Alimova H. P. , Alibekova M. B. , Azimova S. N. , Rakhimova S. R.
Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Multiple organ failure syndrome is determined by the presence of dysfunction of two or more systems of an organism. A total of 60 children aged 3 months to 4 years with diagnosed multiple organ failure were under observation in the intensive care unit and in the paediatric department of the RRCEM. The reason for the development of multiple organ failure syndrome are inflammatory diseases of the lung - 41 (68,3%), combined and associated injuries – 7 (11,7%), sepsis - 12 (20%). In children with polyorgan failure, CD3+, CD4+ and CD16+- lymphocyte count were reduced, CD25+, CD38+ and CD95+- lymphocytes were elevated, B-lymphocyte counts were elevated, and IgA, IgG and IgM immunoglobulin counts were below normal. Level of IL-1 in patients was significantly elevated (p<0,001). For all 60 children with multiple organ failure after the examination were provided immunocorrection with the immunological medication Octagm 30-50 mg/kg 2 times, once a week. Inclusion of Octagam in the complex therapy of children with multiple organ failure led to the increase of initially decreased indexes of the immune cellular link, stabilizated of humoral immunity, shortening the terms of antibacterial therapy, shortening the terms of hospitalization.
Keywords:
Multiple organ failure syndrome, Clinic, Immunogram, Children
Cite this paper: Alimova H. P. , Alibekova M. B. , Azimova S. N. , Rakhimova S. R. , Immunotherapy for Multiple Organ Failure in Children, American Journal of Medicine and Medical Sciences, Vol. 10 No. 8, 2020, pp. 620-623. doi: 10.5923/j.ajmms.20201008.17.
1. Introduction
In recent years, the number of children with multiple organ failure of various etiologies has increased. The high predisposition for the development of multiple organ failure syndrome (MOFS) in children compared with adults is explained by the imbalance in children of the mechanisms regulating the inflammatory response, the vulnerability of the homeostasis system and metabolic reactions, the immaturity of the immune and endocrine systems, which predispose them to contracting the infection and which further contributes to the progression of MOFS [1-2].In recent years, the problem of the immunology of critical states has acquired a pronounced pragmatic character. It has become evident that the determination of the meaning of immunological shifts, their correct and timely diagnosis и and directed correction are an integral part of the management of patients in intensive care units, but unfortunately, very little has been done in this area of scientific research [3-4].Since the discovery of interleukins in the 1970s, more than one hundred biologically active substances have been detected to date. Interleukins enter the bloodstream only for a short time, but it turns out to be enough to launch IL-6 products. IL-6 is constantly present in blood, so its concentration is more consistent with the severity of the inflammatory process [5-6].A special place in the integrated treatment of bacterial infections is the effects directed at the immune system - immunomodulation. When considering the scope of integrated therapy, it is important to take into account the pathogenic mechanisms of their development and the impact of medicines on the immune system of a sick child [7-8]. In general, at present, the search and study of the effectiveness of multiple organ failure agents that inhibit apoptosis and modulate the immune response are ongoing.Aim of research was to study the immunological features and effectiveness of immunotherapy for multiple organ failure in children.
2. Material and Methods
A total of 60 children aged 3 months to 4 years with diagnosed polyorganic insufficiency were under observation in the anesthesiology and intensive care unit (AICU) and in the paediatric department of the RRCEM. Multiple organ failure syndrome in children was defined as the presence of dysfunction of two or more body systems. Among the children examined, 35 (58,5%) were boys and 25 (41,5%) were girls. The average age of the children examined was 1.7. All patients were carried out general clinical examination, biochemical blood tests (total protein, urea, creatinine, bilirubin, potassium, ALT, AST, lactate level, medium-molecular peptides), acid-alkaline state of blood, instrumental methods of examination (chest X-ray, ECG, according to the indications of echocardiography, CT-research). In addition, all patients were conducted immunological tests.The main indicators of the immune system were studied during the acute period of the disease and after immunocorrection (period of clinical well-being). The level of CD3, CD4, CD8, CD16, CD20, CD25, CD38, CD95 lymphocytes were evaluated using monoclonal antibodies (Sorbent Ltd., Moscow). The amount of serum immunoglobulins of classes Ig A, Ig M, Ig G (g / l) was determined by the method of radial immunodiffusion according to Mancini (1969).The level of cytokine (IL-1β, 6) in blood serum was determined by solidphase immunoenzyme analysis using test systems of Vector-Best LLP (Novosibirsk). The data obtained were statistically processed using the Statistica 6.0 software. All 60 children with multiple organ failure after examination provided immunocorrection by immunological drug Octagam, solution for infusions transparent, 20 ml 1g, 30-50 mg/kg 2 times, once a week (production of OCTAPHARMA Pharmazeutika Produktionsges, m.b.H (Austria) OCTAPHARMA NORDIK AB (Sweden)).OCTAGAM is a solution for infusions transparent or slightly opalescent, from colourless to light yellow, 1 ml plasma protein 50 mg, including at least 95% IgG. The form of release 20 ml bottle contains 1g of active substance - normal human immunoglobulin, for children were prescribed 30-50 mg / kg once a day, a week later.
3. Results and Discussion
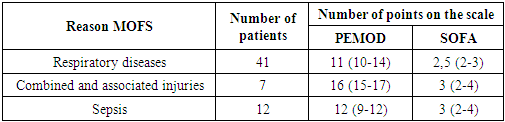
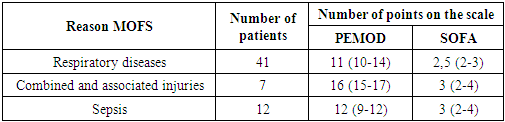
The main systems of organs involved in the pathological process were respiratory, cardiovascular and central nervous systems. Acute respiratory insufficiency in combination with acute heart failure of the 2nd degree were observed in 36 (60%) children, respiratory and cardiovascular insufficiency in combination with cerebral insufficiency in 20 (33.3%) children, cardiovascular insufficiency in combination with toxic lesions of the liver, kidneys and intestinal insufficiency syndrome in 4 (6,7%) cases.The reason for the development of multiple organ failure syndrome was inflammatory diseases in the lungs - 41 (68,3%), combined and associated injuries - 7 (11,7%), sepsis – 12 (20%). Often cases of multiple organ syndrome development were noted against the background of congenital heart defects - 9 (15%). The severity of the children's condition was assessed with the Pediatric Multiple Organ Dysfunction Score (PEMOD). The system evaluates 6 key organ systems: Each of them has one clinical or laboratory criterion. The severity of the condition was also assessed using the scale Sequential Organ Failure Assessment (SOFA), which is designed to assess and describe the sequence of complications in critical patients. The SOFA scale is based on the evaluation of six organ systems: respiratory, cardiovascular, liver, coagulation, renal and neurological, from mild dysfunction (0 points) to severe failure (4 points) (Tab.1).Table 1. Evaluation of patient severity on prognostic scales
 |
| |
|
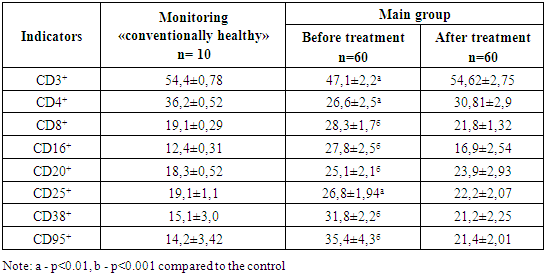
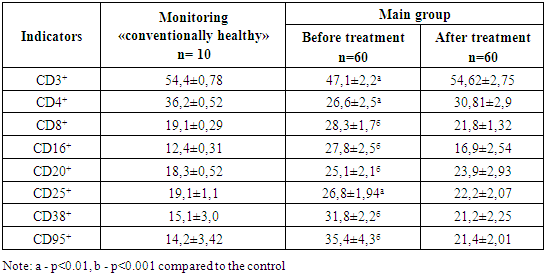
The clinically most severe on all prognostic scales used in the study were patients with combined and associated trauma who underwent emergency surgical interventions.Acute respiratory failure (ARF) of II degree was diagnosed in 40 (67%) of children. In blood tests (determination of the value of the acid-alkaline state an increase in pCO2 > 50 mmHg and a decrease in blood pH < 7.35 were noted.Acute respiratory failure (ARF) of III degree was diagnosed in 20 (33%) of children. These children, upon admission to the hospital, were transferred for forced ventilation by SAVINA (Germany), VELLA (USA). The criteria of indications for transfer to ALV were progressive respiratory insufficiency, pathological type of breathing, persistent tachycardia, indices of oxygen saturation in blood less than 90% despite oxygen therapy, рСО2>70 mmHg and blood pH <7,30.On 2-3 days, 5 (25%) children from 40 children with respiratory failure of the II degree due to insufficient effectiveness of conservative therapy and an increase of respiratory failure were provided with respiratory support in SIMV mode with subsequent transition to CPAP mode and after restoration of adequate sputaneous breathing, patients were extubated.Considering that lactate level disorder in the blood is assessed as a marker of tissue hypoxia, we analyzed the lactate content in the blood. In 47 (78,3%) children in biochemical blood tests lactate level was equal to 6,8±0,5 ммоль\л (normal 0,2-2,2 mmol/l), in 13 (21,7%) patients with severe cerebral insufficiency lactate level in blood was equal to 10,1±0,4 mmol/l. In children with cardiovascular insufficiency on the ECG, various types of metabolic-dystrophic disorders in the myocardium were noted. In 45 (75%) sick children, there were signs of impaired repolarization (decreased T wave and lengthening of the Q-T interval), and 15 (25%) children showed signs of myocardial hypoxia (high pointed T wave, with a normal interval (Q-T).In 13 (21.7%) of the child were observed damage to the central nervous system, clinically marked anxiety, agitation, seizures, stiff neck.In 5 (8.3%) children with lesions of the nervous system there were observed meningial (stiff neck, in early childhood – swelling large fontanelle, symptoms of Kernig, Brudzinsky) and cerebral disorders. Consciousness disorders up to a coma level (from stunning to deep sopor) were detected in 3 (5%), clonic-tonic seizures were noted in 2 (3.3%) children.Oculomotor disorders (strabismus) were observed in 2 (3.3%) children, swallowing disorders were observed in 1 (1.6%) children. At the spinal puncture in 3 (5%) patients the pressure of cerebrospinal fluid was increased, in the liquor a small cytosis, a small increase in protein content. In 6 (10%) patients the blood lactate level in blood tests was 8.4±0.4 mmol/l. In 2 (3,3%) children with hepatic insufficiency on the ultrasound examination of the liver there was a consolidation of the liver parenchyma and an increase in the size. In biochemical blood tests, an increase in the level of total serum bilirubin to 68.4 + 1.5 μmol / L, direct fraction over 10%, also ALT excess in 2 times. In 2 (3.3%), renal failure was prerenal. It was manifested by reduced diuresis. In biochemical blood tests - creatinine level exceeded the normal rate and reached 2.74±1.9 mmol/l, urea 9.9±6.1 mmol/l. The intestinal insufficiency syndrome is clinically manifested by stagnation in the stomach, a violation of digestion and absorption, intestinal paresis. A decrease in potassium level to 3.1 ± 0.2 mmol / L was noted in the blood. In the study of immunophenotype of blood lymphocytes in patients with MOF, immunodeficiency from the immune cellular link was revealed: a significant decrease (p<0,01) of relative number of T-lymphocytes in comparison with the control (47,1±2,2% against 54,4±0,78%), also a significant decrease of relative T-helper content in comparison with the control (26,6±2,5%, p<0,01 against 36,2±0,52%) was observed. During the analysis of non-specific resistance indices it was revealed that the relative content of EC-cells (CD16+) in the blood flow reliably exceeded the control value (27,8±2,5 and 12,4±0,31%, respectively) (p<0,001).The study of the status of activation markers revealed the number of CD25 + lymphocytes (26.8 1.94%) that are reliably above the control values (p 0.01). The relative values of CD38+ lymphocytes and CD95+ cells were also significantly higher than the control values (p<0,001).Table 2. Indicators of cellular immunity link in patients of the main group, %
 |
| |
|
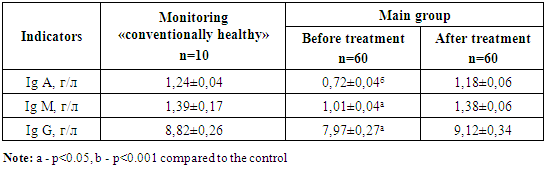
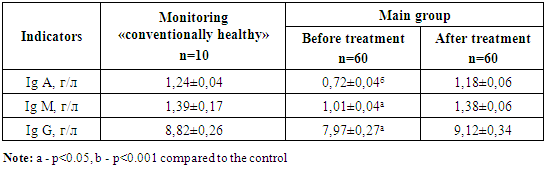
The content of IgG in patients' serum averaged 7.97±0.27 g/l, which is 1.1 times lower than control (8.82±0.26 g/l) (p<0.05). IgA and IgM levels in patients were also lower than in the control group (p<0,001 and p<0,05) (Table 3).Table 3. Indicators of the humoral immunity link in sick children with MOF
 |
| |
|
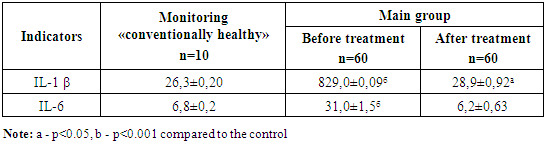
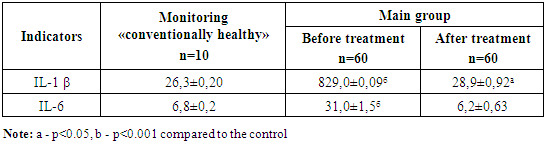
We conducted a study on the serum levels of IL-1 β and IL-6. Interleukin-6 (IL-6) belongs to the group of cytokines with anti-inflammatory and anti-inflammatory effects, also serves as an early marker for the determination of multiple organ failure. The level of IL-1 in patients before treatment was 31,9 times higher than in children of the control group (p<0,001) and on the average made 829±0,9 pg/ml. The production of IL-6 in children was higher (31±1.51 pg/ml), than in the control group (6.8±0.2 pg/ml) in 4.6 times (Table 4). Table 4. The content of cytokines in blood serum in children, PG / ml
 |
| |
|
Thus, in patients with multiple organ failure, a change in the quantitative indicators of the immune status was revealed: a decrease in the relative number of T-lymphocytes, T-helpers, an increase in the content of cytotoxic T-lymphocytes. In parallel with changes in T-cellular link of immunity in patients there were also changes in humoral link of immune status, which manifested as an increase in the number of B-lymphocytes and decrease in the level of immunoglobulins. In children with MOF, there was a significant increase in the production of pro-inflammatory cytokines IL-1 in IL-6 by 31.9 and 4.6 times respectively. All patients underwent complex etiopathogenetic therapy aimed at elimination of multiple organ failure manifestations, provision of adequate gas exchange, stabilization of central and peripheral hemodynamics and maintenance of adequate cerebral perfusion. Antibiotic therapy was carried out by the introduction of at least two broad-spectrum antibiotics (3rd generation cephalosporins + aminoglycosides), further on the sensitivity of the infection to antibiotics. Symptomatic therapy includes infusion and detoxification, medications that improve the rheological properties of blood (direct and indirect anticoagulants), sedatives.Sedative therapy was performed with: Sodium oxybutyrate 50-100mg/kg or 25-30mg/kg/hour, Dormicum 0.1-0.2mg/kg/hour, relaxants (Arduan 0.02-0.05mg/kg/hour) - against the background of forced-assisted lung ventilation. With improvement and stabilization of hemodynamics parameters, reduction of systemic inflammatory reaction, improvement of blood pH -7,35-7,40 and pSO2 ≤50 mmHg, under the control of oxygen saturation index (O2>90% at FiO2 ≤ 0,3) reduced the volume of intensive medication therapy. In heart failure, cardiac glycosides (Digoxin 0.025-0.05 mg / kg / day.), Cardiotropic (Dopamine 5-6 μg / kg / min.), Protease inhibitors (Contracal 500 IU / kg), glucocorticoid drugs (Prednisone 1) are prescribed) -3 mg / kg / day.). According to indications, antiarrhythmic drugs (lidocaine 0.5-1.0 mg / kg / hour.).The efficacy of treatment was manifested by normalization of hemodynamic parameters as the normal body temperature returned to normal, intoxication decreased, normalizated of lung gas exchange (O2>90% at FiO2 ≤ 0.3) and restorated of tissue respiration (blood lactate level decreased to 2.3 ± 1.5 mmol / h) and normalizated of clinical and biochemical parameters. Indicators for the cessation of sedative therapy serve to restore adequate external respiration, level of consciousness (for GCS above 12-13 points), reflexes against the background of improved controlled homeostasis systems (pCO2 = 40-45 mm Hg and blood pH = 7.36- 7.42).As a result of the use of the immunocorrective drug octagam in complex therapy in children with multiple organ failure, there was a decrease in the time spent in the intensive care unit by an average of 4.9 ± 2.1 bed / day, a decrease in the time spent on ALV by an average of 3.6 ± 0.5 days and a decrease in the mortality rate by an average of 6.6 ± 0.3% of the overall mortality rate.The efficiency of using octagam in multiple organ failure in children was also assessed on the basis of indicators of cellular and humoral immunity. There was a more rapid decrease of IL-6 levels which was regarded an early sign of therapy efficacy.
4. Conclusions
Laboratory indicators of dysfunction of the affected system are considered more informative for the detection of multiple organ failure in the early stages. Targeted testing of immune status in children with multiple organ failure makes it possible to identify early deviations in the body's adaptation systems. A decrease in the relative number of T-lymphocytes, T-helpers, an increase in the content of cytotoxic T-lymphocytes, an increase of B-lymphocytes number and a decrease in the level of immunoglobulins dictates the need to prescribe immunocorrective therapy to children with multiple organ failure. A decrease of IL-6 level against the background of intensive therapy was an early sign of therapy efficacy.Inclusion of Octagam in the complex therapy of children with multiple organ failure leads to an increase of initially reduced indicators of the immunity cellular link, stabilization of humoral immunity, promotes more rapid improvement of patients' condition.
References
| [1] | Alexandrovich K.S., Purmagambegova G.K., Piyunsov K.V. and others. Syndrome of multiple organ failure in newborns. Anesthesiology and resuscitation. 2008; 1: 11-15. |
| [2] | Tamburro R.F., Jenkins Tammara L. Multiple Organ Dysfunction Syndrome: A Challenge for the Pediatric Critical Care Community. Pediatr Crit Care Med. 2017; 18: 1-3. |
| [3] | Mironov P.I., Tsydenzhapov E.C. Scales for assessing the severity of the condition in children. Anesthesiology and resuscitation. 2008; 1: 4-7. |
| [4] | Carcillo JA., Podd B, Aneja R, Weiss SL, Hall MW. Pathophysiology of Pediatric Multiple Organ Dysfunction Syndrome. Pediatr Crit Care Med. 2017; 18: S32-S45. |
| [5] | Simbirtsev A.S. Cytokines: classification and biological functions. Cytokines and inflammation. 2004; 3 (2): 16-22. |
| [6] | Kallinen O., Maisniemi K., Bohling T. et al. Multiple organ failure as a cause of death in patients with severe burns. J Burn Care Res. 2012; 33: 206-212. |
| [7] | Fedicheva E.V., Dats A.V., Gorbacheva S.M. A manual for doctors / multiple organ failure syndrome (diagnosis, severity assessment, treatment and outcome prognosis): - Irkutsk: RIO IGIUV, 2009; 46. |
| [8] | Kallinen O., Maisniemi K., Bohling T. et al. Multiple organ failure as a cause of death in patients with severe burns. J Burn Care Res. 2012; 33: 206-212. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML