Khomidova N. R., Negmatullaeva M. N., Akhmedov F. K.
Bukhara State Medical Institute, Bukhara, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Purpose of the study: To study the features of abnormalities in blood parameters and their role in predicting the development of coagulopathic obstetric bleeding. The study of erythrocyte and platelet parameters in pregnant women with a physiological course and hemodynamic disorders showed that all indicators of both groups were significantly reduced (except for the total number of platelets). the relation of the abstract indicators, but also in comparison with the data of pregnant women with a physiological course, and in 66.7% of cases these differences were significant.
Keywords:
Obstetric bleeding, Coagulopathy, Pregnancy
Cite this paper: Khomidova N. R., Negmatullaeva M. N., Akhmedov F. K., Features of Violations of Blood Parameters and Their Role in Predicting the Development of Coagulopathic Obstetric Bleeding, American Journal of Medicine and Medical Sciences, Vol. 10 No. 10, 2020, pp. 762-765. doi: 10.5923/j.ajmms.20201010.07.
1. Introduction
It has been established that obstetric bleeding is the leading cause of maternal mortality in our Republic of Uzbekistan [2,4].On the basis of many scientific works, it has been revealed that massive obstetric bleeding develops due to insufficient contractility of the spiral arteries of the uterus and impaired functional ability of the myometrium [1,3,5].Studies have established that massive obstetric bleeding is defined as blood loss in excess of 1,5% of a woman's body weight or more than 20% of the circulating blood volume with disorders in the hemostasis system and a clinical picture of hemorrhagic shock in a woman [6,8]. It is believed that physiological (permissible) blood loss is blood loss that does not exceed 0,5% of the total body weight of the examined woman [7,9].Massive bleeding is caused by a combination of several reasons and is almost always accompanied by gross violations of the hemocoagulation system. Pregnancy is accompanied by an increase in hematopoiesis, an increase in plasma volume by 2,5-3 times, respectively, the content of corpuscles and hemoglobin changes. During gestation, not only the number of blood cells changes, but also their shape and size. An increase in the size of cells enhances their aggregation, thereby increasing its viscosity [8,9].Objective: To study the features of abnormalities in blood parameters and their role in predicting the development of coagulopathic obstetric bleeding.
2. Materials and Methods
We analyzed and evaluated the indicators of peripheral blood of pregnant women (hemograms) in 110 pregnant women in the prospective group (group 2) in the third trimester of pregnancy at 34-35 weeks gestation, in a comparative aspect with the control (group 1) patients with physiological course pregnancy. The research methods were general clinical and biochemical laboratory research methods.
3. The Results of Research
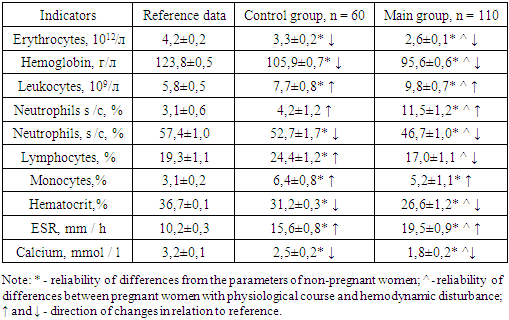
The laboratory results obtained are shown in the table below.Table 1. Comparative indices of peripheral blood (hemograms) of pregnant women under study. n = 170
 |
| |
|
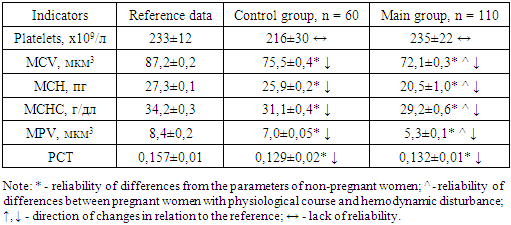
The obtained results show that the parameters of the peripheral blood of pregnant women with a physiological course (n = 60) significantly differed from those of the reference data. Thus, there was a decrease in the number of erythrocytes by 1,27 times (P <0,05) in women with physiological pregnancy and by 1,62 times (P <0,001) in pregnant women with hemodynamic disturbances in relation to the data of non-pregnant women (Table 1).We observed the same picture in terms of hemoglobin, where the decrease in women with physiological pregnancy and pregnant women with hemodynamic disturbances was, respectively, 1,17- and 1,29-fold in relation to the data of non-pregnant women (P <0,05). Leukocytes, on the contrary, were significantly increased in both compared groups (P <0,02).Stab (s /c) and segmented (s /c) neutrophils changed in different directions in the subjects, if the n / i in pregnant women of both groups were significantly increased (P <0,05 - P <0,001), then s /c neutrophils were significantly reduced (P <0,05 - P <0,001). Lymphocytes, as immunocompetent cells, are of due importance for assessing the state of functioning of the immune system. In pregnant women with a physiological course, the relative number of lymphocytes increased by 20,2% in relation to the reference data (P <0,05), and in pregnant women with hemodynamic disorders, on the contrary, lymphocytes decreased by 11,9% in relation to the reference data and by 30,3% in relation to the data of pregnant women with a physiological course (P <0,05). A slight increase in lymphocytes during the physiological course of pregnancy is explained by the activation of the compensatory-adaptive mechanisms of the body and the tension in the immune system of pregnant women.It is known that monocytes are one of the largest cells of the human body (diameter 20 μm), with an irregularly shaped nucleus. Monocytes pass into tissues and transform into macrophages, and the monocyto-macrophage system participates in the protective reactions of the human immune system.In women with a physiological course of pregnancy, monocytes increased 2,0 times in relation to the reference data – 6,4 ± 0,8% versus 3,1 ± 0,2%, respectively (P <0,001). In pregnant women with hemodynamic disturbances, an increase in the relative number of monocytes up to 5,2 ± 1,1% (P <0,05) is also observed. The detected increase in the number of monocytes is regarded by us as an indicator of an increase in the activity of nonspecific factors of the immune system during the development of a pathological process in the body of a pregnant woman.Also, attention is drawn to the hematocrit indicator (total volume of erythrocytes), which turned out to be significantly reduced in women with physiologically proceeding pregnancies and pregnant women with hemodynamic disturbances in relation to the reference data (31,2 ± 0,3% and 26,6 ± 1,2%, respectively). vs. 36,7 ± 0,1%, (P <0.05 - P <0,001). Studies have established that the erythrocyte sedimentation rate (ESR) allows one to judge the activity of the pathological (inflammatory) process.ESR in pregnant women with a physiological course, although significantly increased by 1,53 times in relation to the reference (P <0,05), is at the level of the upper limits of the norm, which indicates the absence of a pathological process, but the presence of signs of a pre-pathological state in these women. In pregnant women with hemodynamic disturbances, ESR is reliably 1,91 and 1,25 times higher, respectively, than in healthy non-pregnant women (P <0.001) and pregnant women with a physiological course (P <0,05), which is a harbinger of a pre-pathological state in this category women.Thus, a comparative analysis of peripheral blood parameters in pregnant women with physiological course and hemodynamic disorders showed that all the studied 10 parameters differed significantly from the reference data. If the indices of the number of erythrocytes, hemoglobin of s / c neutrophils, hematocrit and calcium in the peripheral blood were reduced, then the numbers of leukocytes, s / c neutrophils, monocytes, ESR were significantly increased. Only the relative number of lymphocytes changed in different directions. The revealed violations indicate the presence of a pre-pathological condition and the development of a pathological process proceeding with a violation of hemodynamic, as well as tension in the body's immune system.Estimation of erythrocyte parameters of peripheral blood in the compared groups of pregnant women are shown in table 2.Table 2. Comparative parameters of erythrocyte and platelet parameters in pregnant women. n = 170
 |
| |
|
The results obtained show that all 5 parameters were reduced in pregnant women with physiological course and hemodynamic disorders (P <0,05 - P <0,001).MCV (mean corpuscular volume - the average indicator of the volume of the entire population of erythrocytes) was reduced in both compared groups in relation to the data of the reference indicators - respectively 75,5 ± 0,4 μm3 and 72,1 ± 0.3 μm3 versus 87,2 ± 0, 2 μm3 (P <0,05).The same downward trend was observed for the MCH parameter (mean corpuscular hemoglobin - the average hemoglobin content in the erythrocyte). If we take into account that this indicator decreases with various anemias, then its decrease in pregnant women with hemodynamic disturbances is natural, which is proved as a result of our research - respectively 20,5 ± 1,0 pg in pregnant women with hemodynamic disturbances versus 27,5 ± 0, 1 pg of reference data (decrease by 1,34 times, P <0,05).It is known that MCHC (mean corpuscular hemoglobin concentration - the average concentration of hemoglobin in an erythrocyte) shows the concentration of hemoglobin in one erythrocyte. It has been established that a decrease in MCHS is observed in diseases or conditions accompanied by a violation of hemoglobin synthesis [8,10].In our studies, it was proved that the MSCS indicator significantly decreases in pregnant women with a physiological course and hemodynamic disorders (P <0.005), that is, the tendency for a decrease in erythrocyte parameters was almost the same in the compared groups.Like erythrocyte parameters, platelet parameters also tended to decrease in pregnant women with hemodynamic disorders.The total number of platelets (PLT) in pregnant women with a physiological course decreases in relation to the data of non-pregnant women, but not significantly (216 ± 30x109 / l versus 233 ± 12x109 / l, P >0,05), and the parameters in pregnant women with hemodynamic disturbances remained at the level of normal values (P >0,05).Other platelet parameters tended to decrease significantly in relation to the reference data (P <0,05 - P <0,001).МРV (mean platelet volume - mean platelet volume) in pregnant women with a physiological course decreases by 1,20 times (P <0,05), and in pregnant women with hemodynamic disturbances by 1,58 times (P <0,001) in relation to the reference parameters.Almost identical results were obtained in terms of PCT (platelet cut) content, which a parameter is reflecting the proportion of whole blood volume occupied by platelets. The indicators of both compared groups were significantly reduced in relation to the normative values (P <0,05), and the parameters between these groups did not differ statistically significantly (P >0,05).Thus, the study of erythrocyte and platelet parameters in pregnant women with physiological course and hemodynamic disturbances showed that all indicators of both groups were significantly reduced (except for the total number of platelets), however, it should be emphasized that the indicators of women with hemodynamic disturbances were decreased more intensively, significantly differing not only in relation to the abstract indicators, but also in comparison with the data of pregnant women with a physiological course, and in 66,7% of cases these differences were significant.Thus, the revealed facts proved the negative effect of disturbances in hemodynamic parameters not only on peripheral blood parameters, but also on erythrocyte and platelet parameters. These altered erythrocyte and platelet parameters can be early markers of provoking disorders of the hemostasis system.
References
| [1] | Andrew M.Е., Paes B., Johnston M. Development of the haemostatic system in the neonate and young infant // Am. J. Pediatr. Hematol. Oncol. - 2010. - V. 12. - P.95-104. |
| [2] | Akhmedov F.K. Features of renal function and some indicators of homeostasis in women with mild preeclampsia // Europen Science Review. Austria, Vienna, 2015, № 4-5. – С. 58–60. |
| [3] | Barjaktarovic M., Steegers E.A.P., Jaddoe V.W.V., de Rijke Y.B., Visser T.J., Korevaar T.I.M., Peeters R.P. The association of thyroid function with maternal and neonatal homocysteine concentrations // J Clin Endocrinol Metab. – 2017. - N102(12). – P.4548-4556. |
| [4] | D.I. Tuksanova. Features of the state of homeostasis and cardiohemodynamic parameters in women with physiological pregnancy // Tibbiyotda yangi kun. - Tashkent, 2019. - No. 1 (25). - S.159-163. |
| [5] | Koloskov A.V. Hemostasis in pregnant women and hereditary disorders of the blood coagulation system // Health and education in the XXI century. - 2017. - Vol. 19. - N6. - S.50-54. |
| [6] | Castelnuovo A., Agnoli C., de Curtis A. Elevated levels of D-dimers increase the risk of ischaemic and haemorrhagic stroke Findings from the EPICOR Study // Thromb Haemost. - 2014. - N112. - P.941-946. |
| [7] | Chen Y., Lin L. Potential Value of Coagulation Parameters for Suggesting Preeclampsia During the Third Trimester of Pregnancy // Am J Med Sci. – 2017. - N354(1). – P.39-43. |
| [8] | Federici AB, Konigs C, James AH. Contemporary issues in the management of von Willebrand disease // Thromb Haemost. – 2016. - N116(l). – P.18-25. |
| [9] | Govorov I., Lofgren S., Chaireti R., Holmstrom M., Bremme K., Mints M. Postpartum hemorrhage in women with Von Willebrand disease - a retrospective observational study // PLoS One. – 2016. - N11(10). - e0164683. |
| [10] | Kaminski T.W., Pawlak K., Karbowska M., Mysliwiec M., Grzegorzewski W., Kuna J., Pawlak D. Association between uremic toxin-anthranilic acid and fibrinolytic system activity in predialysis patients at different stages of chronic kidney disease // Int Urol Nephrol. – 2018. - N50(1). – P.127-135. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML