-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(9): 682-689
doi:10.5923/j.ajmms.20201009.12
Received: July 27, 2020; Accepted: August 16, 2020; Published: August 26, 2020

A Survey on Implementation of Integrated Management of Childhood Illness (IMCI) in Northeastern Part of Bangladesh
Md. Shahariar Khan 1, Md Rahimullah Miah 2, Tania Hussain 1, Syed Moosa M. A. Quaium 1, Azizur Rahman 1
1Department of Paediatrics, Northeast Medical College & Hospital, Sylhet, Bangladesh
2Department of Information Technology in Health, Northeast Medical College & Hospital Pvt. Limited, Sylhet, Bangladesh
Correspondence to: Md. Shahariar Khan , Department of Paediatrics, Northeast Medical College & Hospital, Sylhet, Bangladesh.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

An explorative field study evaluates on implementation of integrated management of childhood illness (IMCI) at private medical college hospital and surrounding health care centres in the northeastern part of Bangladesh. The aim of the study is to follow the improvement of health care practices using IMCI strategy. The primary data were collected through questionnaire survey at field levels from medical college hospitals and adjacent healthcare centres, and secondary data were obtained from prominent sources. The study represents on the 60% of male and the rest of female child patients. Among them, 75% of viewers queried about danger signs and 50% of patients were assessed about their positive reflection on main clinical features, where the highest ranking in fever and the low in ear problems. A proposed model develops for IMCI implementation at all health institutions and community levels. The study recommends for dynamic policy development to implement IMCI strategy.
Keywords: IMCI, Healthcare, Service Providers, Common diseases, Bangladesh
Cite this paper: Md. Shahariar Khan , Md Rahimullah Miah , Tania Hussain , Syed Moosa M. A. Quaium , Azizur Rahman , A Survey on Implementation of Integrated Management of Childhood Illness (IMCI) in Northeastern Part of Bangladesh, American Journal of Medicine and Medical Sciences, Vol. 10 No. 9, 2020, pp. 682-689. doi: 10.5923/j.ajmms.20201009.12.
Article Outline
1. Introduction
- Many parents search health care for their ill children caring them to clinics, health centres, hospitals, physicians, traditional healers and other health care providers (Horwood et al., 2009). Earlier field survey exposed that actually a lot of ill children are not effectively assessed and cured by the above mentioned health providers, as well as those parents are poorly advised (Horwood et al., 2009; WHO, 2018). Moreover, lack of health providers’ scientific knowledge on IMCI failed to proper assessment, diagnosis of common major diseases and their ideal referral (Lin and Tavrow, 2000). Nearly 6.3 billion children under 5 years die in each year in the world (Mollah and Nahar, 2018; WHO, 2019). The root causes of deaths are due to acute respiratory infections (ARI), diarrhea, malnutrition and neonatal diseases (Bulla and Hitze, 1978). The common causes of neonatal deaths are about two-thirds of all infants due to preterm low birth weight, perinatal asphyxia, sepsis, congenital abnormalities and malformations in Bangladesh (Ullah et al., 2019); Mollah and Nahar, 2018). So Integrated Management of Childhood Illness (IMCI) is an integrated strategy to improve child health, which associates with a number of significant health problems ensuing in major causes of morbidity and mortality like pneumonia, diarrhoea, malnutrition, measles, malaria (Latif, 2011; Li et al., 2010). Children brought to health facilities are often found suffering from more than one morbid condition, making a single diagnosis impossible. The children require a combined therapy for successful treatment. IMCI efforts have been made to focus on the child as a whole, rather than on a single disease or condition fostering a holistic approach to child health and development. The aim of the study is to find out the newest innovations with interdisciplinary approaches to solve the core challenges of IMCI implementation at all levels of the health sector in order to proper assessment, diagnosis and quick referral to the tertiary level hospitals as well as trained-up of all healthcare providers.
2. Research Methods and Materials
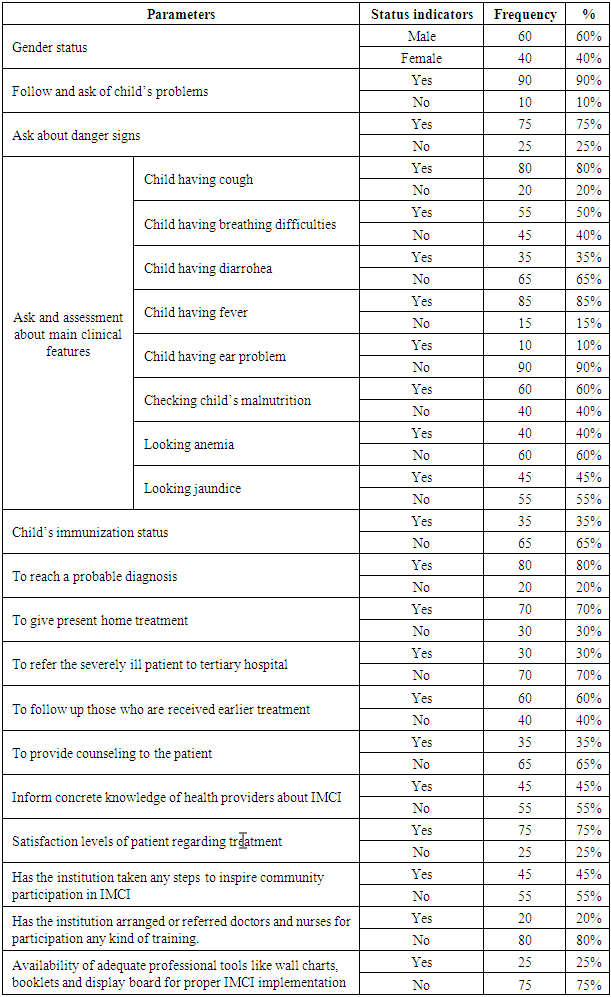
- This study was a field observational survey conducted in the department of Paediatrics at Northeast Medical College Hospital (NEMCH), Sylhet and surrounding health care centres in the northeastern part of Bangladesh from January 2020 to June 2020. Primary data were collected from the NEMCH and healthcare centres in Bangladesh pertaining to implement of Integrated Management of Childhood Illness (IMCI) deals with common diseases in children from the existing out patients of department and nearby health care centres. The surveyed data were also obtained through field observational survey among 100 patients. Secondary data were obtained from miscellaneous sources. Common diseases are ARI, diarrhoea, Malnutrition, Malaria, Measles, Otitis media and other diseases within the stipulated time.All general information regarding attained data was compiled according to the study aim. Compiled data were integrated for analysis and interpretation as findings using standard data analysis software like SPSS version 26, MS Excel 2019 and R programming version 3.5.
 | Figure 1. Site Map of Study Coverage Area in northeastern part of Bangladesh |
3. Results
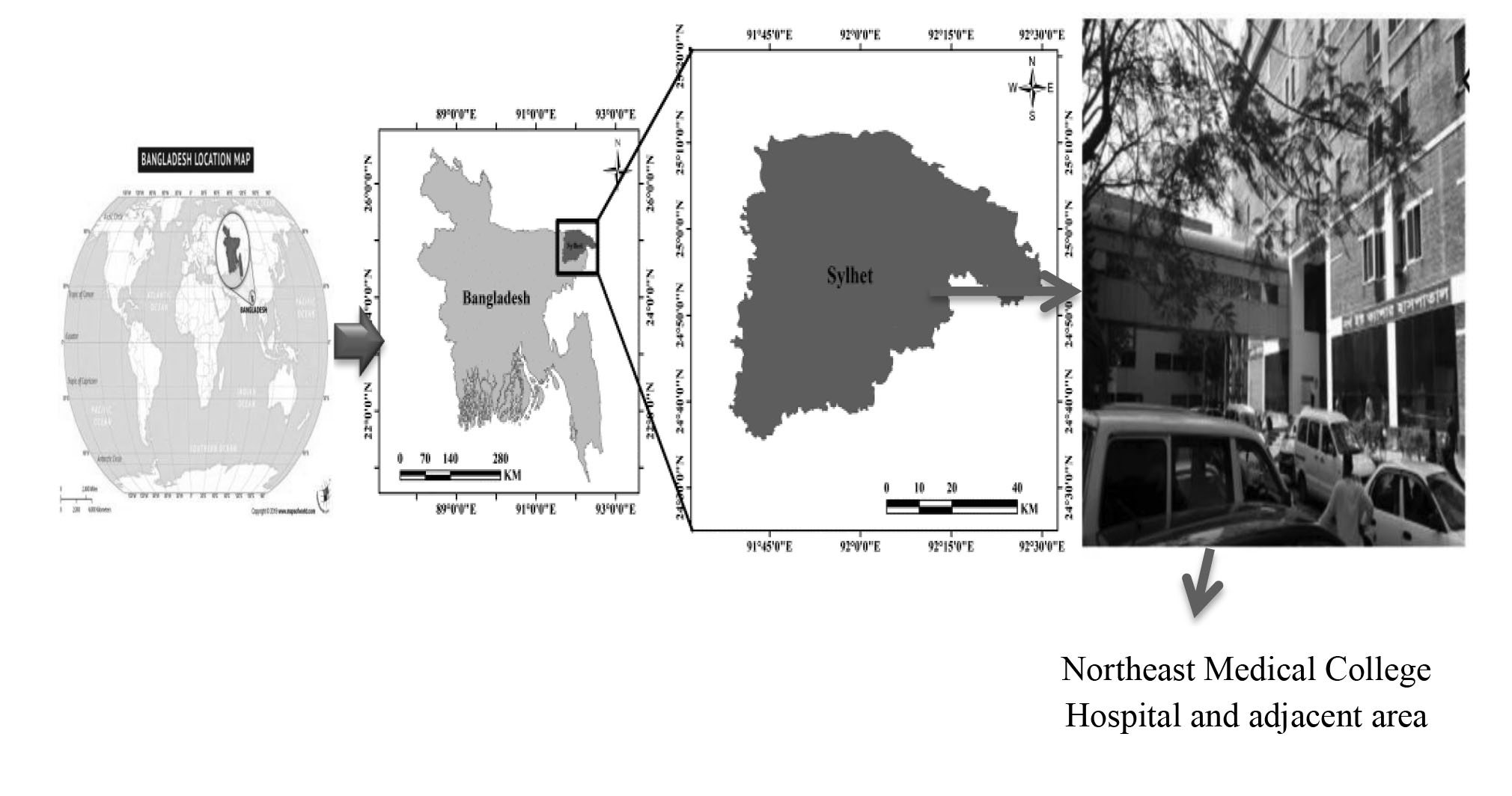
- From the source-profile of patients’ data illustrated on health awareness in common diseases, particular idea of ARI, diarrhea, malnutrition, sanitation, drinking water and service satisfaction and the patient’s status, which as shown in Table 1. The study enhances on diarrhea and malnutrition. From the study, about the 53% of patients were assessed about their positive reflection on main clinical features.
|
3.1. Total Patients Status
- From field observation, the clinical features with different patients identified the rate of prevalence, including maximum is fever and cough and minimum is ear problems, which as shown in Figure 2.
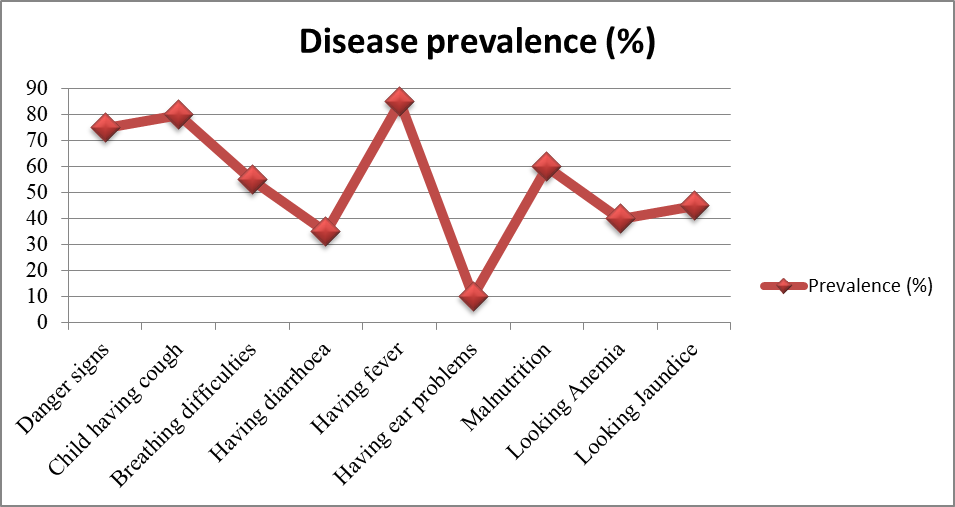 | Figure 2. Clinical features of different patients |
3.2. Referral Patients to Tertiary Hospital
- From field observation, the study illustrated in minimum patients are referred to tertiary level hospital, on the other hand, maximum patients are treated at home by the local health care providers, which as shown in Figure 3.
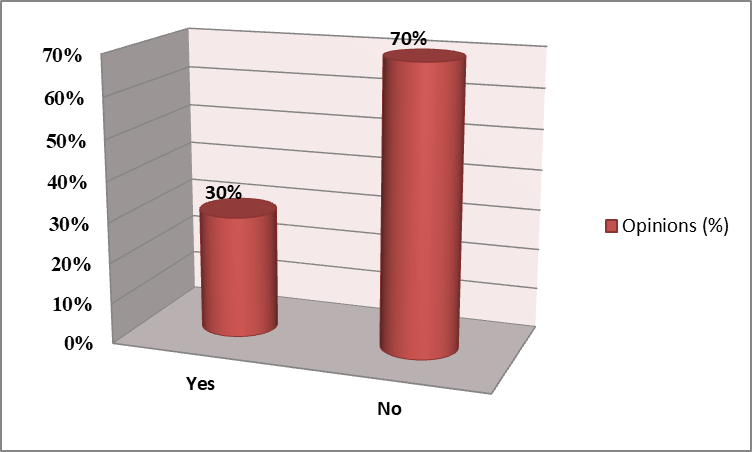 | Figure 3. Providing opinion on referral severely sick patients to tertiary hospital |
3.3. Concrete knowledge about IMCI
- From field observation, the study observed that the majority of health providers have no proper knowledge about IMCI implementation and management skills, which as shown in Figure 4.
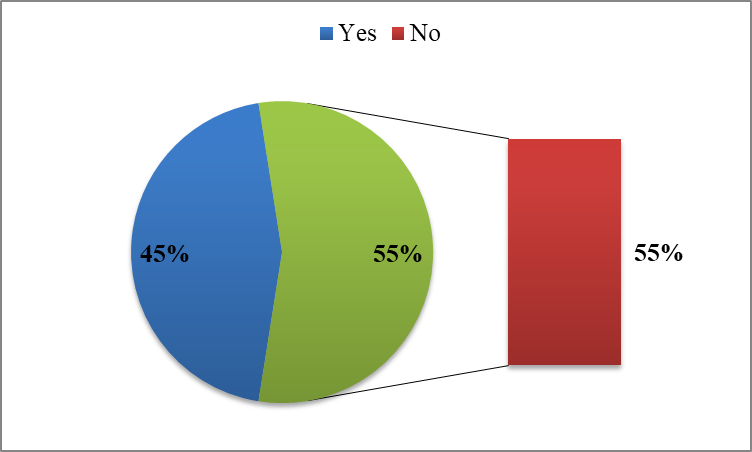 | Figure 4. Achieving concrete IMCI knowledge |
3.4. Priority of the IMCI Strategy Implementation
- Importance of the IMCI Strategy implementation, among all client issues at health care institutions and countries are mentioned with different ranks of priority. These are low priority, moderate priority, high priority and very high priority. From the field observation, about 60% of respondents were opined the positive response for the importance of the IMCI Strategy implementation among clients’ issues, meanwhile 34% of them negatively provided their opinions, which as shown in Figure 5.
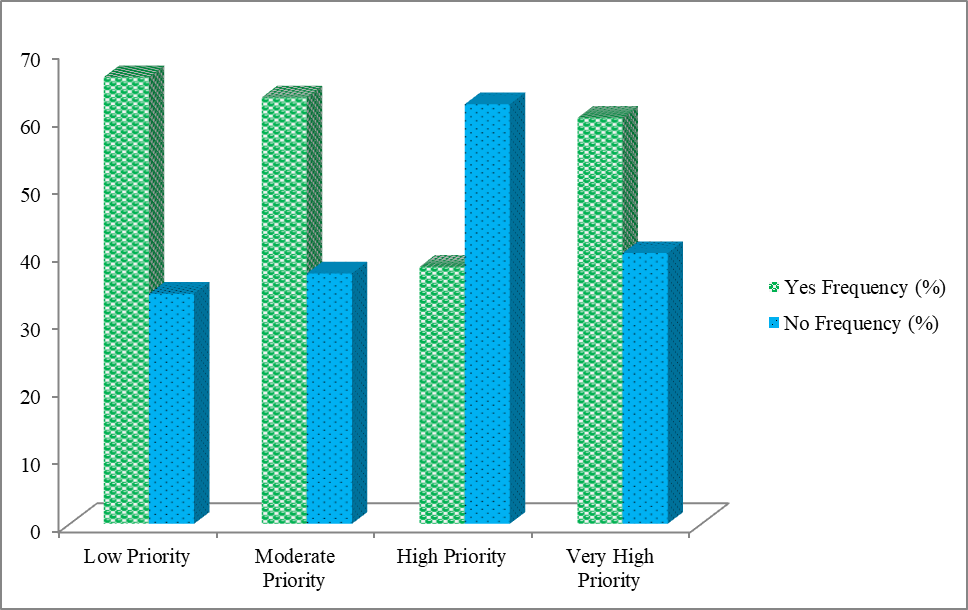 | Figure 5. Diverse Ranking of Priority of the IMCI Strategy Implementation among clients’ issues |
4. Discussion
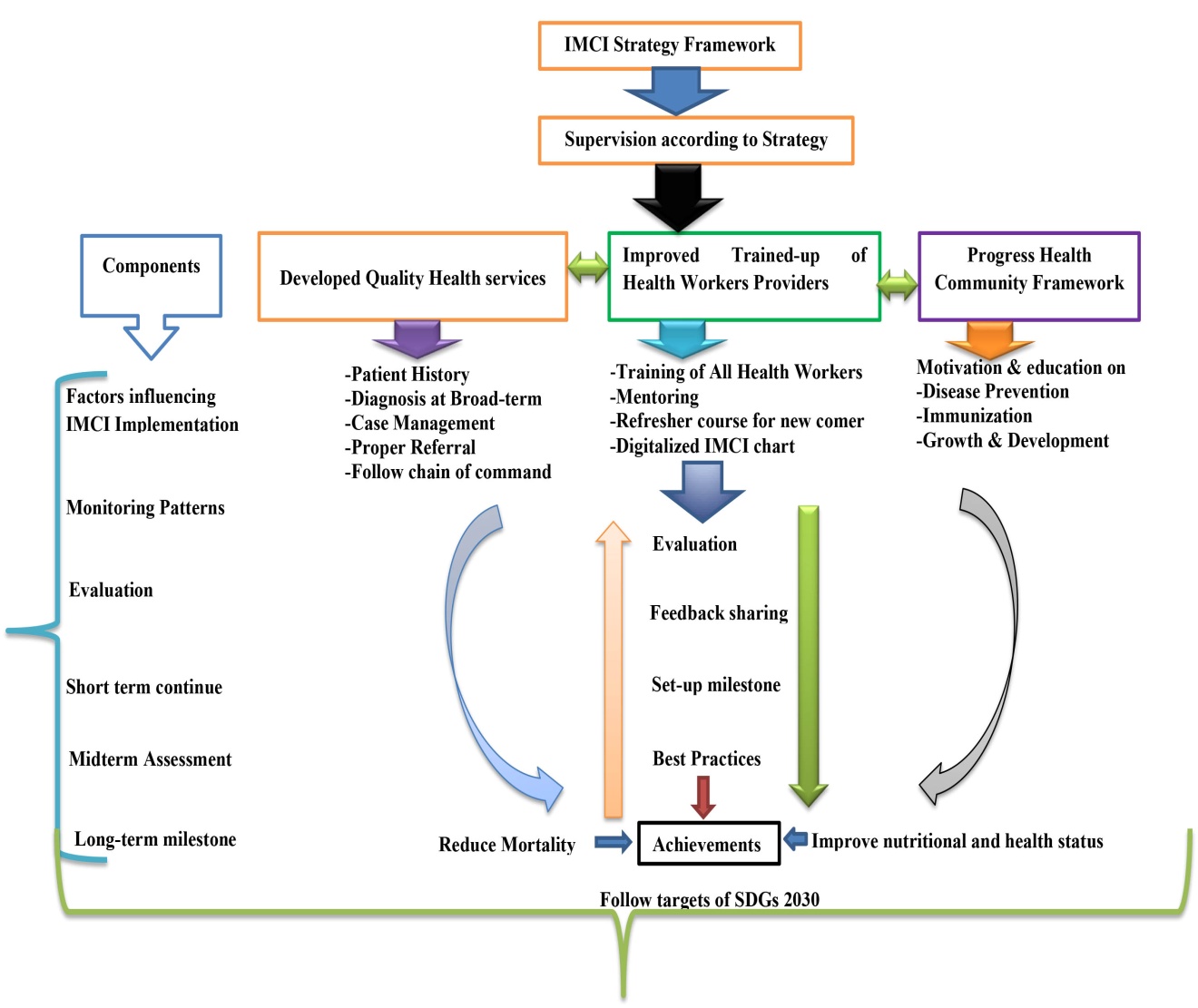
- The study illustrated on the Implementation of Integrated Management of Childhood Illness (IMCI), which was started by the World Health Organization and the United Nations International Children’s Fund 28 years ago for child health improvement. At present, the IMCI strategy is on-going in worldwide including Bangladesh. A survey in the Northeaster part of Bangladesh included at Northeast Medical College Hospital and nearby health centres indicating observational survey on Implementation profile of IMCI, Clinical features of different patients, referral patients to tertiary hospital, concrete knowledge about IMCI and the priority of the IMCI strategy implementation. The findings illustrate on the IMCI profile data regarding about 53% of the patients were assessed in their positive reflection on main clinical features at health institute and centres. The outcomes also exposed to different clinical features including cough, breathing difficulties, diarrhoea, fever, ear problems, malnutrition, anemia and jaundice. Out of them, the highest sign symptom prevalence is fever and the lowest is ear problems. The research exposed the attitude for the referral system to the tertiary hospital due to less practices on about 70% of clients opined their opinions negatively. More than 50% of health workers have no training knowledge on IMCI and also those who are knowledgeable, but they do not utilize it properly due to neglegence. On the other hand, most of health workers did not think integrately to diagnose in different diseases due to lack following the IMCI protocol. So, due to diagnose as a single disease, many other associated diseases are missing in time. For this reason, they need to integrate priority on the clients issue according to case management, including health care, diagnosis at broad term, nutritional assessment, immunization, instruction to the caregivers, and referral system according to presence of danger signs. Overall, most of child dealths occur due to single or combination of common diseases like acute respiratory infection, diarrhoea, malnutrition, malaria and measles (NICEF, 2011). IMCI has comprehended remarkable outcomes, both in reducing childhood mortality and in improving the quality of life children in the study area in Bangladesh. IMCI has achieved impressive results both in reducing childhood mortality and in improving the quality of life of children in Bangladesh. From the study it is identified that many health care providers do not follow the IMCI guidelines due to lack of knowledge & proper monitoring by supervisor, training and usual practices (Shazzadur Rahman et al., 2019). So for the time being, it enhances to develop further policy for the improvement of IMCI implementation properly. The IMCI strategy comprises both preventive and curative interventions (WHO, 2011). The framework of this strategy enhances to improve health care practices in health facilities, health systems, case management skills of health care providers, which are shown as Figure 6. If the higher authority can take the earlier preventive measure, then the mortality and morbidity can be reduced significantly (Dock et al., 2017). The study also observed the fast breathing and cough-cold are usual common manifestations of ARI in connection with another health difficulties which are very much significant due to great mortality and illness. (Hoang et al., 2019). Sometimes it may remain asymptomatic or silent (Son et al., 2017).
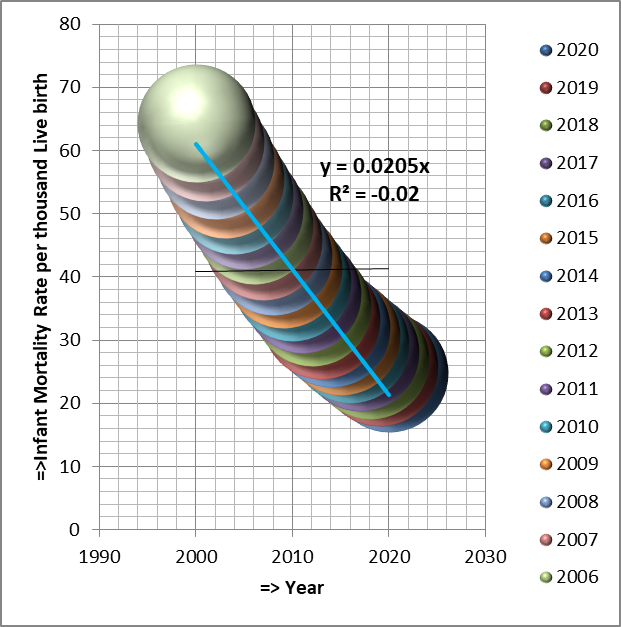 | Figure 6. Infant Mortality Rate per thousand Live birth (Statista, 2020) |
 | Figure 7. A Scientific Control Model for Recovery of Common Diseases |
5. Adversity of the Study
- Due to system complicated, obsolete, traditional and time consuming are diverse challenges in research on IMCI implementation. However, the providers are not fit comfortably during assessment and treatment. There are limited supervision, communication and evaluation data on IMCI implementation with less technological supports. The Sustainable Development Goals adopted by the United Nations in 2015 were developed to promote healthy lives and well-being for all children to reduce under-five mortality to at least as low as 25 per 1,000 live births in every country (WHO, 2019). On the other hand, Constitution of WHO (1948) stated that the achievement of any State in the promotion and protection of health is of value to all. Bangladesh, as a signatory member country, it is difficult to fulfill the health security with the targets of Sustainable Development Goals 2030 due to the high density of population and undesirable status quo.
6. Conclusions
- In concluding the IMCI is an integrated approach to improve child health including management of sick child, nutrition, immunization, other disease prevention and, promotion of growth and development The study also observed about the 53 % of patients were assessed about their positive reflection on main clinical features regarding IMCI implementation. The health care providers should overcome the barriers to implement IMCI. If the higher authority can take earlier preventive measures to provide high quality, training, safe health care with appropriate policies, equipment, facilities and personnel then the mortality and morbidity can be reduced significantly linking with Sustainable Development Goals 2030. The study recommends for future research trajectory with a methodological agenda on sustainable IMCI implementation.
7. Disclosure
- Data AvailabilityThe data are being used to support the findings of this research work are available from the corresponding author upon request. Competing InterestsThe authors declare no potential conflict of interests in this research work.
ACKNOWLEDGEMENTS
- The authors acknowledged the authority of NEMCH, Sylhet, Bangladesh for kind support.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML