Khomidova N. R., Akhmedov F. K.
Department of Obstetrics and Gynecology, Bukhara State Medical Institute, Bukhara, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Goal: Study the role of hemodynamic markers in predicting and preventing obstetric bleeding. To study and determine predictive markers of hemostatic disorders, we conducted a comprehensive examination of pregnant women in the third trimester of pregnancy at 34-35 weeks gestation. This group consisted of 110 patients in the risk group (group 2) on the development of the initial stages of thrombophilia and the predicted development of obstetric bleeding during childbirth due to thrombogemoragic syndrome. The subject of the study was blood serum of patients, ultrasound, Doppler evaluation of the Central hemodynamics of the mother and regional (utero-placental) blood flow. General clinical and laboratory, functional (ultrasound, Doppler) biochemical and statistical methods were used.
Keywords:
Obstetric bleeding, Hemostasis, Central hemodynamics
Cite this paper: Khomidova N. R., Akhmedov F. K., The Role of Markers of Violations of Central Maternal Hemodynamics and Regional (Utero-Placental - Fetal) Blood Flow in Predicting Obstetric Bleeding, American Journal of Medicine and Medical Sciences, Vol. 10 No. 10, 2020, pp. 759-761. doi: 10.5923/j.ajmms.20201010.06.
1. Introduction
One of the main tasks of the health authorities and institutions of our Republic of Uzbekistan is to prevent and reduce maternal and infant mortality, since these indicators reflect the level of development of the state and its health care. In our country, targeted reforms are being carried out to raise medical care to a new level, especially with a preventive focus.According to the development action strategy of the Republic of Uzbekistan for 2017-2021, tasks have been defined to strengthen family health, protect motherhood and childhood, and take large - scale measures to reduce maternal mortality.In the Republic of Uzbekistan, among the causes of maternal mortality, bleeding occupies the first place and often competes with hypertensive conditions during pregnancy.According to WHO it is massive obstetric bleeding (exceeding 1.5% of body weight) is life-threatening. In this regard, in modern obstetrics, the issues of forecasting and early diagnosis of thrombophilic conditions, their significance in the development of obstetric massive bleeding and finding ways to prevent them remain very relevant.Identification of significant prognostic markers of the development of this pathology and the use and implementation of etiopathogenetic preventive medical measures are the main strategy for improving the outcome of pregnancy and childbirth, reducing disability among women of reproductive age. To influence pregnancy outcomes, it is necessary to understand the importance of risk value in relation to medical practice and timely routing of the patient. Successful obstetric management can be when the doctors in a timely manner will be to use methods allowing to predict the occurrence of pregnancy complications. Predicting bleeding during childbirth allows you to determine the most rational tactics of labor management, take into account and use for early diagnosis all markers of violations of the mother's Central hemodynamics and regional MP blood flow and hemostasis system.Objective: study the role of hemodynamic markers in predicting and preventing obstetric bleeding.
2. Materials and Methods of Research
Study and determine predictive markers of hemostatic disorders, we conducted a comprehensive examination of pregnant women in the third trimester of pregnancy at 34-35 weeks gestation. This group consisted of 110 patients in the risk group (group 2) on the development of the initial stages of thrombophilia and the predicted development of obstetric bleeding during childbirth due to thrombogemoragic syndrome.The subject of the study was blood serum of patients, ultrasound, Doppler evaluation of the Central hemodynamics of the mother and regional (utero-placental) blood flow. General clinical and laboratory, functional (ultrasound, Doppler) biochemical and statistical methods were used. To study the parameters of the Central hemodynamics of the mother and regional – utero - placental blood flow, we conducted Doppler studies of all pregnant women in the prospective study group. The control group consisted of 60 pregnant women with a physiological course of pregnancy-group I.
3. Research Result
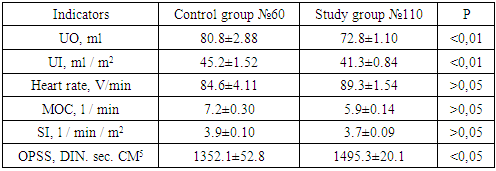
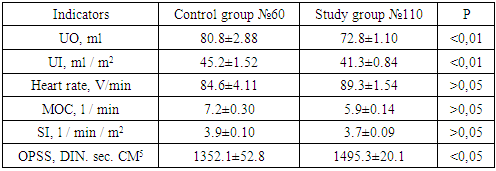
The study of dopplerometry indicators in pregnant women at risk at 34-35 weeks gestation and a comparative assessment of these indicators indicated changes in them, which is shown in the table below. Where, for comparison, we also present control values of the data obtained for pregnant women with the physiological course of gestation.Table 1. CG indicators in pregnant women of the study group at the gestation period of 34-35 weeks. P=170
 |
| |
|
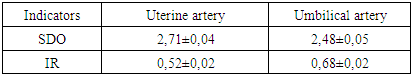
From the results obtained, it can be seen that in pregnant women at risk compared to the control group, all indicators of Central hemodynamics are subject to changes for the worse. Statistically significant differences between the values of the control group are the indicators of one-time productivity (UO,UI), which were reduced by 10.0 and 3.9, respectively. Minute heart performance decreased by 1.3 despite an increase in heart rate by 4.7. a Particularly significant role was played by an increase in heart rate by 143.2 DIN. sec. cm-5, which may indicate a significant constriction of arterioles in the entire circulatory system, especially the placenta, which was accompanied by a decrease in utero-placental - fetal blood flow and a violation of fetal hemodynamics.Data on average IR values and velocity curves of utero-placental-fetal blood flow are presented in Table 2.Table 2. Indicators of utero-placental and fetal blood flow in pregnant women of the study group at the gestation period of 34-35 weeks
 |
| |
|
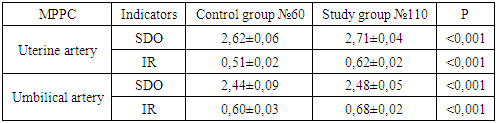
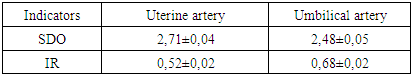
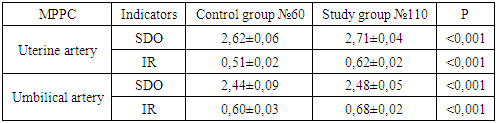
As can be seen from table no., these dopplerograms reflected changes in blood flow velocity curves in the uterine and umbilical arteries in pregnant women at risk for obstetric bleeding, mainly due to the diastolic component and increased OPSS.Table 3. Comparative evaluation of dopplerometry data in the study groups. P=170
 |
| |
|
According to the data given in the above table, it is not difficult to notice that pregnant women in the risk group with an increase in gestation against the background of increased OPSS continue to increase vascular spasm covering mainly the arterial segment, which provokes a deterioration of blood flow in the placental system. SDO and IR in the uterine artery increased by 3.4%, IR by 21.5%, SDO in the umbilical artery increased by 1.6%, and IR by 13.3%, respectively.Based on the data obtained, we tried to find the most reliable criteria that reflect the state of maternal blood circulation and utero–placental blood flow. This criterion turned out to be an indicator that, indicating the state of peripheral blood circulation, had a direct correlation with regional utero-placental blood flow. Taking into account the complexity of determining OPSS using a simple calculation method in maternity hospitals and the high correlation of this indicator with placental blood flow indicators, it will be possible to confidently recommend monitoring the OPSS indicator as a marker for evaluating circulatory disorders in the utero-placental system, but with parallel determination of the values of SDO and IR of the uterine artery. Changes in blood flow in the utero-placental - fetal system, respectively, led to morpho-functional disorders of the placenta. According to the ultrasound study, areas of infarction zones, calcification in 75 pregnant women were identified and clinically showed signs of its morpho-functional insufficiency.We interpreted these changes as spasm of arterial vessels of the placental complex and violations of circulatory adaptation of the hemostatic system. The leading preclinical manifestation of DIC-syndrome was intravascular changes in placental vessels, concentrated in the placental area of the myometrium, which were found according to ultrasound studies indicating infarction zones due to micro and macro thrombosis. Selective damage to the uterus may be the main cause of the development of disorders of the hemostatic system and may be clinically manifested by thrombohemorrhagic syndrome.Violation of the Central hemodynamics of the mother and regional utero-placental - fetal blood flow creates a premorbital background for thrombohemorrhagic complications due to violation of hemostasis parameters. Violation of hemostasis increases the risk of layering of massive bleeding during childbirth and cesarean section. Many researchers have proved that pregnancy complications are the result of placental ischemia with impaired endothelial function and a multi-system response of the maternal body (). This process provokes the development of generalized microangiopathy and thrombophilia.In acting practice, the greatest danger is the hidden defects of the hemostatic system, which can become the main cause of an unfavorable outcome of pregnancy and childbirth.
4. Conclusions
Thus, taking into account the complexity of determining OPSS using a simple calculation method in maternity facilities and the high correlation of this indicator with placental blood flow indicators, it will be possible to confidently recommend monitoring the OPSS indicator as a marker for evaluating circulatory disorders in the utero - placental system, but with parallel determination of the values of SDO and IR of the uterine artery.
References
| [1] | Belkania G. S., Konkov D. G., Dilenyan L. R., Razzhivin A. P., puhalskaya L. G., Bocharin I. V., Tupitsyn V. P., Romanova A. A., Sukhov P. A., Korepanov S. K. a New view on blood circulation in pregnant women-anthropophysiological diagnostics of hemodynamic support of pregnancy // Modern problems of science and education. – 2017. – № 5. |
| [2] | Voskresenskaya N. L., Okhapkin M. B. interrelations of indicators of Central and peripheral hemodynamics of the mother during pregnancy complicated by arterial hypertension.Journal of experimental, clinical and preventive medicine. - 2018. - №15. - p. 487-497. |
| [3] | Okhapkin M. B., Khitrov M. V., Shatskaya O. Yu., Bryantsev M. D. / Evaluation of indicators of Central hemodynamics in the prognosis of the course and outcomes of pregnancy / / XI XI XI "mother and child". - M., 2010. - Pp. 171-172. |
| [4] | Kleshchenogov S. A. the Relationship of Central hemodynamic and heart rate variability of the mother during normal and complicated pregnancy [Text] / S. A. Kleshchenogov, O. I. Kanikowska // Bulletin SB RAMS. - 2019. - No. 3. - S. 115-121. |
| [5] | Makarov, O. V. Peculiarities of Central hemodynamics in pregnant women with arterial hypertension / S. V. Makarov, N. N. Nikolaev, E. V. Volkova // Obstetrics and gynecology. 2013. - no. 4. - P. 18-22. |
| [6] | Stolyarov G. S., Minaeva O. V., Fominova G. V., Tyurina E. P., Amri M. S., Kosenko Yu. y., Zakharov A. A., Fominova I. S., Ekomaskin S. V., Belozerova K. S., Kosova A.V., Lyalichkina N. A. Features of the state of Central hemodynamics and hemostasis in pregnant women with preeclampsia // Modern problems of science and education. - 2018. - № 3. P. 18-22. |
| [7] | Emelyanova D. I. Features of Central hemodynamics in pregnancy against the background of chronic arterial hypertension [Text] / D. I. Emelyanova, N. V. Yagovkina, S. A. Dvoryansky // Scientific Bulletin of the Belgorod state University. - Belgorod. – 2014. - №11(182). – pp. 98-102. |
| [8] | Emelyanova, D. I. Correlation of the type of regulation of Central hemodynamics and birth outcomes in women with hypertension / D. I. Emelyanova / / XVII all-Russian medical and biological conference of young researchers. Saint Petersburg, 2014, pp. 150-152. |
| [9] | Valensise H., Novelli G., Vasapollo B. et al. Systolic and diastolic function of the mother's heart: relationship with utero-placental resistance. Doppler and echocardiographic longitudinal study / / ultrasound of obstetrics. Gynecology. – 2018. – №15. – 487-497. |
| [10] | Perry H., Stirrup, O., Gutierrez, J., Vinayagam D., Thilaganathan B., Khalil. Influence of maternal characteristics and gestational age on hemodynamic parameters: reference ranges of the NICOM device.. Ultrasound Obstetrician Gynecol. 2019 November; 54 (5): 670-675. Dpi: 10.1002 / UOG. 20179. Epub 2019 Oct 6. PMID: 30548496. |
| [11] | Perry G., Lehmann H., Mantovani E., B. Thilaganathan, Khalil A. correlation between Central and uterine hemodynamics in hypertensive disorders during pregnancy. Ultrasound Obstetrician Gynecol. 2019 July; 54 (1): 58-63. Dpi: 10.1002/UOG. 19197. PMID: 30084237. |
| [12] | Hassan H., Malk R., Abdelhamed A., Genedy A., “Infection Control Knowledge and Practices: Program Management in Labor Units According to Standard Infection Control Precautions in Northern Upper Egypt.” American Journal of Nursing Research, 2020; 8(4): 412-425. doi: 10.12691/ajnr-8-4-1. |
| [13] | Hassan H., Mohamady Sh., & Abd El-Gawad N. Protocol for improving nursing performance towards placental examination at labor units. Clinical Nursing Studies, 2017; 5(2): 1-11. http://dx.doi.org/10.5430/cns.v5n2p1. |
| [14] | Brahim H., Elgzar W., Hassan H. Effect of Warm Compresses Versus Lubricated Massage during the Second Stage of Labor on Perineal Outcomes among Primiparous Women. IOSR Journal of Nursing and Health Science. 2017; 6(4): 64-76. doi: 10.9790/1959-0604056476. |
| [15] | Phillips R. A., Ma Z., Kong B., Gao L. maternal hypertension, advanced Doppler hemodynamics and therapeutic accuracy: principles and illustrative cases. Curr Hypertens Republic 2020 July 13; 22(7): 49. doi: 10.1007/s11906-020-01060-2. PMID: 32661569. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML