N. N. Sultonov, M. A. Sabirov, X. B. Barnoev
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The study evaluated the effectiveness of antiaggregant therapy in patients with chronic kidney disease. In the treatment of the disease, patients were divided into two groups, the first group was given alltrombosepin 200 mg/day as an antiaggregant treatment, and the second group was given dipyridamole 150 mg/day. The study was monitored for 30 days and followed by laboratory examinations and renal vascular dopplerography, and the following changes were obtained. In the first group, a maximal systolic velocity in the renal arteries was improved by 21.33%, a minimum diastolic velocity was improved by 24.16%, a decrease in RI-15.03%, and a decrease in PI-15.21%. In the second group after treatment, the maximum systolic velocity in the renal arteries improved by 23.14%, the minimum diastolic pressure by 22.64%, RI-15.29%, PI-15.18%. The results show that the plant-derived and locally produced allthrombosepin drug as an antiaggregant treatment in CKD has not been shown to be inferior to the dipyridamole drug used as a conventional treatment.
Keywords:
Chronic kidney disease, Renal hemodynamics, Antithrombotic treatment, Allthrombosepin, Dipyridamole
Cite this paper: N. N. Sultonov, M. A. Sabirov, X. B. Barnoev, Evaluation of the Effect of Antithrombotic Treatment on Intrarenal Hemodynamics in Chronic Kidney Disease, American Journal of Medicine and Medical Sciences, Vol. 10 No. 8, 2020, pp. 597-601. doi: 10.5923/j.ajmms.20201008.13.
1. Relevance of the Problem
Chronic kidney disease (CKD) is a global problem that is of interest not only to nephrologists, but also to cardiologists and neurologists. The medical and social significance of CKD in the world is determined by its growth, prevalence, complication with the development of terminal renal failure, as well as complications in the cardiovascular system and a high risk of developing them. [4]. Mortality from cardiovascular disease accounts for approximately 58% of deaths among patients in the dialysol phase of CKD. [5].The last decade has witnessed a pandemic of chronic kidney disease around the world. According to international epidemiological studies, the prevalence of CKD among adults in the United States, Western Europe, Australia, and China has increased from 11 to 16%. [3,6] and depending on the racial and other demographic characteristics of the population surveyed, 3-9.5% of the world’s population was found to have early stages of CKD, an increase of 15-20% or even 30% as the population ages. [5].Circulatory disturbances are noted in the early stages of CKD, and the frequency of decrease in glomerular filtration rate (GFR) <60 ml / min increases sharply. [1] Today, circulatory disorders in the kidneys alone do not cause impaired renal function in patients with CHF. In most cases, GFR is not significantly different in patients with CHF systolic dysfunction and in patients with preserved contractile function [6].Chronic kidney disease (CKD) has a negative effect on the remodeling of the vascular system, with the development of cardiorenal syndrome. Epidemiological studies suggest that injury to large humus arteries in patients with terminal renal failure is a risk factor influencing morbidity and mortality. [7]. In CKD, damage to blood vessels of various sizes not only affects the functional state of the kidneys, but also affects the cardiovascular system. This makes the disease more severe. To prevent these cases, we can contribute to reducing mortality and the number of patients with terminal renal failure by taking early diagnosis and treatment of CKD.Taking into account the above information, in order to improve blood circulation in the renal arteries and reduce vascular resistance, it was considered appropriate to study the effectiveness of antiaggregant drug produced in the Republic from local raw materials. The result of our research is the introduction of antiaggregant therapy in patients with CKD in the Republic through the use of low-cost antiaggregant drugs. This will lead to a reduction in costs from patients and our state financially. Such drugs include alltrombosepin, a herbal preparation based on the antiplatelet plant of the same name. Inhibits ADP-induced aggregation of platelets by inhibiting the activation of the GPIIb / IIIa (primary receptor for fibrinogen) complex by weakening the binding of ADP to platelet surface receptors. Alltrombosepin also attenuates platelet aggregation caused by other factors. Alltrombosepin affects ADP through irreversible changes in platelet receptors; normal aggregation activity is restored at a rate corresponding to the rate of formation of new platelets. From the first days of administration of allthrombosepin, inhibition of platelet aggregation occurs.
2. The Purpose of the Study
It consists of evaluating the effectiveness of antiaggregant therapy on the effect on intrarenal hemodynamics in patients with chronic renal disease.
3. Materials and Methods of Research
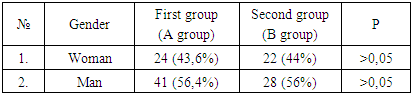
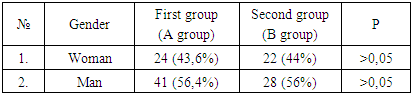
The research was performed on patients with chronic kidney disease of stage II-III of nondiabetic etiology in the nephrology department of the multidisciplinary clinic of the Tashkent Medical Academy, who were treated in 2018-2019. The total number of patients was 105. The patients were conditionally divided into two groups. The main (first) group (group A) included 55 patients, and alltrombosipin 200 mg/day was recommended in these patients as an antiaggregant treatment in combination with conventional therapy. The mean age of patients in the main group was 43.0 ± 1.65 years.The control group 2 (group B) included 50 patients who were given dipyridamole 150 mg/day as an antiaggregant treatment in combination with conventional therapy. The mean age of patients in this group was 44.3 ± 2.4 years. The age and sex distribution of the examined patient is given in Table 1.Table 1
 |
| |
|
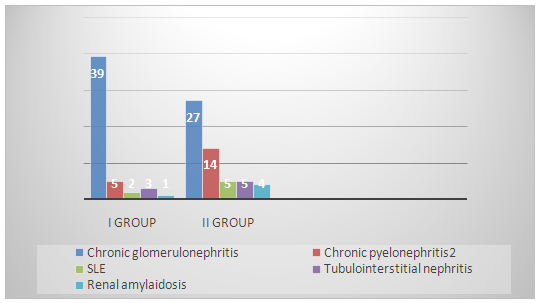
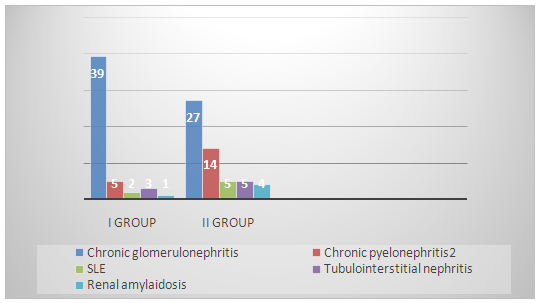
Table 1 shows that 24 (43.6%) of the main group of patients were women, 41 (56.4%) were men, 22 (44%) were women, and 28 (56%) were men.In both groups of patients, chronic kidney disease occurred as a complication of various diseases of nondiabetic etiology. The table below shows the proportion of major diseases caused by CKD in both groups of patients (Tab. 2)Table 2
 |
| |
|
All patients underwent laboratory and renal vascular dopplerography on the first day of treatment and 30 days after treatment. It was performed on the Sonoscape S20 Color Doppler Diagnostic Apparatus in the functional diagnostics department of the Multidisciplinary Clinic of the TMA.In the statistical processing of the results of the study obtained from the above two groups, the application software package of the personal computer "Statistica for Windows 7.0" was used. The arithmetic mean (M) was statistically calculated - this is an indicator of the central trend obtained by dividing the sum of all data values by the number of these data and was used to represent quantitative variables with a normal distribution. In our article, the data of the Arithmetic mean are presented in the form "M ± m", where m is the standard error of the mean (Standard Error of Mean), defined as follows: m = s / √n.
4. Results and It’s Discussion
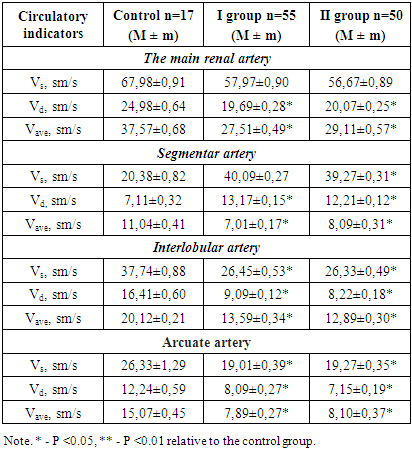
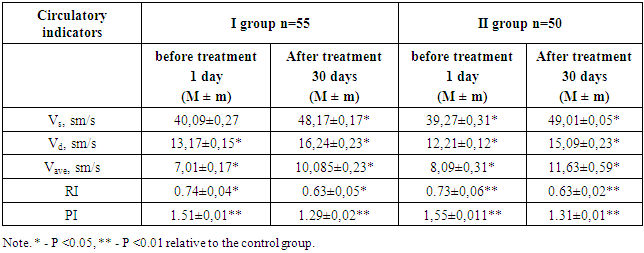
The study of the mechanisms of disease development in patients with chronic kidney disease presents some difficulties. Therefore, we studied the effect of hemodynamic changes on the development of CKD through the study of intrarenal hemodynamics. In the study, as an "indicator" of the pathological condition, we first studied the rate of blood flow and vascular resistance in the adrenal vessels: the main renal artery, segmentar, interlobular, arch arteries. In this study, hemodynamic changes in the kidneys were evaluated before treatment in all patients in our group. These results are given in Table 3.Table 3. Circulatory parameters in the main and intrarenal arteries of CKD (before treatment)
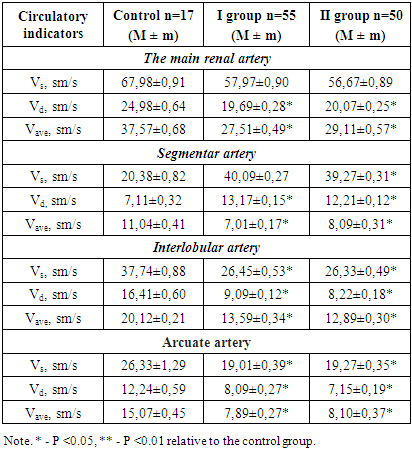 |
| |
|
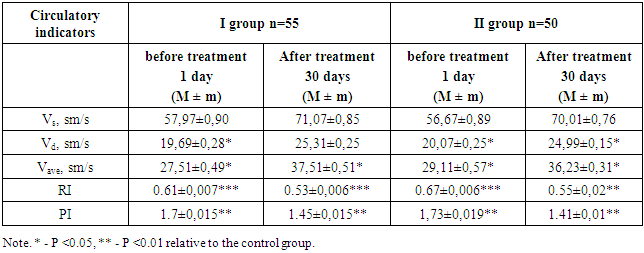
In the results presented in Table 3, the circulatory velocity in all renal arteries in the control group patients is within the normative range. However, in both control groups of patients with stage II-III CKD, we can see that the circulatory rate in the renal arteries is significantly lower than normal and vascular resistance is increased. The reason for this is the change in hemostasis in CKD. More precisely, the increase in platelet aggregation is due to the increase in vascular resistance. Taking into account these changes, patients with CKD stage II-III were given antiaggregant treatments and the dynamics of changes in renal arterial blood flow, vascular resistance were studied. When we studied the dynamics of changes in blood flow velocity and vascular resistance in the renal main artery before and after thirty days of treatment in both groups, we could see a significant improvement in results from day one to day thirty. (Table 4)Table 4. Indications for changes in circulatory velocity and peripheral resistance of the renal arteries in the main renal artery on the thirtieth day before and after treatment in CKD II-III stage
 |
| |
|
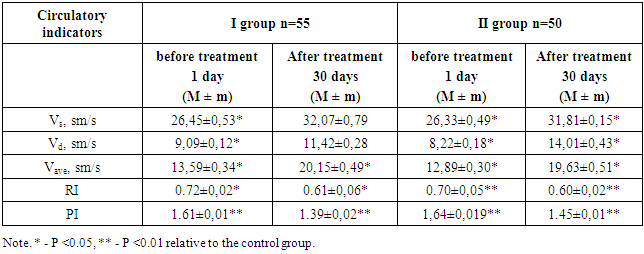
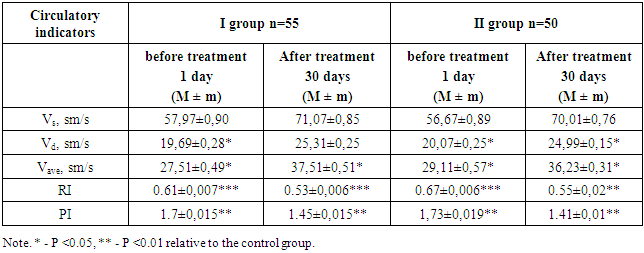
Based on the data in Table 4, it can be concluded that in our first group of patients the maximum systolic velocity in the main renal artery before treatment was 57.97 ± 0.90 cm / s, on the thirtieth day of treatment this indicator improved to 71.07 ± 0.85. It can be seen that a maximum systolic velocity of 22.59% was observed in the main renal artery. Minimal diastolic pressure improved by 28.54%. In our second group of patients, the maximum systolic velocity in the main renal artery before treatment was 56.67 ± 0.89 sm/s, while on the thirtieth day of treatment this figure improved to 70.01 ± 0.76 sm/s. In this group, a maximal systolic rate improvement of 23.53% was observed in the main renal artrery after thirty days of treatment. Minimal diastolic pressure improved by 24.51%.In determining the effectiveness of the effect of prescribed antiplatelet therapy on intrarenal hemodynamics, it is important for us to study the peripheral resistance of the renal arteries, ie RI and PI. In our first group, a 15% improvement in RI was observed during the thirty-day treatment, while a 17.42% improvement was observed in PI. In our second group, these indicators improved RI by 17.91% and PI by 18.49%.If we consider the circulatory rate and vascular resistance in the whole basin of the renal arteries in CKD, we can see the following changes in the segmentar arteries, which are located next to the main renal artery (Table 5).Table 5. Indications for changes in circulatory velocity and peripheral resistance in the renal segmentar artery in stage II-III of CKD (before and after treatment)
 |
| |
|
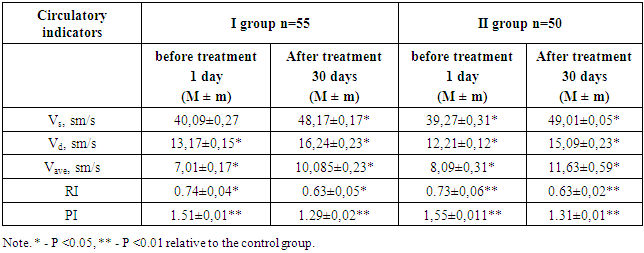
From the indicators given in Table 5 we can see the following changes. In our studies, the maximum maximal systolic velocity in segmentar arteries was increased by 20.15% and the minimum diastolic velocity by 23.31% during treatment. In this group, RI decreased by 14.86% and PI by 14.56%. In our second group of patients, the maximum maximal systolic velocity in the interstitial arteries was increased by 25.8%, and the final minimum diastolic pressure was increased by 23.58%. In this group, RI decreased by 13.69% and PI by 15.48%.In our observations in our groups, the dynamics of changes in blood flow velocity and vascular resistance in the renal interlobular artery before and after thirty days of antiaggregant treatment were studied.Observations have shown that the improvement of blood flow in the main renal artery and segmentar arteries during treatment has led to an improvement in these parameters in the interlobular vessels. All results are presented in Table 6.Table 6. Indications for changes in circulatory velocity and peripheral resistance in the renal interlobular artery on stage CKD II-III before and on the thirtieth day after treatment (M ± m)
 |
| |
|
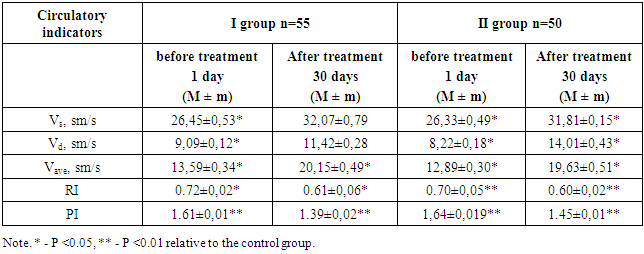
Analyzing the data presented in Table 6, the maximal systolic rate in the interlobular arterial basin was improved by 21.24% after thirty days of antiaggregant treatment, and the minimum diastolic rate was improved by 25.63%. In this group, RI decreased by 15.27% and PI by 13.66%. In our second group of patients, the final systolic rate in the interlobular artery basin was increased by 20.81% after thirty days of antiaggregant treatment, and the minimum diastolic rate was increased by 20.81%. RI decreased by 14.28% and PI by -11.58%.Based on the data in this Table 6, we conclude that CKD has led to improved blood flow in the renal main artery basin and a decrease in vascular resistance has also led to improved circulatory velocity in the adjacent vessels.As a result of the study, we found that the use of antiaggregant therapy in combination with traditional treatment for thirty days improved blood circulation in the renal main artery, segmentar and interlobular arteries, decreased vascular resistance, and in the arcuate artery. Improved blood flow velocity and decreased vascular resistance in the renal arteries led to improved metabolism in the renal arteries, improved renal function, and increased vascular filtration rate.From the results of the above research we can draw the following conclusions:1. In all patients with chronic kidney disease, from the main renal artery to the small arterioles, there is a decrease in blood flow and an increase in vascular resistance. This change in renal hemodynamics leads to a decrease in the functional state of the kidneys and a decrease in GFR.2. Based on the above changes and the results obtained, it is possible to understand the importance of antiaggregant treatment in patients with chronic kidney disease. Timely and appropriate administration of antiplatelet therapy in CKD leads to an improvement in the rate of circulation in the renal vessels by 20-25%, and a decrease in vascular resistance by 10-16%.3. In our study, the comparative efficacy of dipyridamole with allthrombosipin drugs produced in the Republic of Uzbekistan using dipyridamole, which is used as an antiaggregant therapy based on modern standards, is important.4. In the Republic of Uzbekistan, the addition of the antiaggregant allthrombosipin drug, made from local raw materials, to the standard of treatment as an antiaggregant treatment in CKDs has led to a functional state of the kidneys and provides material relief.
References
| [1] | Kutyrina I.A. Vascular remodeling in chronic renal failure. In the book: Nephrology. National leadership. Ed. On the. Mukhina. Moscow: GEOTAR-Media; 2009. S. 608–16. |
| [2] | Minasyan A.M., Sisakyan A.S. “Vascular remodeling in diseases of the kidneys as one of the factors for the development of cardiorenal syndrome” Medical Science of Armenia, National Academy of Sciences of Armenia, vol. LV No. 3 2015. |
| [3] | Nikolaev K.Yu., Nikolaeva A.A., et al. Pathogenesis of the development of chronic kidney failure in arterial hypertension. bulletin with the rams, Vol 32, No. 5, 2012, Articles 48–54. |
| [4] | Rogova I.V., Fomin V.V., Damulin I.V. et al. Vascular cognitive impairment in chronic kidney disease. Neurology, neuropsychiatry, psychosomatics. 2015; (1): 11–18. |
| [5] | Tomilina N.A., Bikhbov B.T., Antonova T.N. et al. On the question of the prevalence of chronic kidney disease in Moscow and its connection with cardiovascular pathology // Nephrology and Dialysis. 2009. 11. (4). 375-377. |
| [6] | Shutov A.M. Chronic kidney disease - a global problem of the XXI century // Clinical. the medicine. 2014. V. 92, No. 5. S. 5-10.]. |
| [7] | Xu R., Zhang L., Zhang P. et al. Comparison of the prevalence of chronic kidney disease among different ethnicities: Beijing CKD survey and American Nhanes // Nephrol. Dial Transplant 2009. 24. 1220-1226. |
| [8] | Oliver Königsbrügge, Sabine Schmaldienst, Martin Auinger, Renate Klauser-Braun, Cihan Ay Antithrombotic agents for primary and secondary prevention of cardiovascular events in patients with end-stage renal disease on chronic hemodialysis Atherosclerosis, Volume 298, April 2020, Pages 1-6. |
| [9] | Shoji Kawakami, Satoshi Yasuda, Hisao Ogawa Antithrombotic therapy in atrial fibrillation patients with coronary artery disease: shifting paradigm to a “less is more” concept regimen Journal of Cardiology, Volume 76, Issue 1, July 2020, Pages 35-43. |
| [10] | Toshiyuki Amano, Satoshi Matsuo, Yuichiro Miyamatsu, Sojiro Yamashita, Akira Nakamizo Impact of antithrombotic therapy on surgical treatment in patients with chronic subdural hematoma Journal of Clinical Neuroscience Volume 74, April 2020, Pages 55-60. |
| [11] | Robert C. Welsh, Eric D. Peterson, Raffaele De Caterina, Christoph Bode, John W. Eikelboom Applying contemporary antithrombotic therapy in the secondary prevention of chronic atherosclerotic cardiovascular disease American Heart Journal Volume 218, December 2019, Pages 100-109. |
| [12] | Behnood Bikdeli, Mahesh V. Madhavan, David Jimenez, Taylor Chuich, COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review Journal of the American College of Cardiology, Volume 75, Issue 2316, June 2020, Pages 2950-2973. |
| [13] | Sukhdeep S. Basra, Peter Tsai, Nasser M. Lakkis Safety and Efficacy of Antiplatelet and Antithrombotic Therapy in Acute Coronary Syndrome Patients With Chronic Kidney Disease Journal of the American College of Cardiology, Volume 58, Issue 2222, November 2011, Pages 2263-2269. |
| [14] | Ying Bai, Hui Chen, Yi Yang, Li Li, Chang-Sheng Ma Safety of antithrombotic drugs in patients with atrial fibrillation and non-end-stage chronic kidney disease: Meta-analysis and systematic review Thrombosis ResearchVolume 137, January 2016, Pages 46-52. |
| [15] | Anders Nissen Bonde, Gregory Y. H. Lip, Anne-Lise Kamper, Peter Riis Hansen, Jonas Bjerring Olesen Net Clinical Benefit of Antithrombotic Therapy in Patients With Atrial Fibrillation and Chronic Kidney Disease: A Nationwide Observational Cohort Study Journal of the American College of Cardiology, Volume 64, Issue 2316, December 2014, Pages 2471-2482. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML