-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(9): 705-710
doi:10.5923/j.ajmms.20201009.16
Received: Jul. 26, 2020; Accepted: Aug. 25, 2020; Published: Sep. 15, 2020

Disturbance of Acid-Base Balance in Surgical Treatment of Septic Endocarditis
Sh. A. Islambekova, L. A. Nazirova, Sh. M. Aliev
Republican Specialized Center of Surgery Named after Academician V. Vakhidov, Tashkent, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

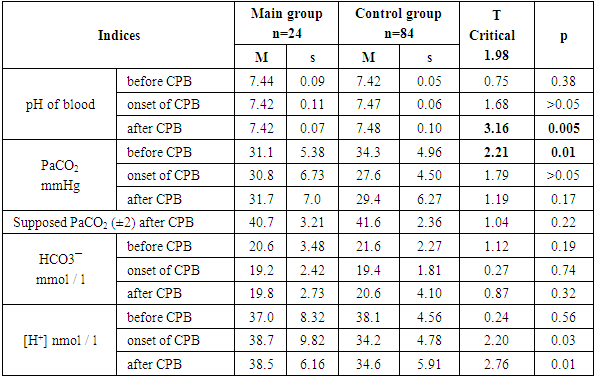
Aim of our study was to assess the acid-base state (ABS) in patients with septic endocarditis (SE) in perioperative period. Material and methods. The research has been based on the analysis of 108 patients with septic endocarditis. The main group included 24 patients who used zero balance ultrafiltration (Z-BUF) of blood during cardiopulmonary bypass (CPB). Control group included 84 patients who were not used Z-BUF. Cardiopulmonary bypass was performed on a “Sarns Terumo” apparatus. Blood analysis of the acid-base state in all groups was carried out on ABL-735 apparatus produced by Radiometer (Denmark). Statistical processing was carried out using the MS Excel applied software package, STATISTICA 10.0. To assess the normality of the sample distribution, the Kolmogorov-Smirnov tests for samples n> 50 and Shapiro-Wilk tests for samples n <50 were used. Statistical hypotheses about the equality of general means were tested to identify the difference between the groups. Quantitative data have been presented as М ± σ, logical data - as a share of the total number of observations. X2 test with Yates’s correction and McNemar was used to compare qualitative features. Data were considered statistically significant at p <0.05. Results. The results of our research showed that after induction of anesthesia, patients in the groups had fully compensated chronic respiratory alkalosis. Hypocapnia was more evident in Z-BUF group and significantly differed from the comparison group (p=0.01). At the end of the cardiopulmonary bypass (CPB), the pH in the main group remained within the normal range, while in the comparison group, an increase in pH (p=0.005) towards alkalosis was revealed. Anion gap of plasma was more than 12 mEq/L in the Z- BUF group: before CPB 7 (29%), after CPB 3 (12.5%); in the comparison group: before CPB 17 (20.2%) after CPB 7 (8.3%), p>0.05. The proportion of patients with low anion gap did not increase after CPB in the Z-BUF group (before CPB (12.5%), after CPB (12.5%)), while in the comparison group, low anion gap increased from 4 (4.76%) to 22 (20.1%) cases. Conclusion. Z-BUF supports the compensatory mechanism of respiratory alkalosis in patients with septic endocarditis during cardiopulmonary bypass. Z-BUF reduces hemodilution and maintains a normal level of albumin in blood during cardiopulmonary bypass. Z-BUF reduces the level of potassium ions in blood by eliminating them during filtration, which is a necessary property during hyperkalemic cardioplegia.
Keywords: Septic, Endocarditis, Cardiopulmonary bypass, Perioperative period, Blood ultrafiltration, Respiratory alkalosis, Acid-base state, Bicarbonates
Cite this paper: Sh. A. Islambekova, L. A. Nazirova, Sh. M. Aliev, Disturbance of Acid-Base Balance in Surgical Treatment of Septic Endocarditis, American Journal of Medicine and Medical Sciences, Vol. 10 No. 9, 2020, pp. 705-710. doi: 10.5923/j.ajmms.20201009.16.
1. Introduction
- Currently, many aspects of the diagnostics and surgical treatment of septic endocarditis (SE) remain relevant. It is mainly connected with an increase of morbidity and a change in the clinical picture of this nosology. Patients are admitted to hospitals with advanced forms of endocarditis, with low myocardial reserves and with the development of life-threatening complications [1]. Kidney damage is often the first clinical manifestation of the disease and occurs from 2 to 78% [2]. Mortality among SE patients with kidney involvement is significantly higher than in patients without this complication [2]. Cardiac surgeons are faced with the question of the possibility and safety of surgical treatment in the conditions of the kidney pathology. Cardiopulmonary bypass (CPB) which is a fundamental component of cardiac surgery, has its drawbacks. Contact of blood with the surface of the extracorporeal circuit, hemodilution, hypothermia trigger the release of numerous inflammatory mediators and imbalance of cytokines and other factors that lead to endothelial damage, contraction of endothelial cells and an increase of capillary permeability [3]. Massive release of fluid from the vascular bed into the intercellular space leads to disruption of tissue metabolism, hypoxia and organs’ edema [3-4]. Improvement of surgical technique and optimization of cardiopulmonary bypass can reduce postoperative complications. The use of the method of blood ultra-filtration (UF) in the protocol of cardiopulmonary bypass is widely covered in the works of various authors [4-8]. Currently, the effectiveness of blood ultra-filtration and its effect on the function of vital organs and systems (hemodynamics, contractile function of the heart, ventilation of the lungs, cerebral blood flow, postoperative blood loss) are widely studied, but there are also conflicting opinions about their capabilities [4-8]. Thus, a number of studies have shown the role of blood UF in the increase of metabolic acidosis due to the active elimination of bicarbonate buffer [9]. According to some authors view, the use of sodium bicarbonate solutions for the correction of metabolic acidosis leads to an increase of a large amount of carbonic acid and CO2 in the blood plasma which requires an increase in the volume of pulmonary ventilation and worsens the condition of patients with respiratory failure [10]. Considering that not only the kidneys but also the lungs are damaged during SE, the correction of metabolic disorders at this pathology requires a special approach.Aim of our study was to assess the acid-base state (ABS) in patients with septic endocarditis (SE) in perioperative period.
2. Material and Methods
- The research has been based on the analysis of 108 patients with septic endocarditis: 63 (58%) males and 45 females (42%). The mean age of patients made up 41.50±11.57 years. The severity of the patients’ condition with chronic heart failure (CHF) was evaluated in accordance with the classification of CHF of the New York Heart Association (NYHA, 1994). The main group included 24 patients who received balanced blood UF during cardiopulmonary bypass (CPB). The control group included 84 patients who did not receive blood UF. There were no significant differences between the groups in age, sex, body surface area and comorbidities. Indications for blood UF during CPB were: chronic kidney disease with a decrease in the glomerular filtration rate GFR <60 ml / min / 1.73 m2, signs of kidney damage (proteinuria, leukocyturia, hematuria), an increase in the left ventricular end-diastolic volume of more than 250 ml (large inflow into the venous reservoir of the oxygenator), CPB for a long time (more than 120 min), moderate anemia, concomitant diseases and cardiorenal syndrome when there is no possibility of using diuretics. The main group significantly differed by more severe clinical course before surgery: functional class (FC) IV was detected in 6 (25%) patients and FC III in 18 (75%) patients according to NYHA, in contrast to the control group, where FC IV was recorded in 6 (7,1%) patients and FCIII in 78 (92.8%) patients according to NYHA at χ2=6,03; р<0,05. Cardiopulmonary bypass was performed on a Sarns Terumo apparatus. Membrane oxygenators "Skipper-Euroset" (Italy) were used. Blood analysis of the acid-base state in all groups was carried out on ABL-735 apparatus produced by "Radiometer" (Denmark). The collection of the ABS analysis was carried out at the following stages of perfusion: before the start of CPB for 5 min of conducting CPB; after CPB; before taking the patient out of the operating room; in the intensive care unit. The following indicators were examined in the obtained blood samples: hematological (Hb, Ht), physico-chemical (pH, BE, HCO³¯, osmolarity, pO2, pCO2, SatO2 of arterial blood), biochemical (glucose, lactate), electrolyte composition (Na+, K+, Ca²+). CPB was performed under moderate hypothermia (32°C). Blood pressure was maintained at a level not lower than 72.9 ± 6.88 mm Hg. For ultrafiltration of blood, we used HPH 700 Medtronic hemoconcentrators (USA) with a pore diameter of 65000 Da. The removed ultrafiltrate was replaced with a balanced electrolyte Ringer-Locke solution or saline (0.9% sodium chloride) with the addition of 10% 10.0 calcium chloride and 8% 50.0 sodium bicarbonate (soda) per 1000 ml of infused liquid. The following parameters were assessed to characterize the acid-base state (ACS): blood buffer systems; carbonate level (НСО3¯), standard bicarbonates (SBС), buffer bases (BE), partial pressure of carbon dioxide (рСО2), oxygen partial pressure (рО2), alkaline blood reserve, ion concentration [Н+], рН, lactic acid concentration. To evaluate metabolic acidosis, the plasma anion gap (PAG, mEq / L) and the differential coefficient were calculated using the formulas: PAG = [Na+] - ([Cl-] + [HCO3-]) and PAG/[ HCO3-], respectively. Simple types of acid-base imbalance were diagnosed based on the analysis of three parameters determined in an arterial blood sample: pH, plasma bicarbonate concentration (НСО3¯) and рСО2. Statistical processing was carried out on a personal computer - IBM Pentium with Windows 7 operating system using a package of applied software MS Excel, STATISTICA 10.0. For statistical analysis of the data, the following methods were used: parametric statistical methods (Kolmogorov-Smirnov test for samples n> 50 and Shapiro-Wilk for samples n <50). Descriptive statistics was used to detect and analyze causal relationships between variables. Statistical hypotheses about the equality of Student's t-test general means were tested to identify the difference between the groups. To compare qualitative features, a chi-square was used with Fisher's test and with Yates' correction. Data were considered statistically significant at p<0.05.
3. Results and Discussion
- The groups did not differ in the duration of CPB (main group - 87.2 ± 28.1 min, control group - 80.0 ± 25.3 min, p> 0.05) and the time of aortic clamping (main group - 66.3 ± 24, 1 min, control group - 60.4 ± 18.0 min, p> 0.05). The minimum hemoglobin during CPB in the groups was significantly different (main group: 80.0 ± 13.4 g / L; comparison group 88.7 ± 11.7 g / L; at t = 2.80; p = 0.009). In the UF group, the level of minimum hemoglobin (Hb = 80.0 ± 13.4 g / l) was sufficient for adequate oxygen delivery to tissues of DO2 and was maintained at a level above the "critical" 330 ml / min-1 / m-2 (523.0 ± 114, 7ml / min-1 / m-2.) at a CPB temperature of 32.4 ± 1.43°C. After CPB, the hemoglobin and hematocrit values in the groups did not differ statistically (p = 0.77) and the hemoglobin value was above 90 g / l.According to the analysis of the average value of ABS of blood in patients of the groups, fully compensated chronic respiratory alkalosis was revealed after induction of anesthesia. As chronic respiratory alkalosis is associated with low or normal HCO3¯ levels, and acute respiratory alkalosis is associated with high blood bicarbonate levels, a condition of chronic hypocapnia that stimulates a compensatory renal response and results in a significant decrease of [HCO3ˉ] plasma [11]. At the same time, hypocapnia was more evident in the main group and significantly differed from the comparison group (p = 0.01) (Tab. 1).
|
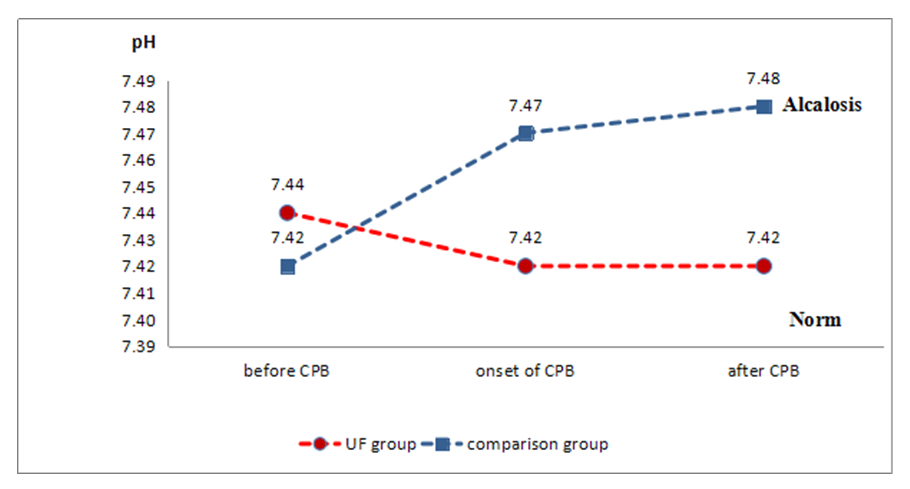 | Figure 1. Dynamics of pH in groups in the perioperative period |
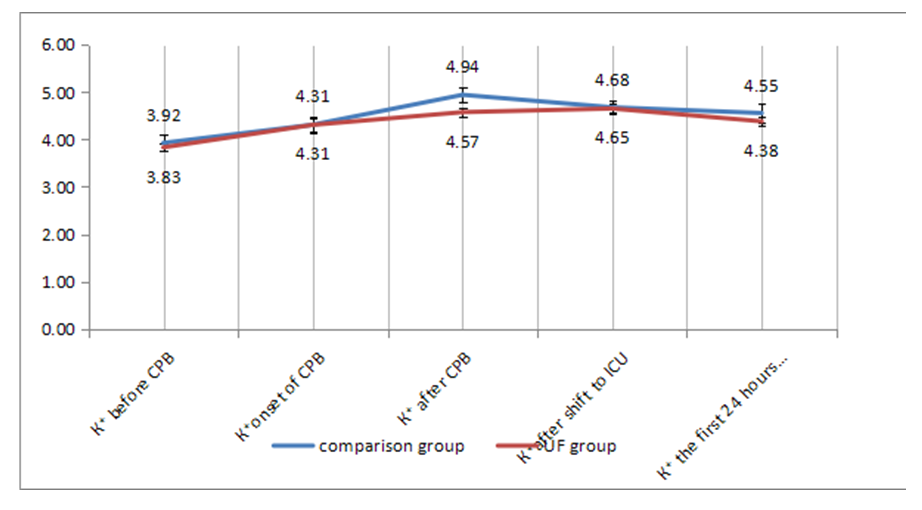 | Figure 2. Dynamics of potassium levels in the perioperative period |
4. Conclusions
- In our work, we examined the changes of the acid-base state in patients with SE during CPB. It was revealed that changes in the acid-base state in patients with SE entailed changes in the electrolyte balance of the blood due to the inclusion of the compensatory systems of the body.Balanced blood UF supports the compensatory mechanism of respiratory alkalosis in patients with SE during CPB. Balanced UF reduces hemodilution, maintains a normal level of albumin in the blood and reduces the level of potassium ions in the blood by eliminating them during filtration, which is a necessary property during hyperkalemic cardioplegia.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML