-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(8): 602-605
doi:10.5923/j.ajmms.20201008.14

Ultrasonographic Diagnostics by Choosing the Method of Surgical Treatment of the Habitual Dislocation of the Patella
Irismetov M. E., Rasulov M. R., Rustamova U. M., Ismatullaeva M. N.
Republican Specialized Scientific and Practical Medical Center of Traumatology and Orthopedics, Tashkent, Republic of Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The choice of the optimal method of surgical treatment of the habitual dislocation of the patella is one of the urgent problems of modern orthopedics. This is evidenced by the existence of more than 160 methods of operations. The ultrasound diagnostic method is non-invasive, affordable and quite informative, especially when choosing an operation. The article presents the results of ultrasound examinations to study the characteristic changes in the elements of the knee joint in this disease. A survey of 219 patients operated on using different methods was performed. According to the results of studies, it was found that ultrasonography is one of the methods for diagnosing the habitual dislocation of the patella, which provides the possibility of multiple dynamic studies and postoperative observation.
Keywords: Patella, Dislocation of the patellar ligament, Ultrasound diagnostics, Treatment
Cite this paper: Irismetov M. E., Rasulov M. R., Rustamova U. M., Ismatullaeva M. N., Ultrasonographic Diagnostics by Choosing the Method of Surgical Treatment of the Habitual Dislocation of the Patella, American Journal of Medicine and Medical Sciences, Vol. 10 No. 8, 2020, pp. 602-605. doi: 10.5923/j.ajmms.20201008.14.
Article Outline
1. Introduction
- Ultrasound examination remains one of the most accessible and reliable imaging methods in the diagnosis of injuries of intraarticular cartilage, tendons, ligaments and muscles (Vasilev А.U., Кlimova I.B., Shlyanak E.A., 2001). The reliability of this method in the study of the knee joint is 65–72% (Sautenko A.A., 2009). The advantage of ultrasound is the safety of the technique, relative simplicity, speed of execution, the ability to dynamically examine the structure of the knee joint. In case of instability of the patella, the state of the quadriceps muscle, the medial and lateral support apparatus are visualized using ultrasonography, and cartilage of the patella, condyles of the femur and tibia can be partially visualized (Maltseva L.V., Buravtsov P.P., 2013). According to Yeskina N.A. (2009), with the early stage of chondromalacia in the visual diagnosis of this pathology, ultrasonography has an advantage over other imaging methods. In addition, with instability, damage to the medial support device of the patella, its thickening, sagging, etc. are very well visualized.The most common damage to the ligamentous apparatus of the knee joint, after rupture of the anterior cruciate ligament, is a dislocation of the patella. The frequency of detection of patellar dislocation reaches up to 35%, which leads to the development of instability of the knee joint. This, in turn, leads to the appearance and progression of severe degenerative changes in the joint (Volokhovsky N.N., 2004; Gnelitsa N.N., 2009; Korolev A.V., 2000; Tuxoe I.J., Teir M., Winge S., Neilsen L.P., 2002). One of the factors in the development of a habitual dislocation is the lateral fastening of the patellar ligament in the tibial tuberosity region (Senavongse W., Amis A.A., 2005). Own ligament of the patella is considered a continuation of the tendon m. quadriceps femoris, which borders the patella and continues in the form of a lig. patellae proprium prior to attachment to tuberositas tibiae. Damage to the retinaculum medialis and medial segment of the patellar tendon, as well as the degree of lateralization to the site of attachment of the patellar tendon with tibial tuberosity, can lead to repeated patellar dislocation. During the examination, we were interested in the features of the patellar ligament at the site of its distal attachment to tuberositas tibiae and lig.patella-femoralis medialis. The state of these ligaments in the habitual dislocation of the patella with the description of their ultrasonographic semiotics was studied (Vatolin K.V., Shein V.N., Drozdov S.A., et al., 2012; Zubarev A.V., Gazhanova V.E., Dolgova I.V., 2003; Zubarev A.R., Nemenova N.A., 2006).Despite the notable successes achieved in the treatment of injuries of the knee joint, many unresolved issues remain in choosing a method of treatment and rehabilitation of the usual dislocation of the patella (Andrish J., 2004; Buravtsov P.P., Gorevanov E.A., 2006). The implementation of these tasks, including improving the anatomical and functional results of treating patients with habitual patellar dislocations by optimizing surgical methods depending on soft tissue damage to the medial surface of the patella and its own ligament, is one of the current trends in traumatology and orthopedics.The purpose of the work is to use the ultrasonographic studies to determine the condition of the soft tissues of the knee joint to select the method of operation with the usual dislocation of the patella.
2. Material and Research Methods
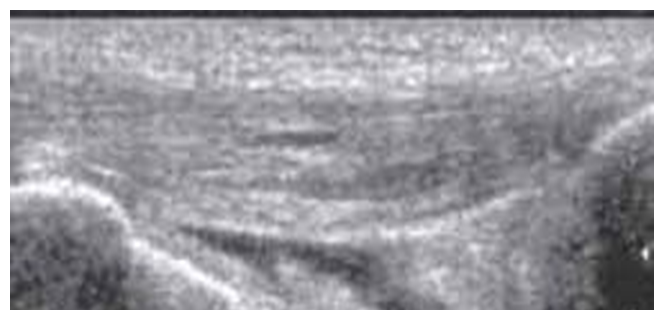
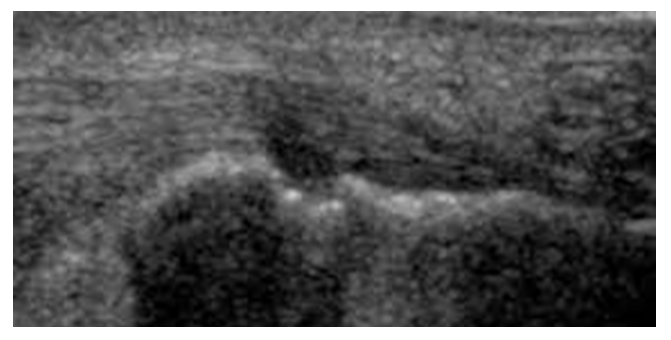
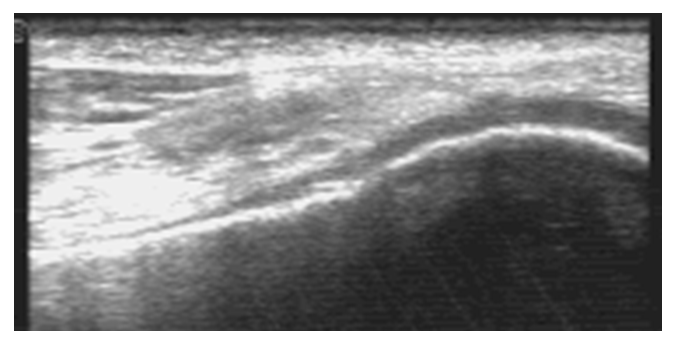
- From 2010 to the present, an ultrasonographic study of the knee joint in 219 operated patients with a habitual dislocation of the patella was performed at the Republican Specialized Scientific and Practical Medical Center for Traumatology and Orthopedics. During the examination, we used the MyLab 40 and MyLab X6 ultrasound equipment (Esaote, Italy) with multi-frequency sensors 7-12 and 6-12 MHz. Studies were performed in sagittal and transverse scans. In a sagittal sonographic examination, we easily determined our own ligament from the lower pole of the patella to the point of attachment to the tibial tuberosity. When using the program for panoramic study of the apparatus, the average ligament length reached 43 mm in the form of a linear hyper- and isoechoic structure. Sonographically, the ligament was identified as a linear isoechogenic structure with a transverse size in the range of 15-25 mm and anteroposterior size from 4 to 6 mm, with the presence of moderately hyperechoic contours. At the site of attachment to the tibial tuberosity, a slight expansion of the ligament size and a slight decrease in its echogenicity were noted. In a cross-sectional study, we visualized our own ligament in the form of point inclusions.We also studied the sonographic semiotics of the lateral and medial support apparatus of the patella. Visualization of it turned out to be somewhat more complicated due to the high anisotropy of the ligaments - Lig. patella-femoralis medialis, m. vastus medialis and retinaculum patella mediale et al. Lig. patella-femoralis medialis was visualized with fuzzy borders.
3. Results and Its Discussion
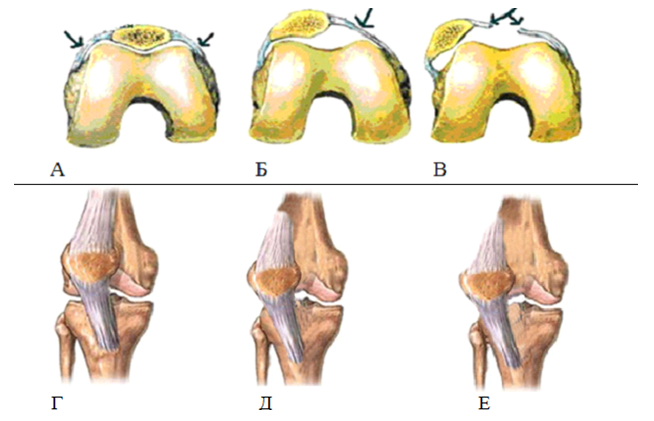
- In conducting clinical and ultrasonographic studies, we noted the importance of soft tissue structures of the medial surface of the patella - Lig. patella-femoralis medialis, m. vastus medialis and retinaculum patella mediale, because damage to these structures plays a big role in choosing a treatment method. Prior to surgery, Lig damage was detected. patella-femoralis medialis - in 98 (44.7%) patients; damage m. vastus medialis - in 76 (34.7%) patients; damage or defect of retinaculum patella mediale - in 45 (20.6%) patients.While maintaining the integrity of the medial patello-femoral ligament and isolated damage to the tendon stretch m. vastus medialis obliquus an important diagnostic method was ultrasonography. Clinical tests of the inclination and lateral displacement of the patella also made it possible to determine the need for surgical intervention on the lateral retinaculum, in case of chronic injuries. Since with prolonged lateral displacement of the patella, scarring of the latter occurs. Sonographically, this was revealed in the form of hyperechoic layers with uneven and fuzzy contours. Scarring leads to a limitation of the medial mobility of the patella and in some cases the impossibility of restoring the anatomical location of the patella in the intercondylar groove of the femur.Sonography was used to determine the degree of patellar displacement, depending on the degree of Lig damage. patella-femoralis medialis and own patellar ligament. Damage to the anatomical integrity of the ligament is determined depending on the sonographic picture as follows: the first degree - if part of the ligament fibers is torn, but the mechanical integrity is preserved, while a slight structural heterogeneity is revealed on the sonogram, the contours are even and clear, not crushed; the second degree - there is a rupture of the ligament with the presence of minor defects; the third degree is a complete gap in the bond with the presence of a noticeable defect (Fig. 1 a, b, c). Depending on the degree of damage to the ligaments, the severity of the patella displacement to the lateral side is observed.
 | Figure 1a. Damage to the ligament of the first degree. Moderate heterogeneity of the structure, the contours of the ligament are even and clear |
 | Figure 3. Schematic anatomical arrangement of the lig. patella-femoralis medialis |
4. Conclusions
- 1. Ultrasonographic examination is one of the important instrumental methods for the diagnosis of habitual dislocation of the patella and makes it possible to make a choice of treatment tactics.2. The advantages of the sonographic method include the possibility of multiple dynamic studies in the postoperative period.3. Timely diagnosis and the choice of rational surgical treatment of the usual dislocation of the patella in patients allows you to restore accurate relationships and stability in the patella-femoral joint and makes it possible to prevent or stop the development of patella-femoral osteoarthritis.4. The result of timely and reliable diagnosis of diseases and traumatic injuries of the musculoskeletal system is to improve the quality of life of the patient, reducing the risk of possible complications.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML