-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(8): 624-626
doi:10.5923/j.ajmms.20201008.18
Received: July 13, 2020; Accepted: July 29, 2020; Published: August 15, 2020

Efficiency of Heprocel in Treatment of Patients with Deep Burns
O. T. Yunusov , F. A. Daminov , Kh. K. Karabaev
Department of General Surgery, Samarkand State Medical Institute, Samarkand, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The work is based on an analysis of the treatment results of 105 victims with thermal injuries (37 females and 68 males) aged from 18 to 75 years who were treated in the combustiology department of the Samarkand branch of the Republican Research Centre of Emergency Medicine in 2017-2019. Clinical evaluation included the following criteria: quantity and nature of discharge; bleeding wounds; terms of epithelization of donor sites, transplanted autodermografts; completeness of epithelization; the severity of wound pain. Local single application of the hemostatic drug Geprocel to the wound with autodermoplasty promotes rapid adhesion of the graft, provides quick and complete engraftment of skin flaps. Improving the results of early necrectomy with autodermoplasty in burned patients by using the local hemostatic agent Heprocel will allow earlier discharge from the hospital and return to the daily life of patients.
Keywords: Heprocel, Burn disease, Necrectomy, Hemostatic agents, Autodermoplasty, Disseminated intravascular syndrome
Cite this paper: O. T. Yunusov , F. A. Daminov , Kh. K. Karabaev , Efficiency of Heprocel in Treatment of Patients with Deep Burns, American Journal of Medicine and Medical Sciences, Vol. 10 No. 8, 2020, pp. 624-626. doi: 10.5923/j.ajmms.20201008.18.
1. Introduction
- Thermal lesions present a serious medical, social, and economic problem. The development of heavy industry and the chemical industry, as well as the widespread use of electric energy in everyday life and industry, contribute to a significant increase of burn injuries. Literature data indicate a stable number of thermal injury victims, the proportion of which makes up 5-12% among peacetime injuries. Burns take 2-3 places in the general structure of injuries with a high proportion of deep burn injuries requiring mandatory surgical treatment [1-2].The essence of deep burns surgical treatment is to piece out the skin defects formed as a result of their necrosis. The most common method of restoring the integrity of the skin is free skin plastic. Plastic closure of a burn wound is preceded by its preparation, which consists in cleansing the wound from necrotic tissues and forming a bed favorable for graft engraftment. Preparation of burn wounds for autodermoplasty can be carried out at different times, by various methods, differing by more or less "aggressiveness". In all cases, the final stage is the closure of the wound surface [3-5].There are two main directions of surgical treatment of burned patients: 1) autodermoplasty of granulating post-burn wounds after spontaneous rejection of necrotic tissue or chemical necrectomy; 2) early surgical necrectomy before the development of inflammation in the wound with subsequent autodermoplasty [6]. Self-rejection of dead tissue during deep burns leads to a complete cleansing of the wound surface after 4-6 weeks. The long existence of a burn scab prevents the implementation of autodermoplasty, promotes the development of pyogenic microflora in the burn wound and the release of toxic substances [7-8].Thanks to early surgical treatment (removal of a burn scab in the first 3-7 days after an injury with simultaneous or delayed autodermoplasty), there are opportunities for changing the course of a burn disease and interrupting its course [9]. The time for preparing burn wounds for autodermoplasty, the time to restore the integrity of the skin, the duration of inpatient treatment, the number of infectious complications and deaths are reduced [10-11]. Early surgical necrectomy is a rather traumatic operation and may be accompanied by profuse blood loss. Blood loss is at least 250-300 ml from the wound surface in 10% [2]. According to other sources, with early excision of dead tissue in an area of 100 cm2, 76 ml of blood is lost, and removal of granulations in the same area is 64 ml [9,12-13].It should be also borne in mind that autodermoplasty provides the formation of extensive "donor" wound surfaces, often equal to burns area. Taking into account the operational risk associated with blood loss and pain impulse, an increase in the area of lost skin, this type of surgery occupies a special place [14-16]. Therefore, adequately performed local hemostatic therapy during surgery can prevent blood loss, thereby improving treatment outcomes for this type of patients [17-18]. Aim of the study is to improve the results of early necrectomy with autodermoplasty in burnt patients by using the local hemostatic agent Geprocel.
2. Material and Methods
- The work is based on an analysis of the treatment results of 105 victims with thermal injuries (37 females and 68 males) aged from 18 to 75 years who were treated in the combustiology Department of the Samarkand branch of the Republican Research Centre of Emergency Medicine from 2017 to 2019. Mean age age of the patients made up 39 years. In most cases, the cause of the injury was a flame; burns with boiling water and contact burns were also observed. The total lesion area in patients ranged from 10 to 40% of the body surface, and a deep burn of IIIb-IV degree - up to 10%. All patients underwent early necrectomy up to healthy tissues with the appearance of capillary bleeding with simultaneous autodermoplasty. Hemostasis was carried out with hemostatic powder from cellulose derivatives with the Geprocel. Application of the drug made up10 mg of powder 1 time per day for 3 days on the wound defect surface. The clinical assessment included the following criteria: the amount and nature of the separated substance; bleeding of wounds; timing of epithelialization of donor sites, transplanted autodermotransplants; completeness of epithelialization; severity of wound pain. Surgical interventions for 105 patients with deep burns were performed using the hemostatic drug Geprocel to stop bleeding after excision of necrotic skin and subcutaneous structures.
3. Results
- Our studies showed that early surgical necrectomy and the taking of split autografts from donor sites was accompanied by blood loss (6-10 ml of blood in an area of 100 cm2). After applying the Heprocel hemostatic powder, the bleeding completely stopped, and the wound surface assumed a brilliant appearance due to the film adhered to it. Pain senses were insignificant. When a wound defect was closed with a donor autoslap, good adhesion of the skin flap to the underlying wound was noted.At the examination next day, signs of necrosis of the skin graft were not observed. The donor wound was also clean, signs of infection and pain were not distinguished. On the 3rd day after the surgery, the patients had a positive dynamics of the skin graft healing, the detection of discharge from the wound was not observed. There were no signs of inflammation or infection in the donor site. On the 7th day after skin transplantation almost complete engraftment of the skin graft was noted, the suture line appeared in the form of a clear thin line, with no signs of redness or infiltration. The skin graft was soft, supple, pale pink. There was no evidence of infection. The donor site was completely epithelized; a thin elastic scar remained without signs of hypertrophy.Complete engraftment of the skin autograft with complete restoration of the defect with slight contraction of the defect area occurred on the 12th day. Thus, the use of the film form of Heprocel hemostatic after necrectomy followed by autodermoplasty in all cases promoted the complete healing of donor sites in patients on the 7th day, and complete engraftment of the skin autograft with complete restoration of the defect by 12th day after surgery.Figures 1, 2 show pictures of a patient F. 42g. admitted with II-IIIAB degree burns of the neck, face, both shoulders and arms (the total surface was 60%). The patient was performed necrectomy 8-9 days after the burn.
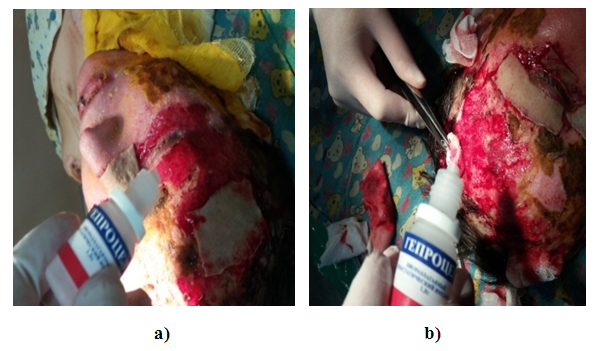 | Figure 1. Patient F., 42 years. a) necrectomy; b) application of Heprocel |
 | Figure 2. Autodermoplasty for patient F., 42 years |
4. Conclusions
- The use of the drug Geprocel during autodermoplasty after early necrectomy provides complete hemostasis and a decrease in the severity of wound pain.Local single application of the hemostatic drug Geprocel to the wound after necrectomy with autodermoplasty promotes rapid adhesion of the graft, provides quick and complete engraftment of skin flaps.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML