-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(9): 697-701
doi:10.5923/j.ajmms.20201009.14
Received: July 15, 2020; Accepted: August 20, 2020; Published: August 29, 2020

Clinical and Instrumental Diagnostics of Gallstone Ileus
F. A. Khadjibaev1, 2, F. B. Alidjanov2, A. B. Kurbonov1
1Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan
2Tashkent Institute of Post-Education Doctors, Tashkent, Uzbekistan
Correspondence to: F. A. Khadjibaev, Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction Gallstone ileus is a rare and at the same time serious complication of cholelithiasis. The reason of its development is the migration of gallstones from the bile ductslumen, most often from the gallbladder into the small intestine lumen. Its prevalence among older age groups exacerbates its course in connection with concomitant chronic and degenerative diseases, which increase the complexity of the treatment choice. It is quite difficult to diagnose gallstone ileus on the basis of only clinical symptoms. Therefore, it is necessary to use data from instrumental methods of research to establish an accurate diagnosis. In this article, we show the main features of gallstone intestinal obstruction and discuss the current state of the problem in modern literature. Aim of the study is to identify the main characteristic clinical features of gallstone ileus and the diagnostic capabilities of instrumental research methods. Material and methods 37 patients with gallstone ileus were treatment at the Republican Research Centre of Emergency Medicine from 2005 to 2019. 5 patients were with Bouveret’s syndrome, the remaining 32 had gallstone ileus. Results The age of patients ranged from 48 to 87 years (mean age 70.3 years). The ratio between females and males was 2.1: 1. More than 90% of patients had concomitant pathology. 72.9% of patients had a gallstone history with a duration of 3 to 33 years. In the anamnesis of 65.7% of patients there were no operations on abdominal organs. Most patients admitted with complaints of cramping abdominal pain, nausea, vomiting, the average duration of symptoms was 5 (1-15) days. The preoperative diagnosis of gallstone ileus was established in 45.9% of patients using a combination of diagnostic methods: ultrasound, radiography, Esophagogastroduodenoscopy (EGDS) and computer tomography (CT). Conclusion Our analysis showed that gallstone ileus, despite its rarity, has a number of specific signs to suspect this form of acute intestinal obstruction and to conduct studies aimed at confirming the diagnosis (EGDS, X-ray contrast examination of the gastrointestinal tract and CT, if necessary). Timely diagnostics will avoid a delay in the timing of the surgery and will positively affect the treatment results.
Keywords: Gallstone ileus, Bouveret’s syndrome, Biliodigestive fistula, Rigler's triad
Cite this paper: F. A. Khadjibaev, F. B. Alidjanov, A. B. Kurbonov, Clinical and Instrumental Diagnostics of Gallstone Ileus, American Journal of Medicine and Medical Sciences, Vol. 10 No. 9, 2020, pp. 697-701. doi: 10.5923/j.ajmms.20201009.14.
1. Introduction
- Gallstone ileus (GI), or the so-called biliary ileus, develops as a result of the passage of gallstone into the intestinal lumen through a biliodigestive fistula. This pathology refers to rare forms of acute intestinal obstruction (AIO) and is observed from 0.4% to 5% among patients with mechanical ileus [1] and occurs with a constant frequency of 30–35 cases out of 1,000,000 admissions over a 45-year period [2]. AIO has a high incidence of postoperative complications and mortality, reaching up to 50% and 27%, respectively [3]. A high frequency of complications and mortality is explained by such unmodifiable factors as old age, multiple concomitant diseases, in particular cardiovascular, respiratory and endocrine (diabetes and obesity), as well as late manifestation of symptoms (on average 4–8 days) [4-5] or delayed surgery associated with diagnosis, 2–37 days (range 1–15 days) [2,6-7]. One of the main reasons of the high postoperative complications frequency and mortality is a delayed surgery connected with diagnostics [4].Due to the rarity of this pathology, there is practically no analysis of the reliability of traditional methods of radiation diagnostics in the literature. It is known that stones in the intestinal lumen are difficult to visualize on plain radiography, while only 10–20% of stones contain enough calcium to be X-ray contrast [8-9]. However, some authors note the high reliability of CT and MRI in the diagnostics of GIO [5-6]. The vast majority of those stones which cannot be visualized are X-ray negative (usually associated with cholesterol stones), but some may be hidden by obesity or superimposed by bone structures or fluid-filled intestines [10]. At the same time, some authors note the high reliability of CT and MRI in the diagnostics of gallstone ileus [11-12]. Contrast-enhanced CT is considered the gold standard for diagnosing intra-abdominal abnormalities. Nevertheless, non-contrast CT has noticeable advantages: it does not cause a contrast allergic reaction, can be used to examine patients with renal insufficiency, and, importantly, non-contrast CT can identify ectopic gallstones regardless of the degree of calcification [8,13]. MRI scans can demonstrate almost 100% of cases of the Riegler triad [14] compared to 77.8% at CT. This research method is relevant for assessing the risk or tendency of chronic gallbladder calculus pass to fistula into the intestine [15]. However, in practice, the implementation of MRI and CT for all patients with AIO in order to diagnose this pathology is quite expensive and is available only for large clinics [16]. In this regard, to recommend their widespread use today is not possible. The way out of this situation may be the selection of patients with AIO for conducting high-precision methods of radiation diagnostics based on clinical and medical history data and data of generally accepted methods of radiation diagnostics (overview radiography of the abdominal cavity and ultrasound).Aim of the study is to identify the main characteristic clinical features of gallstone ileus and the diagnostic capabilities of instrumental research methods.
2. Material and Methods
- The analysis of the diagnostic results of 37 patients treated due to gallstone intestinal obstruction at the Republican Research Centre of Emergency Medicine in the period from 2005 to 2019 was carried out. The analysis included anamnestic data, the course and duration of the clinical picture, the results of radiation research methods (survey radiography of the abdominal cavity, ultrasound, contrast study of the gastrointestinal tract, CT), as well as esophagogastroduodenoscopy (EGDS).
3. Results
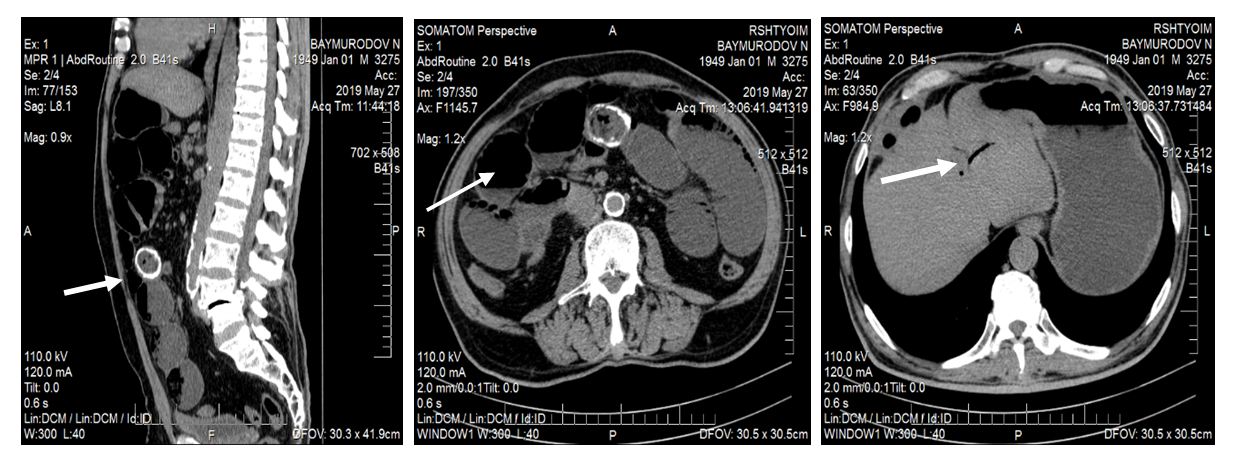
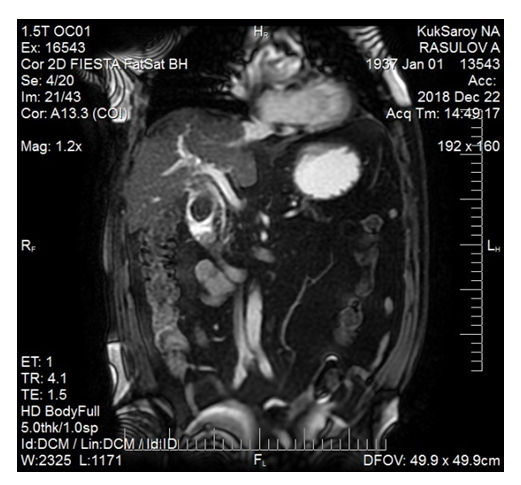
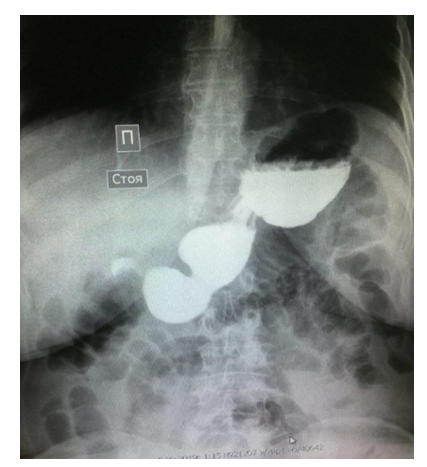
- 37 patients with gallstone ileus have been operated on at the Republican Research Center of Emergency Medicine for 15 years. Five of them were with Bouveret’s syndrome. Patients’ age varied from48 to 87 years. Mean age made up 70.3 years. The number of patients by age was as follows: up to 50 years - 1, from 51 to 60 years –6, over 60 years - 32 (86.5%). The ratio of women to men was 2.1: 1. More than 90% of patients had concomitant pathology, 23 of them had 2 or more concomitant diseases. 72.9% of patients had a gallstone anamnesis with a history from 3 to 33 years; 2 of them had been previously undergone retrograde pancreatocholangiography (RPCH), endoscopic papillosphincterotomy (EPST) due to choledocholithiasis. One patient was performed cholecystolithomy due to destructive cholecystitis 33 years ago. 25 (67.5%) patients were not performed surgerieson abdominal organs in the past. Patients were admitted to the hospital within 1 to 15 days from the onset of the disease first symptoms (on average after 5 days).The clinical presentation of patients with Bouveret’s syndrome and small bowel obstruction was different. The main characteristic symptoms in patients with Bouveret’s syndrome were nausea, repeated vomiting of food eaten. There was a presence of blood impurities in the vomit, as a result of pressure sores of the duodenal wall with a large fixed calculus in 2 (40%) patients. Usually abdominal pains were non-intense, bursting in the epigastric region. One patient had no abdominal pain at all. Typical complaints of patients with gallstone small bowel obstruction were diffuse cramping abdominal pain, nausea, repeated vomiting, bloating, flatulence and no stool. In 22 (68.7%) patients pain was intermittent, i.e. from time to time periods of symptoms relief for a more or less long time (from 4 to 24 hours) were noted with their subsequent resumption. Nausea and repeated vomiting were noted in all patients in this group. There were gallstones of various diameters left along with vomiting 2 patients. Gas and stool retention was observed in 22 (68.7%) patients. 27 (84.3%) patients had bloating of various degrees occurred at admission. Survey radiography of the abdominal cavity was performed in 34 (91.2%) patients: small bowel levels were found in 24, pneumobilia - in 11, no shadow from calculus outside the projection of the biliary tract was detected in any patient (Fig. 1). An X-ray contrast study of the stomach was performed in 13 patients; in 5 cases, reflux of the contrast agent into the bile ducts, which indicated cholecystoduodenal fistula, was noted (Fig. 2). In one patient with Bouveret’s syndrome a shade of calculus obturation of the duodenal bulb was revealed (Fig. 3).
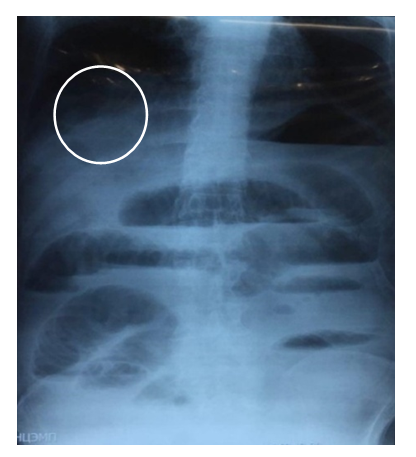 | Figure 1. Multiple small intestinal levels and pneumobilia are determined on a panoramic radiograph |
 | Figure 2. On an X-ray contrast study of the stomach, the reflux of the contrast agent into the gallbladder through a cholecysto-duodenal fistula is determined |
 | Figure 3. X-ray of the stomach. A filling defect at Bouvert’s syndrome is determined in the duodenal bulb |
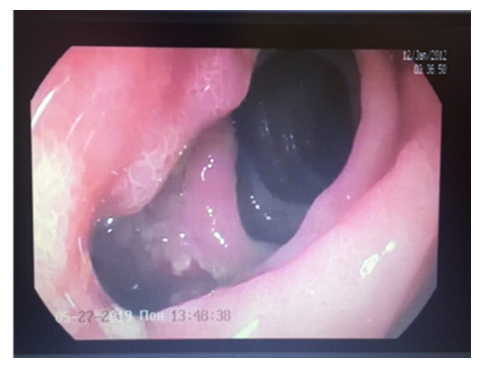 | Figure 4. Cholecystoduodenal fistula is determined on EGDS |
 | Figure 5. Obturation calculus is visualized in the duodenum |
4. Discussion
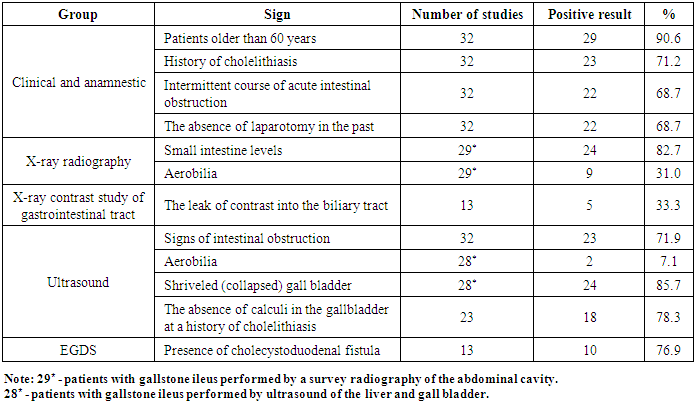
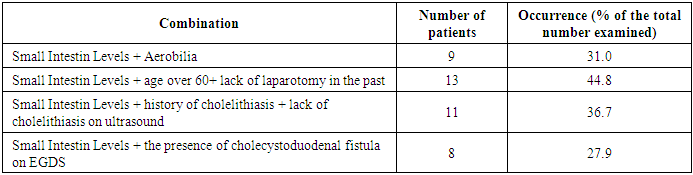
- The results of the study showed that the diagnostics of gallstone ileus (GI) in the form of Bouveret’s syndrome is not particularly difficult and can be easily determined by EGDS or X-ray examination of the gastrointestinal tract. However, it is quite difficult to establish a small intestinal GI in a timely manner. At the same time, CT and MRI are highly informative in the diagnosis of GI. However, the implementation of these research methods for all patients with acute intestinal obstruction is highly costly, and often impossible because of the lack of equipment in clinics. At the same time, as S. Reinberg aptly noted [8], “The diagnosis should be economical: only the diagnosis that gets the most information with a minimum of research is good. Therefore, it is necessary to narrow the indications for high-tech research without compromising diagnostics. Our studies showed the most sensitive signs of GI, which are presented in Table 1.
|
|
5. Conclusions
- The symptoms and signs of gallstone ileus are mostly nonspecific. The intermittent nature of the symptoms will interfere to establish a correct diagnosis when the clinical manifestations correspond to partial obstruction or distal migration of the gallstone. A high index of suspicion is required, especially in elderly patients with signs of small bowel obstruction. The use of radiological imaging is invaluable in the diagnostics of intestinal obstruction.Thus, we can conclude that in most cases it is possible to establish with high accuracy the diagnosis of gallstone ileus by a combination of the above signs, and the feasibility of CT and MRI to clarify gallstone ileus should be made in case of doubt and require further clarification.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML