] Oxidative stress (OS), as a universal mechanism of cellular damage and a significant factor in atherogenesis, is closely associated with inflammation through the intersection of signaling pathways through reactive oxygen species (ROS) [15]. Excessive generation of reactive oxygen species (ROS) causes oxidative modification of LDL, as well as nucleotides in hypoxia-sensitive elements (promoters) of hypoxia-inducible genes: vascular-endothelial growth factor (VEGF) gene, heme oxygenase -1, endothelin -1 [12], as well as oxidative modification of cellular DNA. The presence of defective DNA leads to excessive activation of poly adenosyl ribose polymerase (PARP), which leads to oxidation of NAD and depletion of ATP reserves, which further aggravates its deficiency in cells, especially in cardiomyocytes during hypoxia [10] in patients with CHD. Prognostic implications of percutaneous coronary interventions can be performed according to the appropriate use criteria for coronary revascularization [16,17]. Long term prognosis of PCI should to be evaluated according multidisciplinary approach [18,19]. Aim of research was to study the level of inflammatory effectors and mediators in coronary atherosclerosis and to establish their prognostic value in major adverse coronary events (MACE) development in the long-term period after the percutaneous coronary intervention (PCI).
2. Materials and Methods
- There were examined 164 patients with coronary atherosclerosis (CA), who were treated at the State Institution “Republican Specialized Scientific Practical Medical Centre of Surgery named after academician V. Vakhidov”" in the period from 2012-2017. All patients had CHD, stable angina of functional class 3 (FC-III) according to the classification of The Canadian Cardiovascular Society (CCS). The average age of patients with CA was 60.6 (95% CI: 58.4-62.7) years; there were 117 (71.3%) men, 47 (28.7%) women. To assess the state of the coronary arteries and the contractility of the left ventricular myocardium, the interventional cardiologist (the chief of department – professor M.M. Zufarov) performed selective coronary angiography and left ventriculography (CVG) in all patients, which made it possible to identify patients with 1, 2, 3 vascular lesions of the coronary arteries, microvascular angina; determine the number of affected segments of the arteries, the degree of narrowing of their lumen, or chronic occlusion. The criteria for inclusion in the study were the presence of stable angina pectoris FC-III according to CSS.Exclusion criteria: acute myocardial infarction (AMI), including those suffered in the last 2 months, unstable angina pectoris, and CHD combined with pathology of heart valves, cardiomyopathies. According to international and domestic standards, patients received double antiplatelet therapy with clopidogrel and aspirin as prescribed by a cardiologist.According CVG results, 16 patients had microvascular lesions of the coronary vessels, 40 patients had indications for surgery coronary artery bypass grafting, that’s why PCI with the installation of “Ultimaster”, “Resolute-onix”, “Resolute-integrity” stents was performed in 108 patients. MACE was assessed in patients who underwent PCI 12 months after the intervention. In the long-term postoperative period, the survival rate, the incidence of adverse clinical events (death, nonfatal AMI and relapse of angina pectoris, the need for repeated revascularization), as well as the progression of coronary atherosclerosis in the arterial segments not associated with stenting were assessed.CRP level, lipid profile parameters (high density lipoprotein cholesterol - HDL, triglycerides - TG), glucose (glu), uric acid (MC) were determined on an automatic biochemical analyzer Vitros-350 (USA). The concentration of malonic dialdehyde (MDA) was determined by the thiobarbituric acid test. IL-6, tumor necrosis factor – alpha (TNF-a), VEGF, N-terminal fragment of brain natriuric peptide precursor (NTproBNP) were determined by ELISA using reagent kits manufactured by Vektor-BEST (Russia) on an ELISA analyzer ST-360 (China). Statistical data processing was carried out using the Medic-Calc software package, ROC – analysis was performed and area under curve were evaluated.
3. Results and Discussion
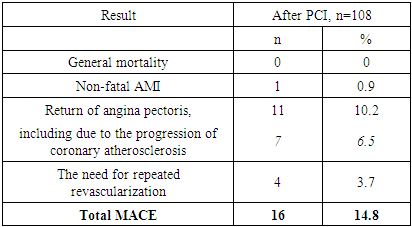
- Hemodynamically significant stenosis of the coronary arteries was detected in 148 out of 164 patients with CHD stable angina (SA) FC-III, since 16 patients had microvascular lesion of the coronary vessels. According to the number of involved vessels, the patients were distributed as follows: 37 (22%) had 1 vascular lesion, the rest had two and three-vascular lesions (Fig. 1).
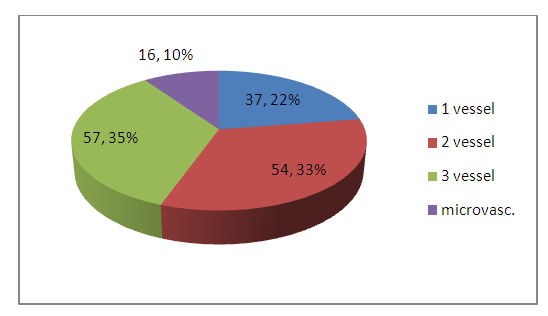 | Figure 1. Distribution of patients by type of coronary artery disease |
|
|
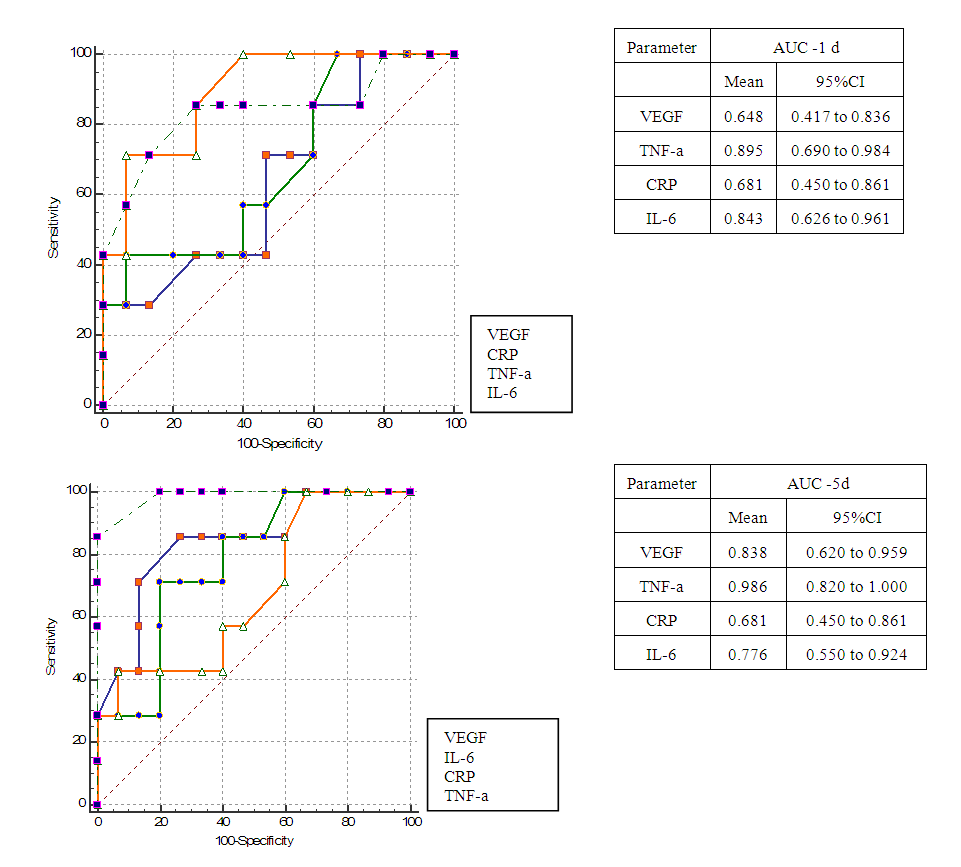 | Figure 2. Predictive quality of the model for inflammatory factors over time after PCI |
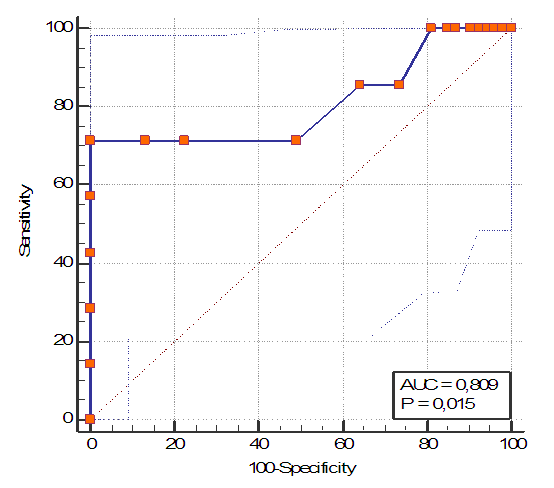 | Figure 3. Predictive model quality for delta CRP |
4. Discussion
- The activation of inflammation can be triggered by various factors, including, in addition to direct trauma to the vessel during PCI, there can be an unfavorable initial metabolic background, namely, excessive generation of reactive oxygen species, hyperproduction of pro-inflammatory cytokines accompanying metabolic syndrome. In this regard, we studied the correlations between the inflammatory factors - CRP, IL-6, TNF-alpha, and VEGF with indicators of oxidative stress (MDA), with indicators of cardiac function (EF, NTproBNP), and metabolic factors - the level of glycemia, HDL, TG, cholesterol, SAD. In patients with coronary atherosclerosis, a strong direct correlation was found between the level of CRP and the level of glucose, triglycerides, and uric acid: for CRP/Glu r=0.86; p<0.05; for CRP/TG: r=0.78, p<0.05; for CRP/MK r=0.88, p<0.05; and the relationship between CRP/HDL was negative of medium strength (r=-0.33 p<0.05). It is corresponding with Windecker S et al data [20]. The relationship between TNF-a and dyslipidemia parameters was of moderate strength (direct for TNF/TG-r = 0.51 and inverse for TNF/HDL-r=-0.48), which indicates a significant contribution of lipid metabolism disorders to the development of systemic inflammation in CHD. It is noteworthy that in microvascular angina, the correlations between the factors of inflammation and the parameters of lipid metabolism: CRP/TG and TNF/TG were direct strong reliable: r=0.88 and r=0.92, respectively. This indicates the interdependence of systemic inflammation and metabolic disorders - dyslipidemia, hyperuricemia, and glycemia in CHD. At the same time, in CHD, the relationship between CRP and markers of oxidative stress was insignificant, however, the MDA level directly correlated with MC, which has antioxidant properties (MDA/MC r=0.41, P<0.05); the MDA/HDL link was weak inverse (r=-0.23, P<0.05), and the MDA/glu link was r=0.03, P>0.05. These results indicate that oxidative stress in CHD occurs in parallel with systemic inflammation, regardless of the presence of MS components. The correlation between MDA and the VEGF endothelial state index, NTproBNP marker of left ventricular distension, as well as the index of myocardial contractility - EF was studied. It was revealed that the intensity of OS in CHD is associated with endothelial dysfunction, which develops as a result of hypoxia, and excessive production of APE. At the same time, impaired myocardial blood supply in 2- and 3-vascular lesions, as well as in microcirculatory (non-obstructive) IHD is characterized by equally intense OS, and the MDA/VEGF correlations in 3-vascular lesions were r=0.40, p<0.05 ), with microvascular lesions were r = 0.81; p <0.05. Correlation relationships MDA/NTproBNP were direct, weak significant (r=0.29, p<0.05 and r=0.24; p<0.05) in patients with coronary artery disease with macro- and microvascular lesions. The relationship between MDA/EF was mean inverse force significant (r=-0.39, p<0.05 and r=-0.45; p<0.05) in patients with coronary artery disease with obstructive and microvascular coronary artery disease, respectively. The relationship between EF/TNF was a weak straight line (r=0.11), and TNF/NTproBNP was of medium strength (r=0.67). This indicates a close connection between inflammation and myocardial dysfunction at the cellular level, while at the organ level it is less pronounced. That is, an increase in TNF in the blood is accompanied by an increase in the stretching of the tissues of the left ventricular myocardium and the release of NTproBNP into the blood, and in general, the contractility of the myocardium does not suffer and weakly depends on the level of TNF. Possibly, the presence of the TNF/NTproBNP relationship is a reflection of subcellular changes in the myocardium, and a high level of TNF can be considered a predictor of impaired myocardial contractile function in CHD.
5. Conclusions
- In the patients with CHD stable angina FC-III in the case of 3 coronary vessels damage, both effectors (IL-6, TNF-a) and the mediator of inflammation CRP were increase statically significantly versus the control, which is accompanied by an increase in the marker of endothelial dysfunction and neoangiogenesis VEGF; whereas the single-vessel and microvascular lesions of the coronary arteries was accompanied with proinflammatory mediators increase only. According to the results of ROC-analysis, the following markers have a predictive value in determining the risk of MACE 12 months after the PCI: baseline level of VEGF, IL-6; the threshold level for predicting an unfavorable long-term PCI result for IL -6 - is more than 17 pg/ml; for VEGF - more than 98.5 pg/ml.An increase in the concentration of CRP from 1 to 5 days after PCI, as well as a consistently high level of IL-6 and TNF-a within 5 days after PCI are associated with a high risk of MACE; high quality test found for CRP delta between 1 and 5 days after PCI (AUC=0.809 (95% CI: 0.686 to 0.899), with 71% sensitivity, 98% specificity. In microvascular angina, the correlations between the factors of inflammation and metabolic syndrome CRP/TG and TNF-a/TG were direct strong reliable, which indicates the interdependence of systemic inflammation and metabolic disorders, their contribution to the progression of atherosclerosis.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML